Facing the reality of cancer can be deeply unsettling. In an age of information overload, the sheer volume of conflicting advice about prevention and causes often amplifies fear rather than providing clarity.
This article is a calm space for understanding. We are dedicated to uncovering The Truth About Cancer by turning to clinical research and established science, not headlines or myths. Here, we replace confusion with a clear, evidence-based framework.
By focusing on what the data actually tells us about risk, prevention, and early signs, this guide empowers you with knowledge. Our aim is to provide you with a trustworthy foundation, helping you move from anxiety to informed awareness and actionable steps.
What Is Cancer, and How Does It Develop in the Body?
At its core, cancer is not a single disease but a collection of related diseases characterized by one fundamental, shared principle: the uncontrolled growth and spread of abnormal cells. Think of it as a breakdown in the meticulous rules that govern how our bodies renew and repair themselves. Normally, our tissues maintain a careful balance. Cancer occurs when this balance is lost, and a group of cells begins to ignore the body’s signals to stop dividing, die when damaged, or stay in their designated place.
The Biological Foundation: From Normal Cell to Cancer Cell
Your body is an intricate community of roughly 37 trillion cells. In healthy tissue, these cells follow a strict life cycle: they grow, divide to create new cells when needed, and eventually die through a programmed process called apoptosis. This elegant system is regulated by an intricate set of genes, which act like a blueprint and a command center.
Cancer begins when genetic changes (mutations) disrupt this orderly cycle. These mutations can be:
- Inherited: Passed down from a parent (accounting for a small percentage of cancers).
- Acquired: Developed over a lifetime due to:
- Environmental factors: Such as exposure to tobacco smoke, ultraviolet radiation, or certain chemicals.
- Lifestyle factors: Like chronic poor diet or alcohol consumption.
- Random errors: Simple mistakes that happen naturally when a cell copies its DNA during division—a significant and unavoidable source of mutation.
The Multi-Step Journey: Carcinogenesis
The development of cancer, a process called carcinogenesis, is typically not instantaneous. It is a slow, multi-stage journey that can unfold over years or even decades, often without any symptoms. This progression can be understood in three key stages:
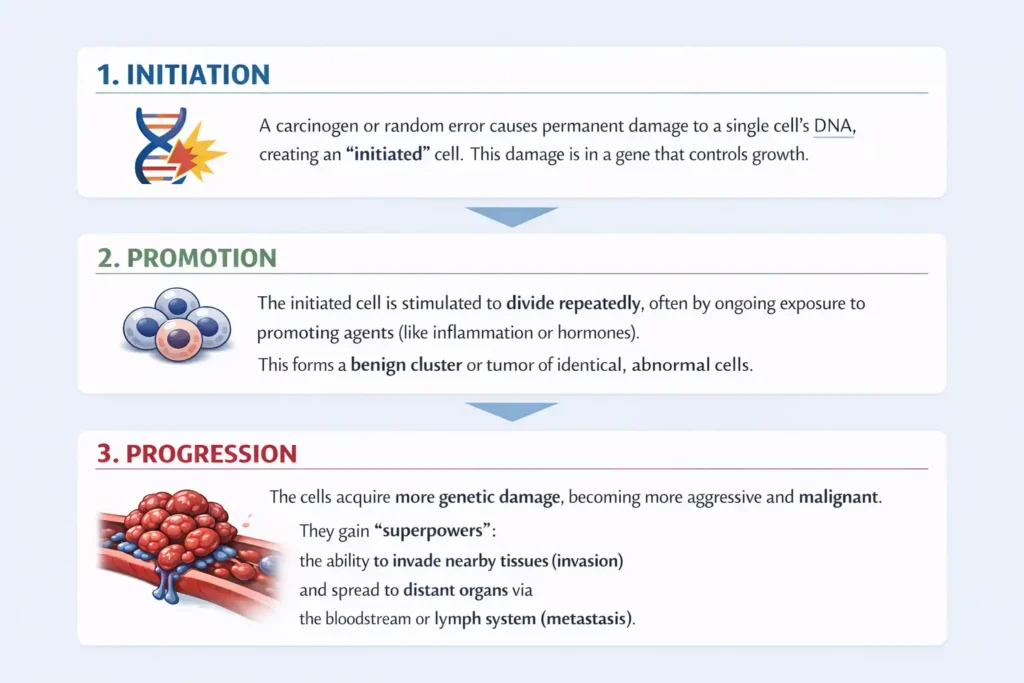
1. Initiation: The journey starts when a carcinogen (e.g., chemicals in tobacco, UV rays) or a random copying error causes permanent damage to the DNA of a single cell. This mutation is often in a gene that controls cell growth or repair. The cell is now “initiated,” but it is not yet cancerous.
