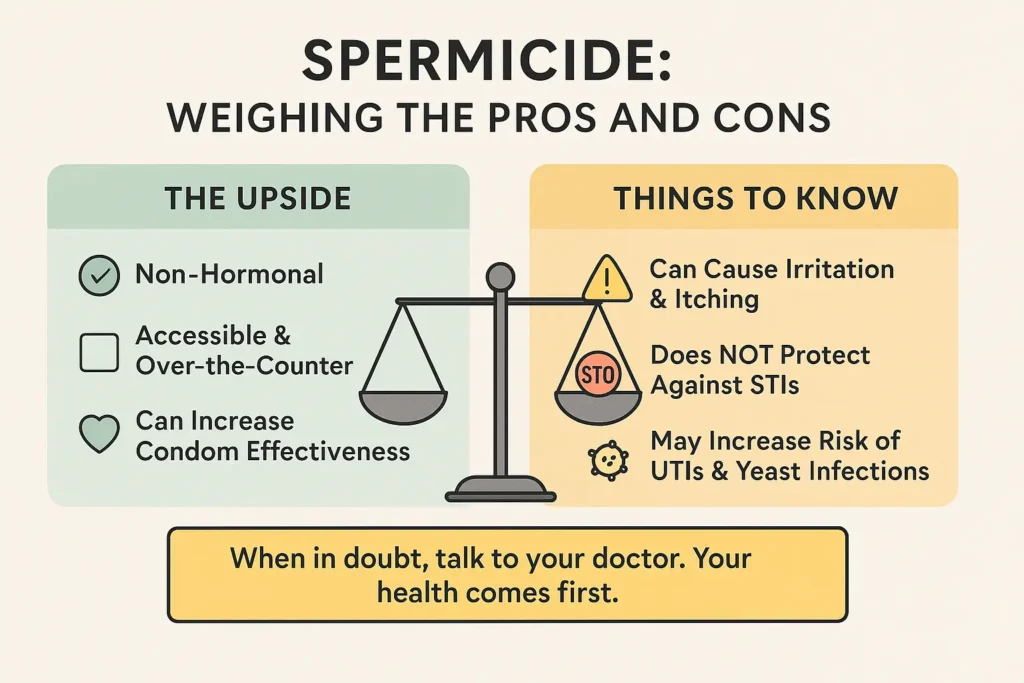
When it comes to birth control, having options is key. If you’re looking for a non-hormonal, accessible method that you can control, spermicide might be on your radar. But what exactly is it, and with different types like gels, films, and foams available, how do you choose?
This guide is here to clear up the confusion. We’re breaking down the 6 main types of spermicide, explaining exactly how to use each one, and outlining their pros and cons. By the end, you’ll have all the information you need to decide if spermicide is the right choice for you.
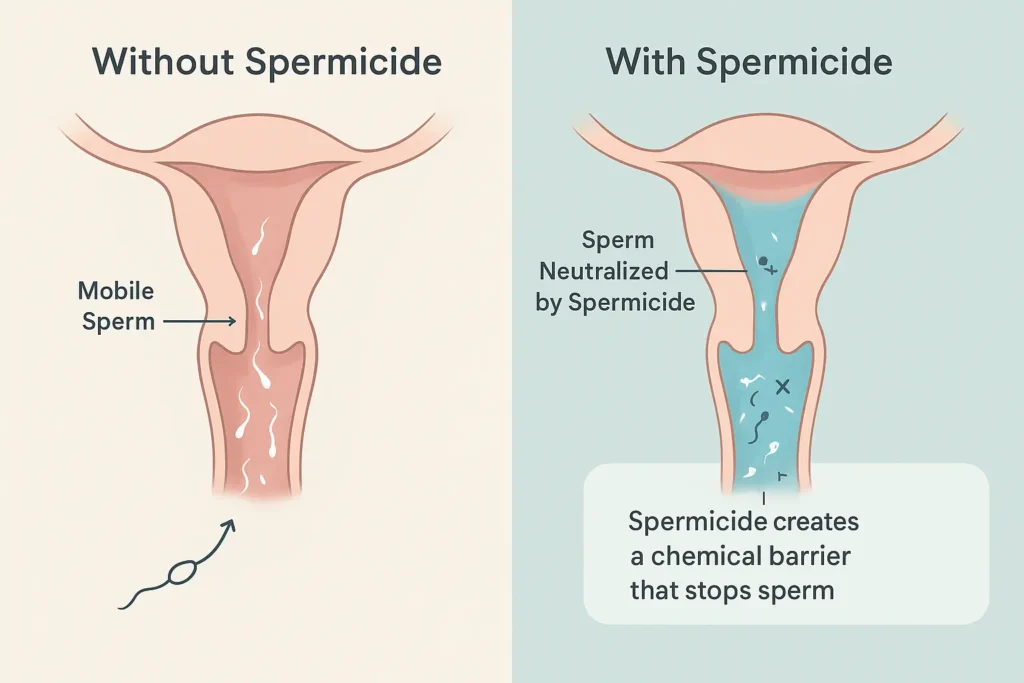
What is Spermicide and How Does It Work?
