What Happens During a Heart Attack Step-by-Step is a critical process that many people don’t fully understand.
Knowing the step-by-step progression of a heart attack can help you recognize early warning signs and take immediate action to save a life. From the initial artery blockage to the heart muscle damage, understanding each stage could make the difference between life and death.
In this article, you will learn:
- What happens inside your body during a heart attack step-by-step.
- The warning signs and symptoms that progress over time.
- How quick responses can reduce long-term heart damage.
Let’s explore the step-by-step process to better understand what happens during a heart attack.
What is a Heart Attack?
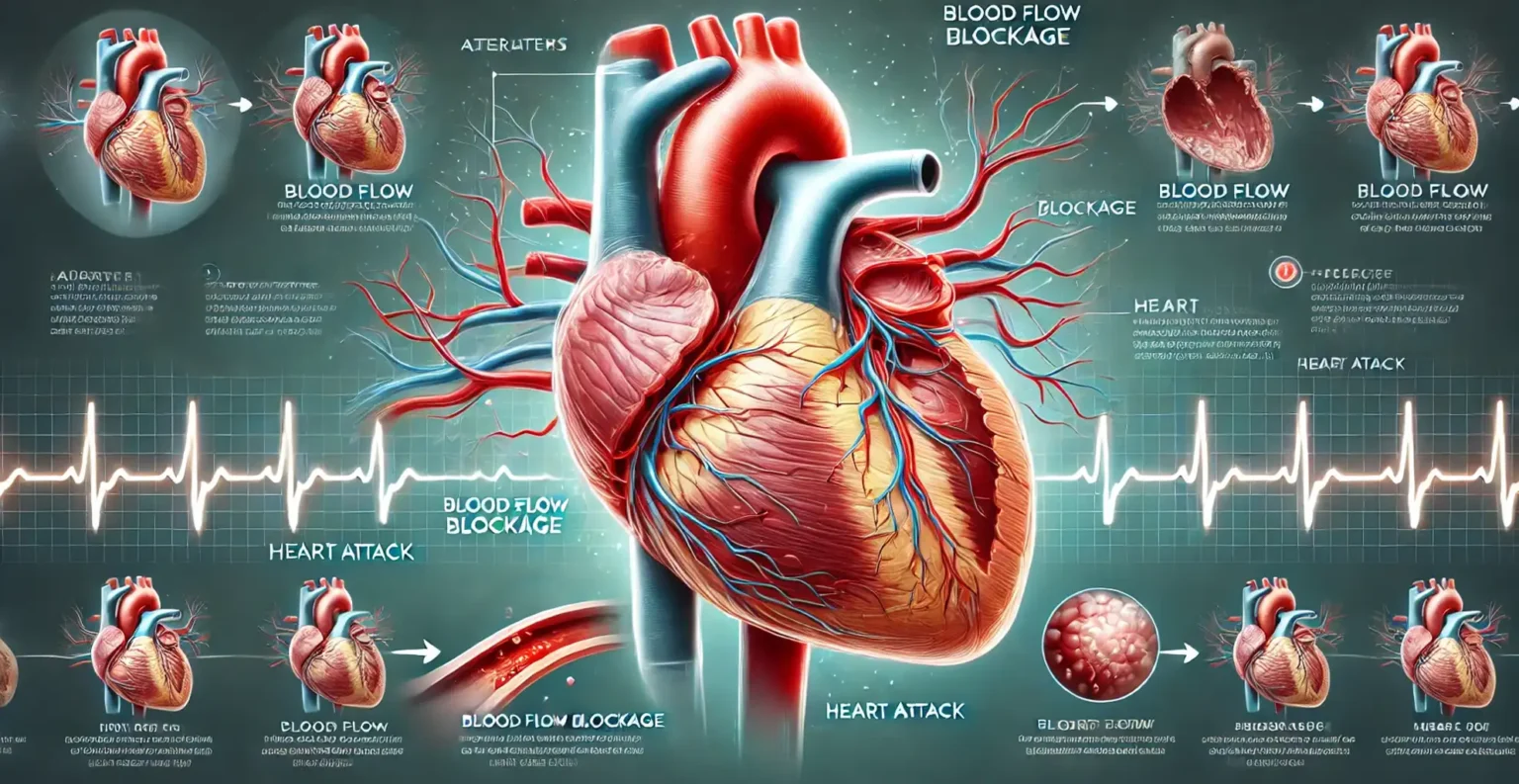
A heart attack, also known as a myocardial infarction, occurs when the blood supply to a part of the heart is suddenly and completely blocked. The heart, like every other muscle in the body, needs oxygen-rich blood to function. When that blood flow is cut off, even for a short time, the heart muscle begins to suffer damage. If the blockage isn’t removed quickly, parts of the heart muscle can die, leading to long-term complications or even death.