2. Promotion: The initiated cell sits dormant until it is stimulated to divide repeatedly. This promotion can be driven by ongoing exposures—such as chronic inflammation, certain hormones, or additional lifestyle factors—that encourage growth. These repeated divisions create a mass or cluster of identical, abnormal cells. This stage can last a long time and may even be reversible if the promoting factors are removed.
3. Progression: Eventually, these dividing cells acquire more genetic mutations. They become more aggressive, unstable, and genetically diverse. They may develop the hallmarks of cancer: they can evade the immune system, create their own blood supply (angiogenesis), and, critically, gain the ability to invade surrounding healthy tissues and metastasize—break away, travel through the blood or lymph, and form new tumors in distant organs.
Cancer Is Not One Single Event: The “Multiple Hit” Model
It’s crucial to understand that cancer is rarely the result of one mistake or one exposure. The “multiple hit” model explains that a series of genetic “hits” or mutations is required to transform a normal cell into a cancerous one. This is why:
- Risk increases with age: We have more time to accumulate these genetic hits.
- Prevention is powerful: Reducing cumulative exposure to damaging agents (like quitting smoking, protecting skin from sun) directly reduces the number of potential “hits” on our cells over a lifetime.
- Not everyone exposed gets cancer: An individual’s risk depends on the complex interplay of their genetics, their total lifetime exposures, and a degree of random chance in cellular processes.
This foundational understanding empowers us. By knowing that cancer development is a prolonged, multi-factor process, we can see the genuine value in long-term, evidence-based prevention strategies that work to minimize these damaging “hits” and support our body’s innate defense systems.
Cancer Myths vs. Scientific Facts: Separating Fiction from Evidence
Misinformation about cancer isn’t just confusing—it can be harmful, leading to unnecessary fear, false hope, or the dismissal of effective prevention and treatment. In an era of viral claims and “miracle cure” anecdotes, turning to the steady voice of scientific consensus is more important than ever. This section examines some of the most persistent cancer myths and contrasts them with the clear, evidence-based facts, empowering you to navigate health information with critical thinking and confidence.
Debunking Common Cancer Misconceptions
The table below addresses four widespread myths with clarity, citing sources like the World Health Organization (WHO) and the American Cancer Society to ground each fact in established research.
| Myth | Scientific Fact & Evidence |
|---|---|
| “Cancer is a modern, man-made disease.” | Cancer has existed throughout history. Paleopathologists have found evidence of tumors in Egyptian mummies and fossilized bones. While modern lifestyles and environmental exposures (like processed foods and pollution) influence today’s risk rates, the disease itself is ancient. Our longer lifespans and better diagnostic tools also make cancer more visible now. |
| “Superfoods like blueberries or broccoli can cure cancer.” | No single food can cure cancer. However, a diet rich in a variety of fruits, vegetables, and whole grains is consistently associated with a reduced risk of developing certain cancers. These foods contain beneficial compounds (e.g., antioxidants, fiber) that support overall health and may help protect cells from damage, but they are part of a broader protective pattern, not magic bullets. |
| “Cancer treatments are often worse than the disease.” | While treatments like chemotherapy and radiation have significant, well-documented side effects, their use is based on a rigorous, personalized risk-benefit analysis. For many cancers, modern, evidence-based protocols have dramatically improved survival rates and quality of life. Supportive care has also advanced greatly to manage side effects effectively. |
| “If no one in my family has cancer, I won’t get it.” | Only about 5-10% of cancers are strongly hereditary. The vast majority are “sporadic,” caused by a complex interplay of lifestyle, environment, and random genetic mutations acquired during one’s lifetime. This is why screening based on age and personal risk factors, not just family history, is critical. |
The “Bad Luck” Myth: A Closer Look
A particularly nuanced and persistent idea is that cancer is “just bad luck.” This myth stems from influential research (like the 2017 study in Science) that quantified the role of random errors in DNA replication as a key factor in cancer risk. It’s true that random chance plays a role—we cannot predict which specific cell might have a copying error.