If you’re exploring non-hormonal birth control options, you’ve likely come across spermicide. But what exactly is it, and how does it prevent pregnancy on a biological level? Let’s break down the science in simple terms.
At its core, spermicide is a chemical contraceptive. Its sole purpose is to prevent pregnancy by stopping sperm in their tracks—literally. It does this through a one-two punch: first, it immobilizes sperm, making it impossible for them to swim, and second, it breaks down the sperm’s protective cell membrane, effectively killing them before they can reach and fertilize an egg.
The Active Ingredient: Nonoxynol-9 (N-9)
The vast majority of over-the-counter spermicides in the United States use a chemical compound called Nonoxynol-9 (N-9) as their active agent. Think of N-9 as a surfactant, similar to what you’d find in detergents. It works by disrupting the outer membrane of sperm cells, causing them to break down and lose their motility. This makes it impossible for them to navigate through the cervix to meet an egg.
A Critical Distinction: Spermicide Does NOT Prevent STIs
This is the most important point to understand about spermicide. It is not a reliable method for preventing sexually transmitted infections (STIs), including HIV.
In fact, the opposite can be true. Because N-9 can irritate and disrupt the delicate cellular lining of the vagina, frequent use can actually cause microscopic tears and inflammation. This breakdown of the body’s natural protective barrier can make it easier for pathogens like HIV, chlamydia, and gonorrhea to enter the bloodstream.
The Golden Rule: For protection against both pregnancy and STIs, spermicide should always be used in combination with condoms. Condoms provide a physical barrier that is highly effective against STIs, while the spermicide adds an powerful extra layer of defense against pregnancy.
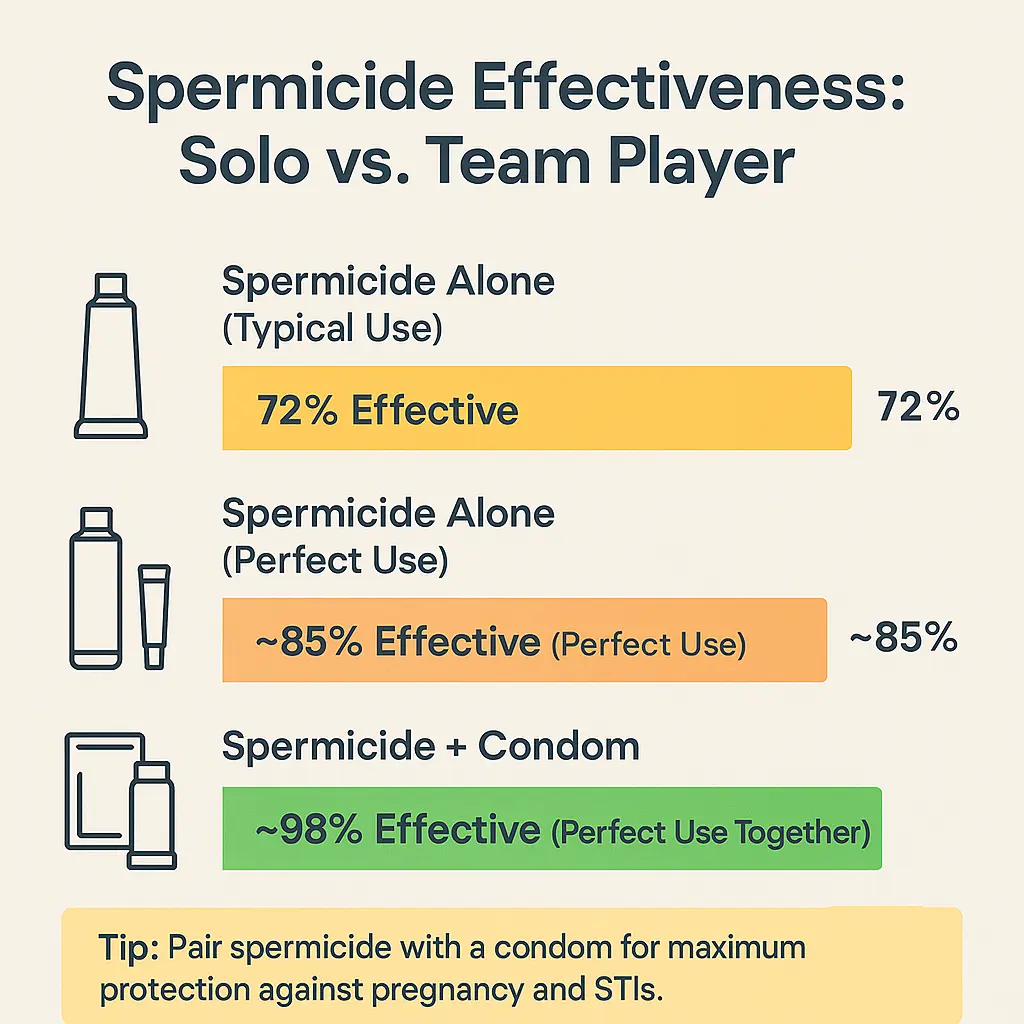
Understanding Spermicide Effectiveness
When choosing any birth control, understanding its real-world effectiveness is the most critical step. For spermicide, the key is to know the difference between “perfect use” and “typical use,” and more importantly, how to make it work for you.
The Reality of Typical Use: 72-82% Effective
On its own, with typical use over a year, spermicide is about 72% to 82% effective. Let’s put that into perspective:
- Typical Use (72% effective): This accounts for human error—applying it too late, not waiting for it to dissolve fully, missing a dose, or not placing it correctly. In this scenario, out of 100 people using only spermicide for a year, about 28 may become pregnant.
- Perfect Use (Approx. 85% effective): If used exactly as directed, every single time, the effectiveness rises to around 85%. This means about 15 out of 100 users may still become pregnant in a year. This “perfect use” rate is still lower than many other contraceptive methods, highlighting that its standalone power is limited.