The blockage usually happens in the coronary arteries, which are the blood vessels that supply oxygen to the heart. Over time, these arteries can become narrowed due to the buildup of a waxy substance called plaque. Plaque is made of cholesterol, fats, and other substances in the bloodstream. This process is called atherosclerosis, and it can take years to develop without causing noticeable symptoms. However, when a piece of plaque suddenly breaks open (ruptures), the body reacts as if there’s an injury. It sends blood-clotting cells called platelets to the site, which can cause a clot to form inside the artery.

This clot can completely block the artery, stopping blood flow to a section of the heart muscle. Without blood flow, that part of the heart is deprived of oxygen, a condition known as ischemia. Within minutes, the affected heart cells start to die. The longer the blockage lasts, the more heart tissue is damaged, making quick treatment essential.
Heart attacks often happen without warning, but they are usually the result of years of damage to the arteries. In some cases, the heart may try to compensate by forming smaller blood vessels around the blockage, but this is rarely enough to prevent a heart attack. If left untreated, the damage can be permanent, increasing the risk of heart failure, irregular heart rhythms, or sudden cardiac arrest.
The key to surviving a heart attack is immediate medical intervention. Treatments like clot-busting medications and emergency procedures, such as angioplasty (which reopens blocked arteries), can restore blood flow and minimize damage to the heart muscle. Every minute matters because the heart muscle starts to die within 10-15 minutes of a complete blockage. Acting quickly not only saves the heart but can also reduce the risk of life-threatening complications.
Understanding what happens during a heart attack step-by-step is critical to recognizing the signs early and seeking help immediately. The sooner blood flow is restored, the better the chances of survival and recovery.
The Step-by-Step Process of a Heart Attack
A heart attack doesn’t happen all at once — it’s a step-by-step process that unfolds in a matter of minutes to hours. Understanding how a heart attack progresses can help you recognize symptoms early and take life-saving action.
Step 1: Plaque Buildup and Blockage Begins
The process of a heart attack often begins years before the event with plaque buildup in the coronary arteries. This plaque is made up of cholesterol, fats, calcium, and other substances that stick to the walls of the arteries. Over time, the buildup causes the arteries to narrow, a condition known as atherosclerosis.
At some point, the plaque can become unstable and rupture, causing a crack or tear in the artery wall. The body sees this rupture as an injury and tries to repair it by sending platelets (blood-clotting cells) to the site. However, instead of helping, this response forms a blood clot that can partially or completely block the artery, stopping blood flow to the heart.
Step 2: Blood Flow Gets Blocked
Once the blood clot forms, it can completely block the flow of oxygen-rich blood to a section of the heart. The heart muscle depends on a steady supply of oxygen to function, and without it, the affected area quickly begins to suffer.
It takes just 10 to 15 minutes for the lack of oxygen to start damaging the heart tissue. This condition is known as ischemia, which means the heart muscle is starving for oxygen. If the blockage isn’t cleared quickly, the damage will continue to spread, increasing the risk of long-term complications or death.
Step 3: The Heart Muscle Begins to Die
Without blood flow, heart muscle cells in the affected area begin to die. This process is called myocardial infarction, and it typically begins in the innermost layer of the heart muscle. The damage then spreads outward to other layers if blood flow isn’t restored in time.
Heart cells are highly sensitive to oxygen deprivation, and once they die, they cannot regenerate. The longer the blockage remains, the larger the area of dead tissue becomes. This is why immediate medical intervention is critical — treatments like clot-busting medications and angioplasty can stop the damage from spreading if administered quickly.