However, interpreting this as “prevention is futile” is a dangerous and scientifically inaccurate conclusion. As the World Health Organization (WHO) emphasizes, a large proportion (an estimated 30-50%) of cancers are linked to modifiable risk factors. This means our daily choices and environments substantially increase or decrease the probability of those random errors occurring or progressing.
Think of it like rolling dice: “Bad luck” determines if a specific roll shows a high-risk number. But lifestyle and cancer risk factors determine how many times you roll the dice in the first place. Smoking, poor diet, and sun exposure add more “rolls,” significantly increasing the odds over a lifetime. Therefore, evidence-based cancer prevention is powerfully effective at the population and individual level, even as we acknowledge an element of randomness.
Evidence-Based Risk Factors: Genetics, Lifestyle, and Environment
Understanding cancer risk is less about a single cause and more about understanding a personal risk profile—the unique combination of factors each person accumulates over a lifetime. Scientific research consistently groups these influences into three interconnected categories: Genetic, Lifestyle, and Environmental. By mapping these factors, we can see where our greatest opportunities for evidence-based cancer prevention truly lie.
The following visual summarizes how these three categories interact to influence overall risk:
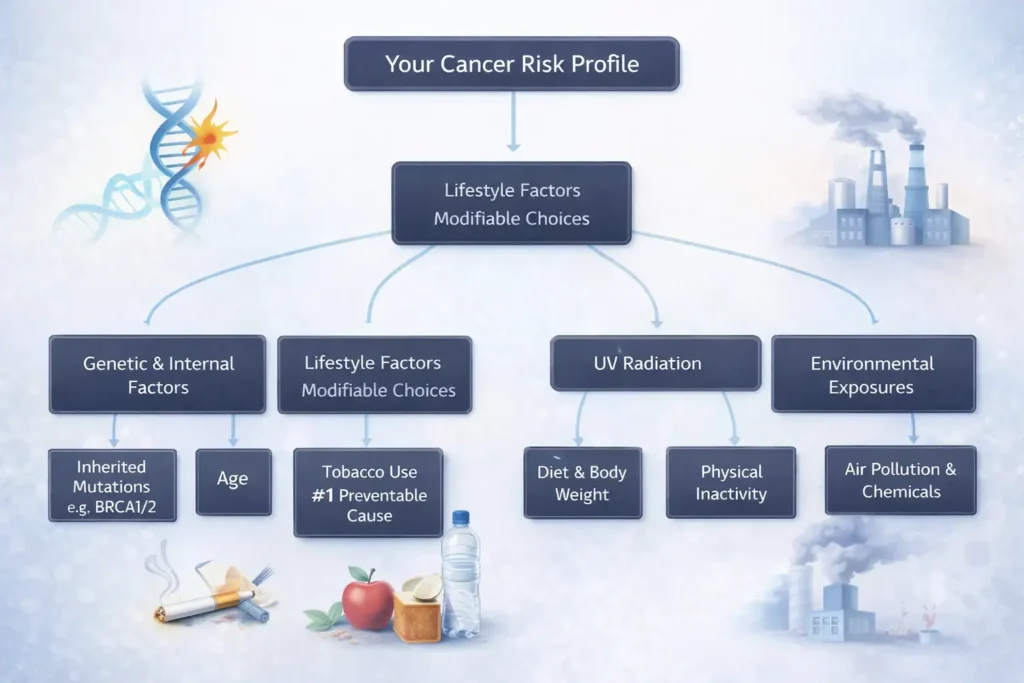
1. Genetic and Internal Factors (The Foundation You Inherit)
These are factors we are born with or that are intrinsic to our biology. While we cannot change them, understanding their role provides crucial context for our personal health picture.
- Inherited Mutations: Specific gene variants passed from parent to child can significantly increase risk. For example, mutations in the BRCA1 and BRCA2 genes substantially raise the lifetime risk of breast, ovarian, and other cancers. However, it’s vital to remember that these strongly hereditary factors account for only about 5-10% of all cancers.
- Age: This is the single most significant risk factor for most cancers. The risk rises dramatically as we age, primarily because accumulating years provide more time for cellular damage to build up and for the body’s repair mechanisms to become less efficient. According to the National Cancer Institute (NCI), the median age of a cancer diagnosis is 66 years.
- Immune Function: Our immune system constantly patrols for and eliminates abnormal cells. Individuals with chronically suppressed immune systems—due to conditions like HIV/AIDS, autoimmune diseases, or immunosuppressive medications after an organ transplant—have a higher risk of developing certain cancers, particularly those caused by viruses.