Why isn’t it 100% even with perfect use? The chemical barrier is not impenetrable. A determined sperm that avoids contact with the spermicide, or a slight misplacement of the product, can be enough to result in pregnancy.
The Power of Pairing: Boosting Your Protection
The true strength of spermicide is revealed when you stop thinking of it as a solo act and start seeing it as the ultimate team player. Its effectiveness jumps significantly when used as a backup method with other forms of contraception.
This strategy is often called the “Pair and Protect” method. By combining two methods, you create multiple lines of defense, dramatically lowering the chance of pregnancy.
Powerful Combinations:
- Spermicide + Condoms: This is the gold standard for dual protection. Condoms provide a physical barrier against sperm and STIs, while spermicide acts as a chemical backup, disabling any sperm that might escape from a broken or slipped condom. This combination can be over 95% effective with perfect use.
- Spermicide + Diaphragm/Cervical Cap: These barrier devices are designed to be used with spermicide. The diaphragm or cap blocks the entrance to the cervix, and the spermicide coated on it neutralizes any sperm that get past the physical barrier.
The Bottom Line: While spermicide alone may not be the most reliable option for everyone, it transforms into a powerhouse of pregnancy prevention when paired with another method. For the best results, always use it as part of a combined strategy.
The 6 Types of Spermicide: A Detailed Breakdown
Let’s dive into the six primary forms of spermicide you’ll find at your local pharmacy or online.
1. Spermicidal Gel
Description: A thick, slippery, and transparent substance that comes in a tube with a special applicator.
- How to Use: You fill the applicator with the gel and insert it deep into the vagina, close to the cervix, similar to inserting a tampon. It’s important to do this within the time frame specified on the package, usually between 10 minutes and an hour before intercourse.
- Pros: Easy to apply with the provided applicator; provides lubrication.
- Cons: Can be messy and may leak out after sex.
2. Spermicidal Cream
Description: Very similar to gel but with a lighter, lotion-like consistency.
- How to Use: The method is identical to the gel, using an applicator for insertion. It’s also commonly used to coat the side of a diaphragm that rests against the cervix.
- Pros: Less thick and potentially less messy than some gels.
- Cons: May not stay in place as well as thicker formulations.
3. Spermicidal Foam
Description: A light, aerated, and shaving cream-like substance that comes in a canister.
