You’ve seen the statistics plastered on pamphlets in your doctor’s office and buried in online articles: “99% effective,” “93% effective.” These numbers are meant to summarize Birth Control Effectiveness, but they often create more questions than they answer. What do these figures actually mean for your life, your body, and your peace of mind? If you’ve ever felt confused about what “effectiveness” truly looks like in everyday use, you’re not alone.
The gap between perfect clinical studies and real-world, typical use is where myths thrive and anxiety grows. This confusion about true Birth Control Effectiveness isn’t your fault—it’s a natural result of complex data being oversimplified. When the stakes feel so high, understanding the real story behind the percentages is essential.
It’s time to cut through the clutter, the jargon, and the well-intentioned but misleading advice. This article exists to replace confusion with clarity by focusing squarely on the facts of Birth Control Effectiveness. We’re laying out the plain, evidence-based truth about how well birth control really works, who the most and least effective methods are designed for, and how to move past the numbers to find your genuine perfect match.
The Truth About “99% Effective”
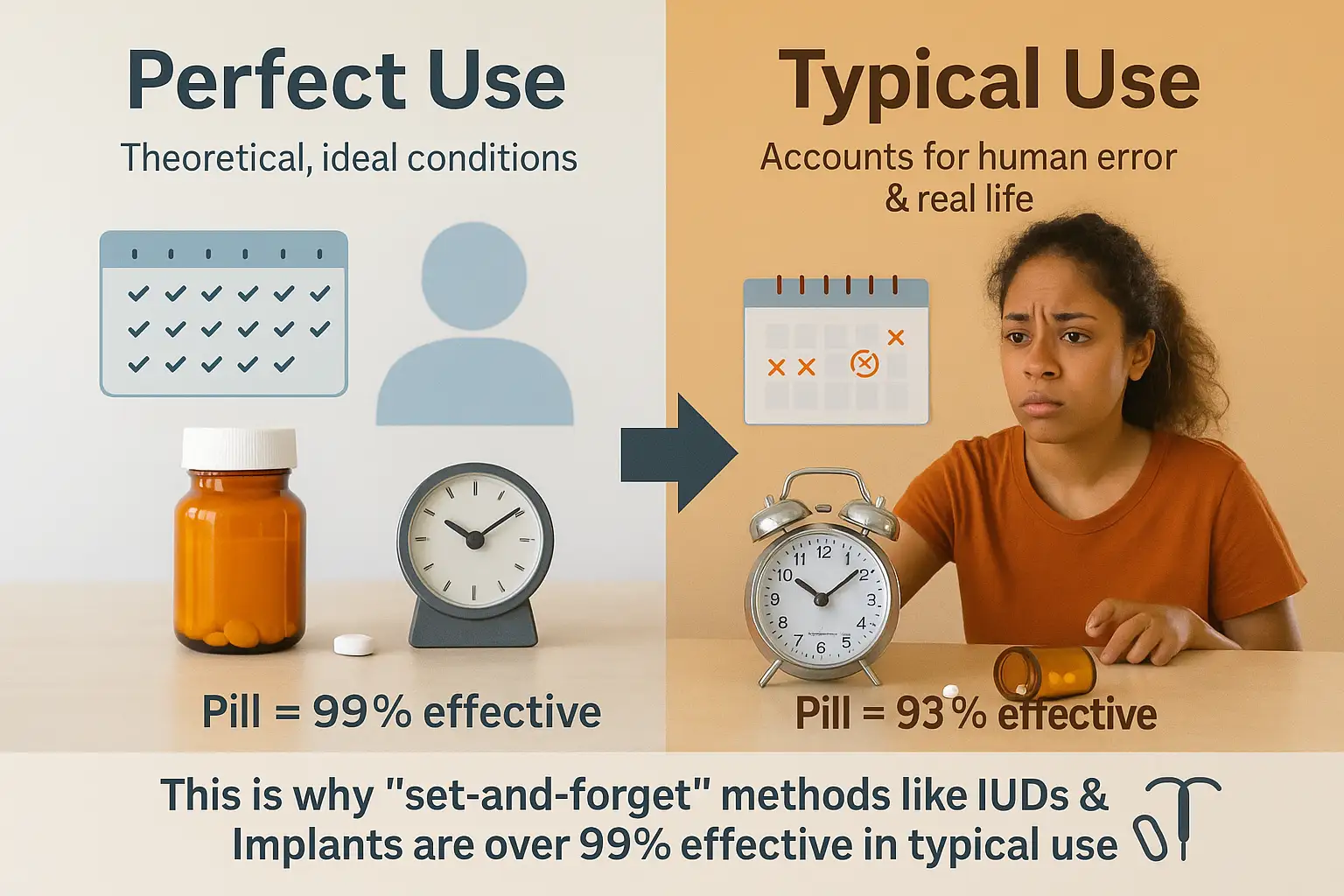
The phrase “99% effective” is the gold standard touted in birth control marketing, but it’s also the most misunderstood. The critical truth that often gets lost is that this near-perfect rate almost always refers to “perfect use”—a clinical ideal where the method is used exactly as directed, without a single error or lapse, every single time.
In reality, life is not a clinical trial. “Perfect use” doesn’t account for the human factor—the busy mornings, the travel, the simple forgetfulness that happens to everyone. This is why the most important statistic for you is “typical use.”
What “Typical Use” Really Means:
“Typical use” effectiveness is the real-world success rate that accounts for human error. It’s a far more honest and practical gauge of a method’s reliability for the average person. For example:
- The Pill: With perfect use, it’s 99% effective. But with typical use (missing a pill, taking it late, stomach bugs affecting absorption), that rate drops to 93%.
- Condoms: With perfect use, they are 98% effective. But with typical use (incorrect sizing, improper storage, breakage), that rate falls to 87%.
How to Interpret the Numbers Correctly:
A common misconception is that a 90% effective rate means the method fails 10% of the time you have sex. This is false. The effectiveness rate is an annual statistic. It means that over the course of one year, approximately 10 out of every 100 people using that method will experience an unintended pregnancy.
The “Set-and-Forget” Advantage:
This stark difference between perfect and typical use explains why Long-Acting Reversible Contraceptives (LARCs) like IUDs and implants consistently top the charts for Birth Control Effectiveness. They are designed to be “set-and-forget,” requiring no daily, weekly, or monthly action from the user. Once inserted by a healthcare provider, they work automatically for years, effectively eliminating the risk of user error. This is why their “typical use” effectiveness rate remains overwhelmingly high—over 99%—making them the most reliable form of reversible birth control available.
The Real-World Effectiveness Rankings
Let’s be blunt: when it comes to preventing pregnancy, not all birth control methods are created equal. While factors like cost, hormones, and access are vital, the most fundamental question is: “How well does it actually work?”
The following table cuts through the hype and shows the cold, hard numbers of birth control success rates with typical use. This is the data that matters most, as it reflects real-life experiences, not just ideal scenarios in a clinical trial.
| Method | Effectiveness Rate (Typical Use) | What It Means (Pregnancies per 100 Users/Year) |
|---|---|---|
| Birth Control Implant | >99% | <1 |
| IUD (Hormonal & Copper) | >99% | <1 |
| Sterilization (Vasectomy/Tubal Ligation) | >99% | <1 |
| Birth Control Shot | 96% | 4 |
| Birth Control Pill | 93% | 7 |
| Birth Control Patch | 93% | 7 |
| Vaginal Ring | 93% | 7 |
| Male Condoms | 87% | 13 |
| Diaphragm | 83% | 17 |
| Withdrawal | 80% | 20 |
| Spermicide | 79% | 21 |
| Fertility Awareness | 77% | 23 |
Understanding the “Tiers” of Effectiveness
The data reveals a clear and dramatic divide, creating three distinct tiers of Birth Control Effectiveness:
** Tier 1: The “Set-and-Forget” Powerhouses (Over 99% Effective)**
This tier includes the birth control implant, IUDs, and sterilization. Their supreme effectiveness isn’t just about technology—it’s about strategy. These are user-independent methods. Once administered by a healthcare provider, they work automatically for years, completely eliminating the risk of human error. You can’t forget to use them. This is why their “typical use” rate is identical to their “perfect use” rate.