2. Lifestyle Factors (Your Powerful Levers for Prevention)
This category represents the most substantial area where individual choices can directly and significantly alter cancer risk. This is the core of actionable, evidence-based cancer prevention.
- Tobacco Use: Remains the leading cause of preventable cancer death globally. The Centers for Disease Control and Prevention (CDC) states that tobacco smoke, with its 7,000+ chemicals, is causally linked to cancers of the lung, mouth, throat, pancreas, bladder, and at least 10 other organs. There is no safe level of exposure.
- Diet and Body Weight: The synergy between diet and weight is critical. The World Cancer Research Fund (WCRF) concludes that maintaining a healthy weight is one of the most important steps you can take to reduce cancer risk. Excess body fat can promote inflammation and alter levels of hormones like insulin and estrogen, which can stimulate cancer growth. Diets high in processed meats (like bacon and sausage) and low in fruits, vegetables, and whole fibers are consistently associated with higher risks, particularly for colorectal cancer.
- Physical Inactivity: Regular activity works independently to lower risk. It helps regulate hormones, reduces inflammation, improves immune function, and aids in maintaining a healthy weight. For example, robust evidence shows that regular physical activity lowers the risk of colon, breast, and endometrial cancers.
- Alcohol Consumption: Alcohol is a recognized Group 1 carcinogen. When the body metabolizes alcohol, it produces acetaldehyde, a chemical that damages DNA. Even moderate consumption increases risk, with the danger rising with the amount consumed. Cancers linked to alcohol include those of the breast, liver, esophagus, and head and neck.
3. Environmental and Occupational Exposures (The World Around Us)
These are carcinogens we encounter in our physical surroundings, often in the air, water, or workplace.
- Ultraviolet (UV) Radiation: From the sun and artificial tanning devices, UV radiation directly damages the DNA in skin cells. This cumulative damage is the primary cause of most skin cancers, including melanoma, the deadliest form. Prevention is straightforward: seek shade, wear protective clothing, and use broad-spectrum sunscreen.
- Infectious Agents: Several viruses and bacteria are established biological carcinogens. Persistent infection with high-risk Human Papillomavirus (HPV) is responsible for nearly all cervical cancers and is linked to cancers of the oropharynx, anus, and genitals. Similarly, chronic Helicobacter pylori infection is a major cause of stomach cancer. Vaccination (HPV) and treatment (H. pylori) are powerful preventive tools.
- Air Pollution and Chemical Exposures: The International Agency for Research on Cancer (IARC) classifies outdoor air pollution (specifically fine particulate matter) as a Group 1 carcinogen, linked to lung cancer. Occupational exposures to substances like asbestos, benzene, and certain industrial chemicals also carry established risks, highlighting the importance of workplace safety regulations.
Understanding this triad of factors empowers you to focus on what you can control—primarily lifestyle choices—while being informed about the factors you monitor, like family history and age-appropriate screenings. It moves the conversation from one of fear to one of informed personal agency.
Early Signs of Cancer Explained: The Critical Importance of Awareness
Cancer is most treatable when found early. While screening tests are designed to detect cancer in asymptomatic individuals, being attuned to your body’s signals provides a crucial second layer of defense. Awareness of potential early signs of cancer empowers you to partner with your doctor proactively. It is essential to remember that these symptoms are far more often caused by benign conditions than cancer. However, recognizing them and seeking timely evaluation is a key principle of early detection.
Common General Warning Signs: The “CAUTION” Framework
The American Cancer Society’s well-established CAUTION acronym provides a memorable checklist for changes that warrant a conversation with a healthcare professional. The operative word is change from your personal norm, and the critical qualifier is persistent or unexplained.
- Change in bowel or bladder habits: This includes persistent constipation or diarrhea, changes in stool caliber (e.g., pencil-thin stools), a feeling of incomplete emptying, or increased frequency/urgency of urination. Blood in the stool or urine is a particularly important sign that should never be ignored. For a deeper look at one key area, our guide to digestive warning signs explores these symptoms further.
- A sore that does not heal: A persistent sore in the mouth, on the skin, or in the genital area that does not heal over several weeks.
- Unusual bleeding or discharge: This includes coughing up blood, unusual vaginal bleeding or discharge, bloody discharge from the nipple, or blood in vomit.