- How to Use: You must shake the canister vigorously, then fill the applicator. The foam is inserted deep into the vagina near the cervix. The foam expands, helping to cover the cervical area.
- Pros: Expands for good coverage; less likely to leak than gels or creams.
- Cons: It can be difficult to tell if the applicator is full, and the consistency can vary.
4. Spermicidal Suppositories (Inserts)
Description: Small, solid, bullet-shaped or tablet-like inserts that you manually place into the vagina.
- How to Use: You unwrap a suppository and use your finger to insert it deep into the vagina. The critical step is waiting exactly as long as the instructions say—typically 10 to 15 minutes—for it to melt and become activated from your body heat.
- Pros: Very portable, discreet, and generally non-messy until they melt.
- Cons: Requires advance planning; if you don’t wait long enough, it won’t be effective.
5. Spermicidal Film (Vaginal Contraceptive Film – VCF)
Description: A thin, small, dissolvable square of paper that looks like a breath strip.
- How to Use: This method has a slight learning curve. You fold the film in half and use your finger to place it directly over your cervix. You must wait at least 15 minutes for it to dissolve and become a gel. Once dissolved, it’s effective for up to 3 hours.
- Pros: Extremely discreet, portable, and non-messy.
- Cons: Correct placement is crucial for effectiveness, and it requires a waiting period.
6. Spermicidal Sponge
Description: A soft, round, squishy polyurethane sponge that is pre-soaked in spermicide. It’s one of the more “all-in-one” barrier methods.
- How to Use: You wet the sponge with a small amount of water to activate the spermicide, then fold it and insert it deep into the vagina, ensuring the dimpled side covers your cervix. The sponge works for multiple acts of intercourse within a 24-hour period without needing to reapply spermicide. It must be left in place for at least 6 hours after the last intercourse.
- Pros: Provides continuous protection for 24 hours; can be used for multiple sessions.
- Cons: Can be difficult for some people to remove; some report a “foreign body” feeling.
Comparison Table: Spermicide Types at a Glance
| Type | Form | Ease of Use | Mess Factor | Waiting Time | Best For |
|---|---|---|---|---|---|
| Gel | Liquid | Easy (with applicator) | High | 10-60 min | Use with diaphragms |
| Cream | Lotion | Easy (with applicator) | Medium | 10-60 min | Use with diaphragms |
| Foam | Aerated | Moderate | Low | 10-60 min | Good cervical coverage |
| Suppository | Solid | Easy | Low (pre-melt) | 10-15 min | Discreetness, travel |
| Film | Dissolvable | Moderate (needs practice) | Very Low | 15 min | Spontaneity within a 3-hr window |
| Sponge | Sponge | Moderate | Low | None (after insertion) | Multiple acts, 24-hr protection |
How to Choose the Right Spermicide for You
With six different options available, selecting the right spermicide can feel overwhelming. But the choice becomes much simpler when you remember this golden rule: The “best” spermicide is the one that aligns with your lifestyle, your body, and your needs. It’s not about what’s most popular; it’s about what works most seamlessly for you.
To help you find your perfect match, ask yourself these key questions:
1. “How important is low mess to me?”
If the thought of leakage or a sticky feeling is a major turn-off, you’ll want to prioritize low-mess options.
- Your Best Bets: Spermicidal Film (VCF), Suppositories, and Foam.
- Why: The film and suppositories are solid until they dissolve inside the body, resulting in minimal leakage. Foam is lightweight and tends to be absorbed more easily than thicker formulas.
2. “How spontaneous are my intimate moments?”
If you prefer not to interrupt the moment, waiting 10-15 minutes for a product to activate can be a deal-breaker.
- Your Best Bet: The Spermicidal Sponge.
- Why: Once you insert the sponge, it provides continuous protection for up to 24 hours without needing to reapply. You can have sex multiple times without any additional waiting. (Note: Gels/creams/foams can also be inserted in advance, but their effective window is shorter than the sponge’s).
3. “Am I using it with another device, like a diaphragm?”
If you’re using a diaphragm or cervical cap, your choice is often directed by the device itself.
- Your Best Bets: Spermicidal Gel or Cream.
- Why: These thicker formulas are ideal for coating the rim and cup of a diaphragm, creating a secure seal and ensuring the spermicide stays in place right against the cervix. Always follow your doctor’s specific recommendation.
4. “Do I have sensitive skin?”
Irritation is the most common side effect of spermicides. If you’re prone to sensitivities, a proactive approach is key.
- Your Strategy:Conduct a Patch Test.