Step 4: Symptoms Intensify (Recognizing the Signs)
As the heart attack progresses, classic symptoms begin to appear. The most well-known symptom is chest pain or discomfort, often described as a squeezing, pressure-like sensation. This pain may spread to the arms, neck, jaw, or back. Other common symptoms include:
- Shortness of breath
- Nausea or vomiting
- Cold sweats
- Dizziness or lightheadedness
However, symptoms can vary significantly between individuals. For example, women may experience less chest pain and more subtle symptoms such as fatigue, indigestion, or back pain. People with diabetes or older adults may have “silent heart attacks” with very mild or no symptoms at all. Recognizing these variations is crucial to ensuring timely medical care.
Step 5: The Heart Tries to Compensate
During a heart attack, the heart tries to compensate for the damage. If part of the heart muscle is weakened, the heart may try to pump harder to maintain blood flow. This extra strain can cause the heart to beat irregularly, a condition called arrhythmia.
In some cases, the irregular heartbeat can become dangerous, leading to ventricular fibrillation, where the heart quivers instead of pumping blood. This can result in sudden cardiac arrest, where the heart stops beating altogether. Without immediate defibrillation or CPR, cardiac arrest can be fatal within minutes.
The heart’s ability to compensate is limited, which is why immediate treatment is essential. The faster blood flow is restored, the better the chances of minimizing damage and preventing life-threatening complications.
How to Respond to a Heart Attack
A heart attack is a medical emergency, and knowing how to respond quickly can be the difference between life and death. Immediate action is critical to restore blood flow to the heart and prevent severe damage. In this section, we’ll explore step-by-step actions to take if you or someone else shows signs of a heart attack and why early intervention is key.

Recognize the Symptoms and Act Fast
The first step in responding to a heart attack is recognizing the warning signs. Common symptoms include chest pain or discomfort, shortness of breath, nausea, sweating, dizziness, and pain in the arms, neck, jaw, or back. If any of these symptoms appear — even if they seem mild or come and go — treat it as a heart attack until proven otherwise.
If you or someone else is experiencing these symptoms:
- Stop all activity and sit or lie down immediately. This reduces the strain on the heart.
- Take a deep breath to stay calm. Anxiety can worsen the situation by raising heart rate and blood pressure.
Next, take immediate action to seek help.
Call Emergency Services Immediately
The most important thing you can do during a heart attack is call emergency services (like 911). Time is critical — don’t waste valuable minutes debating whether symptoms are serious. The quicker medical professionals arrive, the better the chances of survival and recovery.
When calling emergency services, be prepared to provide:
- Your location
- A description of symptoms
- The person’s medical history, if known
Why call an ambulance instead of driving to the hospital?
- Paramedics can begin life-saving treatments immediately. They have the tools and medications to treat heart attacks on the way to the hospital.
- Ambulances are equipped with defibrillators to restart the heart in case of cardiac arrest.
- Time matters. Driving yourself or someone else delays medical care if the condition worsens en route.
Life-Saving Treatments: CPR and Defibrillation
In some cases, a heart attack can lead to sudden cardiac arrest, where the heart stops beating altogether. In these situations, CPR (cardiopulmonary resuscitation) and defibrillation are essential life-saving interventions.
CPR (Cardiopulmonary Resuscitation)
CPR is a manual technique used to keep blood flowing to the brain and vital organs when the heart has stopped. If someone collapses, is unresponsive, and stops breathing, start CPR immediately while waiting for emergency services to arrive.
Here’s how to perform hands-only CPR:
- Place your hands in the center of the person’s chest.
- Push hard and fast at a rate of 100-120 compressions per minute.
- Don’t stop until medical help arrives or the person starts to respond.
Even if you’re not trained in CPR, hands-only CPR can keep the person alive by circulating oxygenated blood to the brain and heart until professionals take over.
Defibrillation (Using an AED)
An automated external defibrillator (AED) is a portable device that can deliver an electric shock to the heart to restore a normal rhythm. Many public places, such as airports, schools, and gyms, have AEDs on hand.
If an AED is available:
- Turn on the device and follow the instructions.
- Attach the pads to the person’s chest as shown in the diagram on the AED.
- Let the AED analyze the heart rhythm and deliver a shock if needed.
Defibrillation is especially important in cases of ventricular fibrillation, a deadly arrhythmia that often occurs during cardiac arrest. Every minute without defibrillation reduces the chances of survival by about 10%.