- Thickening or lump in the breast or elsewhere: Any new, painless lump or area of thickening in the breast, testicle, lymph nodes (armpit, neck, groin), or soft tissues. Breast changes also include dimpling, puckering, or changes to the nipple.
- Indigestion or difficulty swallowing (dysphagia): Persistent indigestion or heartburn not linked to a known dietary cause, or a sensation of food getting stuck when swallowing.
- Obvious change in a wart or mole: Any change in size, shape, color, or border of a skin lesion, or the development of a new, atypical-looking mole (following the ABCDE rules of melanoma).
- Nagging cough or hoarseness: A cough that lasts for more than a few weeks without an obvious cause, or persistent hoarseness of the voice.
Additional General Signs: Unexplained weight loss (10+ pounds without trying), persistent and unexplained fatigue that doesn’t improve with rest, and persistent, low-grade fever can also be associated with some cancers.
Why Screening Saves Lives: The Proactive Approach
Screening is the systematic use of tests to find cancer in people who have no symptoms whatsoever. Its power lies in intercepting cancer at its earliest, most treatable stages, often before it has spread. The decision to recommend a population-wide screening test is based on rigorous evidence that the benefits (lives saved) outweigh the potential harms (like false positives or overdiagnosis).
Key Evidence-Based Screening Tests
The following are recommended for average-risk individuals at specific ages:
| Cancer Type | Screening Test | General Recommendation (for Average Risk) |
|---|---|---|
| Breast Cancer | Mammography | Women, starting at age 40-50, repeated every 1-2 years. |
| Cervical Cancer | Pap Test & HPV Test | Women, starting at age 21-25. Pap tests every 3 years, or co-testing (Pap + HPV) every 5 years from age 30. |
| Colorectal Cancer | Colonoscopy, Stool Tests | Adults, starting at age 45. Colonoscopy every 10 years, or annual high-sensitivity stool tests. |
| Lung Cancer | Low-Dose CT (LDCT) Scan | Adults aged 50-80 with a significant smoking history (current or former). |
Creating a Personalized Screening Plan
Your individual plan should be developed in partnership with your doctor, considering:
- Personal Risk Factors: Your lifestyle, medical history, and known environmental exposures.
- Family History: A strong family history of certain cancers may prompt earlier or more frequent screening.
- Overall Health & Life Expectancy: Screening recommendations may change based on other health conditions.
Understanding the Limitations
Informed participation in screening means understanding its nuances:
- False Positives: A result that suggests cancer when none is present. This can lead to anxiety and follow-up tests but is part of ensuring nothing is missed.
- False Negatives: A test result that appears normal even though cancer is present. No test is 100% sensitive.
- Overdiagnosis: The detection of very slow-growing cancers that may never have caused harm in a person’s lifetime. This is a complex topic, especially in screenings for prostate and some breast cancers.
The most effective strategy combines being aware of your body’s signals (like the CAUTION signs) with participating in evidence-based screening appropriate for your age and risk. This dual approach maximizes the chances of early detection, when treatment options are most numerous and successful.
Prevention: What Does Science Actually Support?
TrWhen it comes to cancer, the concept of prevention is often misunderstood. It is not about finding a single “magic bullet” or guaranteeing absolute immunity. Rather, true cancer prevention is about risk reduction—consciously stacking the odds in your favor through decades of proven science. It involves separating impactful, evidence-based actions from well-marketed but unproven trends. By focusing on factors within our control, we can make meaningful strides in evidence-based cancer prevention.
Primary Prevention: Reducing the Risk of Cancer Developing
Primary prevention refers to actions taken to avoid the initial development of cancer. These strategies target the modifiable risk factors we have direct influence over, forming the cornerstone of a proactive health approach.