- How: Apply a small amount of the spermicide (a dab of gel or a piece of a dissolved film) to a sensitive area like your vulva or the inside of your elbow. Wait several hours to see if any redness, itching, or burning occurs.
- If you react: You might need to try a different brand or a formula without Nonoxynol-9 (N-9), though these are less common. This is also a strong reason to discuss alternatives with your healthcare provider.
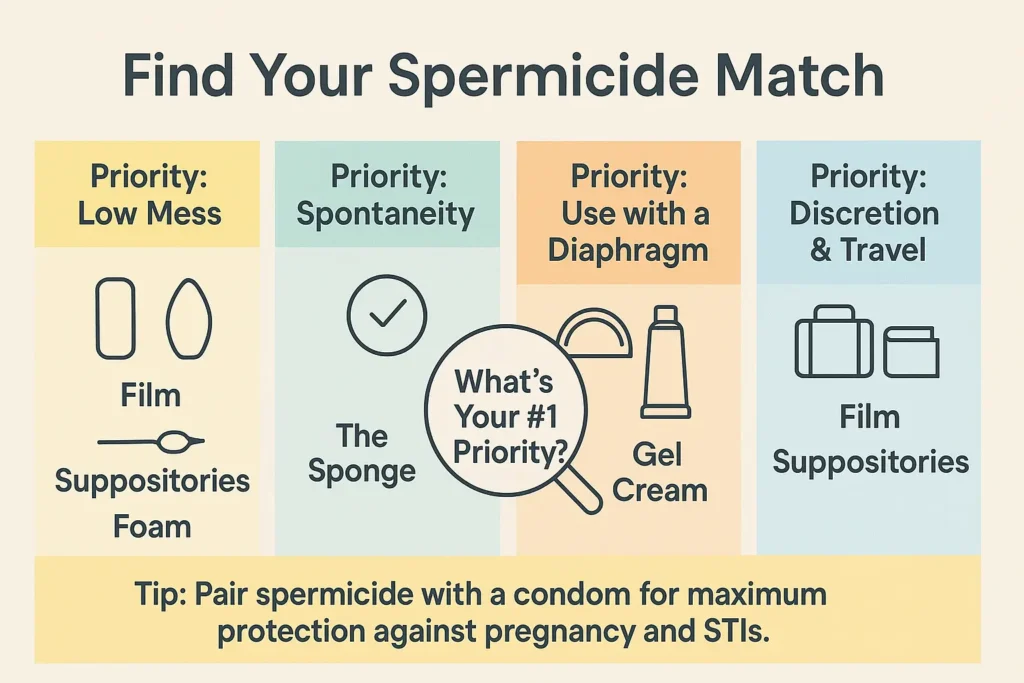
5. “What about discretion and portability?”
If you travel often or value a discreet product, some options are clearly better than others.
- Your Best Bets: Film and Suppositories.
- Why: These are small, silent, and look nothing like traditional birth control. A few film sheets or suppositories can easily be tucked into a wallet or small pouch without drawing any attention.
By listening to your body and honestly evaluating your lifestyle, you can move past the confusion and confidently choose a spermicide that feels less like a chore and more like a seamless part of your intimate health routine.
Important Considerations and Potential Side Effects
Knowledge is power, especially when it comes to your body. While spermicide is a safe and effective choice for many, being aware of its potential side effects and important health considerations is crucial for making an informed decision. Let’s walk through what you need to know before you use it.
Common Side Effects: What to Watch For
The most frequently reported side effects are localized, meaning they occur in the area of application for either partner.
- Local Irritation: This is the number one complaint. You or your partner might experience:
- Redness, itching, or a burning sensation in or around the vagina or penis.
- General discomfort or a “raw” feeling after use.
- This irritation is usually mild and tends to resolve on its own once you stop using the product.
- Increased Risk of Infections: This is a significant consideration. The active ingredient, Nonoxynol-9 (N-9), doesn’t just affect sperm; it can also disrupt the delicate balance of the vaginal flora—the good bacteria that keep yeast and harmful bacteria in check.
- Urinary Tract Infections (UTIs): Irritation near the urethra can make it easier for bacteria to cause an infection.
- Yeast Infections: By disrupting the natural pH and bacterial balance, spermicide can create an environment where yeast can overgrow.
- Bacterial Vaginosis (BV): Similar to yeast infections, the disruption in flora can also lead to BV.
The STI Risk: A Critical Warning
It’s vital to reiterate: Spermicide with N-9 does NOT protect against STIs and can actually increase your risk.