What NOT to Do During a Heart Attack
While taking quick action is essential, there are a few common mistakes to avoid:
- Don’t ignore symptoms. Many people dismiss early heart attack symptoms as indigestion or fatigue.
- Don’t drive yourself to the hospital. You could lose consciousness while driving, endangering yourself and others.
- Don’t wait to see if symptoms improve. Every minute of delay increases the risk of severe damage or death.
The Importance of Acting Fast
When a heart attack happens, every minute counts. The sooner blood flow is restored, the less damage occurs to the heart muscle. Treatments like angioplasty (to reopen blocked arteries) and clot-busting medications are time-sensitive and work best when administered quickly.
By recognizing the signs of a heart attack, calling emergency services immediately, and performing CPR or using an AED if necessary, you can save a life. Quick action improves the chances of survival and reduces the risk of long-term heart damage.
Preventing a Heart Attack
Heart attacks can happen suddenly, but the underlying causes often develop over time due to lifestyle choices and genetic factors. While some risk factors like age and family history can’t be changed, many others are within your control. Taking proactive steps to maintain heart health can significantly reduce your chances of experiencing a heart attack. In this section, we’ll explore lifestyle changes, stress management techniques, and the importance of regular medical check-ups.
Adopt a Heart-Healthy Lifestyle
One of the most effective ways to prevent a heart attack is by making sustainable lifestyle changes. These adjustments can improve your heart health, lower blood pressure, reduce cholesterol, and help maintain a healthy weight. Below are key areas to focus on:
1. Eat a Heart-Healthy Diet
What you eat directly impacts your heart health. A heart-healthy diet is rich in:
- Fruits and vegetables: Provide essential vitamins, minerals, and antioxidants.
- Whole grains: Help reduce bad cholesterol and maintain healthy blood pressure.
- Lean proteins: Choose options like fish, poultry, beans, and legumes.
- Healthy fats: Incorporate nuts, seeds, and olive oil instead of saturated fats.
At the same time, limit or avoid unhealthy foods that can contribute to artery blockages:
- Processed foods
- Sugary drinks and snacks
- Trans fats and saturated fats
- Excess salt
A Mediterranean-style diet, which emphasizes whole foods and healthy fats, is often recommended for improving heart health.
2. Exercise Regularly
Physical activity is crucial for keeping your heart strong and your blood vessels healthy. Aim for at least 150 minutes of moderate-intensity exercise per week, such as:
- Brisk walking
- Cycling
- Swimming
- Aerobic exercises
Regular exercise helps:
- Lower blood pressure
- Improve cholesterol levels
- Manage body weight
Even small changes, like taking the stairs instead of the elevator or walking during breaks, can make a big difference. The goal is to keep your heart active and improve overall circulation.
3. Manage Stress
Chronic stress can take a toll on your heart by raising blood pressure and causing unhealthy coping behaviors, such as overeating or smoking. Learning to manage stress is a crucial part of preventing heart disease.
Consider incorporating the following stress-reduction techniques into your daily routine:
- Meditation or mindfulness practices
- Deep breathing exercises
- Yoga or tai chi
- Spending time outdoors or engaging in hobbies
Managing stress helps regulate your heart rate, lowers cortisol levels (the stress hormone), and reduces the risk of developing high blood pressure or heart disease.
4. Quit Smoking and Limit Alcohol Consumption
Smoking is one of the leading causes of heart disease. It damages blood vessels, raises blood pressure, and reduces oxygen levels in the blood, increasing the risk of a heart attack. Quitting smoking is one of the most impactful changes you can make for your heart health.
Similarly, limit alcohol intake to reduce blood pressure and avoid contributing to weight gain. Excessive alcohol can cause heart rhythm problems and damage the heart muscle over time.
The Importance of Regular Check-Ups
While lifestyle changes are essential, regular check-ups with your doctor are equally important for preventing a heart attack. Many risk factors, such as high blood pressure, high cholesterol, and diabetes, have no noticeable symptoms until damage is already occurring. Regular screenings can help catch these conditions early and allow you to manage them before they become serious.
During your check-ups, your doctor will likely monitor:
- Blood pressure: High blood pressure is a major risk factor for heart attacks.