The following evidence-based strategies are widely recognized by global health authorities like the World Health Organization (WHO) and the World Cancer Research Fund (WCRF) as having the strongest impact on reducing overall cancer risk:
| Prevention Strategy | Scientific Rationale & Key Action |
|---|---|
| 1. Do Not Use Tobacco | Tobacco in any form (smoked, smokeless,二手烟) is the world’s leading preventable cause of cancer. Quitting at any age provides immediate and long-term risk reduction for at least 15 different cancers. |
| 2. Maintain a Healthy Weight | Excess body fat promotes chronic inflammation and alters levels of hormones like insulin and estrogen, which can stimulate cancer cell growth. Aim for a sustainable weight within a healthy BMI range. |
| 3. Move Regularly | Physical activity helps regulate hormones, reduces inflammation, and improves immune function independently of weight. Aim for at least 150 min of moderate exercise (e.g., brisk walking) per week. |
| 4. Eat a Balanced Diet | Prioritize whole foods: fill half your plate with a variety of colorful fruits and vegetables, choose whole grains, and include legumes. Limit processed meats and sugary drinks. |
| 5. Limit Alcohol | For cancer prevention, there is no completely risk-free level. If you drink, limit to ≤1 drink/day for women, ≤2 for men. Less is always better from a cancer-risk perspective. |
| 6. Protect Your Skin | UV radiation from the sun and tanning beds is a direct DNA mutagen. Use broad-spectrum SPF 30+ sunscreen daily, seek shade, and wear protective clothing and hats. |
| 7. Get Vaccinated | Vaccines are powerful primary prevention tools. The HPV vaccine prevents cancers caused by the human papillomavirus (cervical, oropharyngeal). The Hepatitis B vaccine prevents liver cancer. |
| 8. Avoid Carcinogen Exposure | This includes practicing safe sex to reduce viral exposure, not sharing needles, and being aware of occupational hazards (e.g., asbestos, certain industrial chemicals). |

Secondary Prevention: Stopping Cancer Early
If primary prevention aims to stop cancer before it starts, secondary prevention aims to stop it in its earliest, most treatable stages. This involves surveillance and intervention for precancerous conditions or early-stage disease in asymptomatic individuals.
- Adherence to Screening Guidelines: This is the most critical component. Participating in evidence-based cancer screening according to your age and risk profile (e.g., colonoscopy, mammography, Pap/HPV tests) can detect precancerous polyps or early-stage cancers, often allowing for simpler, more curative treatments. Screening is a direct application of the knowledge that early signs of cancer explained by medicine are often invisible to us.
- Management of Precancerous Conditions: This is medical intervention to halt progression. Examples include:
- Removing colorectal polyps during a colonoscopy to prevent them from turning into cancer.
- Treating a chronic Helicobacter pylori infection to prevent gastric (stomach) cancer.
- Monitoring and treating Barrett’s esophagus to prevent esophageal adenocarcinoma.
- Genetic Counseling and Testing: For individuals with a strong family history, genetic testing can identify inherited mutations (like BRCA). This allows for tailored, enhanced surveillance (e.g., earlier or more frequent MRIs) or risk-reducing surgeries, which are considered very effective secondary prevention measures.
The Power of Synergy
It’s vital to understand that these strategies are not isolated. They work synergistically. For example, regular physical activity (primary prevention) helps maintain a healthy weight, which in turn lowers the risk of cancers like colorectal cancer. Similarly, getting a colonoscopy (secondary prevention) can both detect and prevent cancer by removing polyps.
Science supports a layered, consistent approach. By integrating these primary and secondary prevention strategies into your life and healthcare plan, you are actively engaging in the most powerful, evidence-based defense against cancer we currently possess.
Deeper Learning Resources
Understanding cancer can feel overwhelming, but knowledge is the foundation of empowerment. While this article provides a broad overview, some readers seek a more integrated and detailed exploration of how lifestyle, environment, and biology connect.
For those who wish to delve deeper, Max Wild, founder of healthysimo.com and author of the free guide mentioned on our site, has compiled an extensive, evidence-informed resource. This guide, The Truth About Cancer, aims to connect complex scientific concepts in a clear, practical way. It expands on the topics discussed here, exploring the nuanced links between daily choices, our internal systems, and long-term risk, all while emphasizing the critical role of working with healthcare professionals.
Conclusion: Knowledge as Your Foundation
The journey to understanding cancer is one of replacing fear with facts and uncertainty with actionable knowledge. The science-based truth about cancer causes prevention and early detection reveals a landscape where our choices hold significant power. While not all cancers are preventable, a substantial portion of risk is influenced by the lifestyle and cancer risk factors we can modify. By focusing on evidence-based cancer prevention strategies, understanding legitimate early signs of cancer explained by science, and participating in recommended screening, we take proactive steps for our health.
Remember, this information serves as an educational starting point. Your most important partner in health is a qualified healthcare professional who can provide personalized advice tailored to your unique history and needs.
Medical Disclaimer
The content provided in this article is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or before making any changes to your healthcare regimen. Never disregard professional medical advice or delay in seeking it because of something you have read here.


1 thought on “The Truth About Cancer: What Science Really Says”