Here’s why: The chemical irritation that can cause microscopic tears in the vaginal or rectal tissue provides an entry point for viruses like HIV, herpes, and hepatitis. This is why spermicide is strongly discouraged for anyone at high risk of STIs or for use during anal sex.
When to See a Healthcare Provider
Consulting with your doctor or a gynecologist is a non-negotiable step before starting any new birth control, including over-the-counter options like spermicide.
Speak to your provider if:
- You have a history of frequent UTIs, yeast infections, or BV.
- You or your partner have known sensitivities or allergies to chemicals or cosmetics.
- You experience irritation that doesn’t clear up within a day or two after discontinuing use.
- You have any doubts or questions about whether it’s the right method for you.
They can help you understand if spermicide fits your health profile, recommend alternative products (like a different brand or a product without N-9, if available), and guide you on correct usage to minimize risks.
Performing a Patch Test: A Simple Precaution
If you’re concerned about sensitivity, a simple patch test can save you from significant discomfort later.
- Apply a small amount of the spermicide to a sensitive area like your inner forearm or vulva.
- Wait 24 hours to see if any redness, swelling, or itching develops.
- If you have a reaction, do not use the product intravaginally.
Making an empowered choice means weighing the benefits against the potential risks. By understanding these considerations, you can use spermicide safely and effectively, or make an informed decision to explore other options that better suit your body’s needs.
Frequently Asked Questions (FAQ)
How long does it take for spermicide to work?
It depends on the type. Suppositories and film require a 10-15 minute wait to melt. Gels, creams, and foams are typically effective immediately after insertion, but always check the package instructions.
How long does spermicide last?
Effectiveness varies. The sponge works for 24 hours. Film is effective for 3 hours once dissolved. Most other forms need to be reapplied for each act of intercourse.
Can spermicide cause birth defects?
Extensive research has shown that if you accidentally get pregnant while using spermicide, there is no increased risk of birth defects.
Can you use spermicide with condoms?
Yes! This is a highly effective combination. Using spermicide with condoms provides extra pregnancy prevention and peace of mind.
Where can I buy spermicide?
You can find most types of spermicide over-the-counter at pharmacies, grocery stores, and online retailers without a prescription.
Conclusion: Key Takeaways
Spermicide offers a valuable, non-hormonal option in the world of birth control. From the easy-to-apply gel to the discreet film and the long-lasting sponge, there are six main types to suit different needs and preferences.
Remember, while it’s a good method on its own, spermicide is most powerful when used as part of a team—especially with condoms. Your journey to finding the right birth control is personal. Use this guide as a starting point, talk to your healthcare provider, and choose the method that makes you feel most confident and in control.
Ressources
Authoritative Health Organizations
- The American College of Obstetricians and Gynecologists (ACOG)
- Link: www.acog.org/womens-health
- What you’ll find: A trusted resource from the leading group of women’s health care physicians. Search for “barrier methods of contraception” for detailed, physician-reviewed information.
- Planned Parenthood
- Link: www.plannedparenthood.org/learn/birth-control
- What you’ll find: Comprehensive, easy-to-understand guides on all birth control methods, including spermicide, with details on effectiveness, cost, and how to use them.
- The Centers for Disease Control and Prevention (CDC)
- Link: CDC Contraception Page
- What you’ll find: Official data on contraceptive effectiveness, usage statistics, and public health guidelines. Their “Contraceptive Guidance for Healthcare Providers” is the gold standard for effectiveness rates.
- The Office on Women’s Health (U.S. Department of Health & Human Services)
- Link: www.womenshealth.gov/a-z-topics/birth-control-methods
- What you’ll find: A reliable, government-run site that provides a broad overview of all birth control methods, including their pros and cons.
- Mayo Clinic
- Link: Mayo Clinic – Spermicide
- What you’ll find: A medically reviewed, in-depth look at spermicide, including how it works, risks, and what to expect.
Product Information & Manufacturer Websites
- Today Sponge
- Link: www.todaysponge.com
- What you’ll find: Detailed information on the spermicidal sponge, including how to use it, FAQs, and where to buy.
- VCF (Vaginal Contraceptive Film)
- Link: www.vcf.com
- What you’ll find: Information about the contraceptive film, usage videos, and a store locator.
Disclaimer: This blog post is intended for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for and should not be relied upon for professional medical advice. Always talk to your doctor, gynecologist, or another qualified healthcare provider about any questions you may have regarding a medical condition or birth control method.