- Cholesterol levels: Too much LDL (bad cholesterol) can contribute to artery blockages.
- Blood sugar levels: Diabetes increases the risk of heart disease and heart attacks.
These routine screenings can identify risks and help you take corrective action before a heart attack occurs.
Know Your Family History
Your genetics play a significant role in determining your heart attack risk. If your parents, siblings, or other close relatives have a history of heart disease or heart attacks, your risk may be higher. It’s important to inform your doctor about your family history so they can adjust your care plan accordingly.
Having a family history of heart disease doesn’t mean you’re destined to have a heart attack, but it does mean you should be extra vigilant about lifestyle changes and medical screenings. Being proactive can help offset genetic risk factors.
The Power of Prevention: Small Changes Make a Big Difference
Preventing a heart attack is about building lifelong habits. Small, consistent changes — like swapping unhealthy snacks for fruits, adding a 20-minute walk to your day, or practicing mindfulness — can have a massive impact on your heart health over time. By combining a healthy lifestyle with regular medical check-ups and an awareness of your genetic risks, you can reduce your chances of experiencing a heart attack and improve your quality of life.
In heart health, prevention is always better than cure. The steps you take today can protect your heart for years to come.
Heart Attack Prevention and Response
Here are some frequently asked questions about heart attacks to provide additional clarity on this critical topic.
1. How can I tell if I’m having a heart attack?
The most common signs of a heart attack include:
- Chest pain or discomfort (feeling of pressure, squeezing, or fullness)
- Pain in the arms, neck, jaw, or back
- Shortness of breath
- Nausea, dizziness, or cold sweats
If you experience any of these symptoms, call emergency services immediately.
2. Can a heart attack be prevented?
Yes, heart attacks can often be prevented through lifestyle changes and medical check-ups. Eating a heart-healthy diet, exercising regularly, managing stress, quitting smoking, and limiting alcohol intake are key preventive measures. Regular screenings for blood pressure, cholesterol, and blood sugar levels are also crucial.
3. What should I do if someone is having a heart attack?
Follow these steps:
- Call emergency services immediately.
- If the person is unconscious and not breathing, start CPR.
- Use an automated external defibrillator (AED) if available.
- Keep the person calm and still until help arrives.
4. Can women have different heart attack symptoms than men?
Yes, women may experience more subtle symptoms, such as:
- Fatigue
- Nausea or indigestion
- Pain in the back, neck, or jaw
They may also have less noticeable chest pain compared to men. Recognizing these differences is essential for early detection.
5. How long does it take for heart muscle damage to occur during a heart attack?
Heart muscle damage can begin within 10-15 minutes after blood flow is blocked. The longer the blockage remains, the more extensive the damage. This is why immediate treatment is critical.
6. Is there a difference between cardiac arrest and a heart attack?
Yes.
- Heart attack occurs when blood flow to the heart is blocked.
- Cardiac arrest happens when the heart stops beating altogether due to electrical issues.
A heart attack can lead to cardiac arrest if not treated quickly.
7. What are the best ways to reduce stress to prevent a heart attack?
Some effective stress-reduction techniques include:
- Meditation and mindfulness practices
- Regular physical activity
- Deep breathing exercises
- Spending time outdoors
- Getting enough sleep
Conclusion: What Happens During a Heart Attack Step-by-Step
Understanding what happens during a heart attack step-by-step is crucial for recognizing symptoms early, responding effectively in an emergency, and taking preventive measures to protect your heart health. From the initial plaque buildup in the arteries to the life-saving treatments like CPR and defibrillation, every minute counts when a heart attack strikes.
Let’s recap the key takeaways from this article:
- A heart attack happens when blood flow to the heart is blocked, causing heart muscle damage.
- Recognizing the symptoms and responding quickly with emergency services and CPR can save lives.
- Prevention through lifestyle changes and regular check-ups is the best way to reduce your risk.
Preventing a heart attack starts with the small choices you make daily — eating healthy, exercising, managing stress, and getting regular check-ups. These actions, combined with knowledge of heart attack warning signs, can dramatically improve your heart health and increase your chances of a long, healthy life.
Next, consider learning about heart attack recovery and life after a cardiac event to prepare for what comes next after surviving a heart attack. Understanding the recovery process can help you or a loved one manage long-term heart health successfully.