Tier 2: The “You-Dependent” Hormonal Methods (93-96% Effective)
This tier includes the shot, pill, patch, and ring. They are highly effective if used perfectly, but their real-world success hinges entirely on consistent and correct use. A missed pill, a late shot, or a patch that falls off introduces risk. The 7% failure rate of the pill represents the gap between intention and the reality of a busy life.
Tier 3: The “Use-In-The-Moment” Barriers & Methods (77-87% Effective)
This tier includes condoms, diaphragms, withdrawal, spermicide, and fertility awareness. Their effectiveness is lowest because it depends on correct use every single time you have sex. This introduces numerous opportunities for error—from breakage and slippage to miscalculations and imperfect application.
The Untold Truth: A Stark Comparison
The most revealing way to understand this data is through direct comparison. The top-tier methods (implants and IUDs) are over 20 times more effective than methods like withdrawal, spermicide, or fertility awareness.
Consider this:
- With Fertility Awareness, approximately 23 out of 100 people will become pregnant in a year.
- With a Birth Control Implant, that number is fewer than 1.
This isn’t a matter of opinion; it’s a simple, powerful fact demonstrated by the data. Choosing a method from Tier 1 isn’t just a slightly better choice—it’s a dramatically different level of protection against pregnancy.
Debunking 3 Common Birth Control Myths
Misinformation about contraception can lead to unintended pregnancies and a false sense of security. It’s time to replace dangerous myths with empowering facts. Let’s dismantle three of the most persistent myths about Birth Control Effectiveness.
Myth 1: “The pill is almost 100% effective.”
The Myth: This pervasive idea suggests that simply being “on the pill” is a near-guarantee against pregnancy, fostering a potentially risky complacency.
The Reality: This myth dangerously conflates “perfect use” with “typical use.” While the pill is indeed 99% effective with flawless, laboratory-perfect use, the real-world statistic—93% effective with typical use—paints a very different picture.
This 6-point gap represents the countless ways daily life interferes with perfect protocol:
- Forgetting a dose: Even being a few hours late can reduce effectiveness for some pills.
- Illness: Vomiting or severe diarrhea within 3-4 hours of taking a pill can prevent absorption.
- Medications: Common antibiotics (like rifampin), certain antifungals, and even some St. John’s Wort supplements can interfere with the pill’s potency.
- Storage: Leaving pills in a hot car can degrade the hormones.
The Bottom Line: The pill is a highly effective method, but it is not infallible. Its success is a partnership between the medication and perfect user adherence—a standard that is difficult to maintain consistently.
Myth 2: “Vasectomies work immediately.”
The Myth: Many believe that male sterilization is effective from the moment the procedure is completed, leading to immediate unprotected sex and potential pregnancy.
The Reality: This is one of the most dangerously false beliefs. A vasectomy is not immediately effective. The procedure works by blocking the vas deferens, the tubes that carry sperm. However, sperm remains viable in the reproductive tract beyond the blockage site post-surgery.
It takes approximately 3 months and 15 to 20 ejaculations to fully clear the existing sperm from the pipelines. Relying on a vasectomy before this process is complete is the equivalent of using no birth control at all.
The Non-Negotiable Step: A follow-up test with a urologist is mandatory. Only a lab test confirming a zero sperm count (azoospermia) gives the all-clear. There is no other way to confirm the procedure’s success.
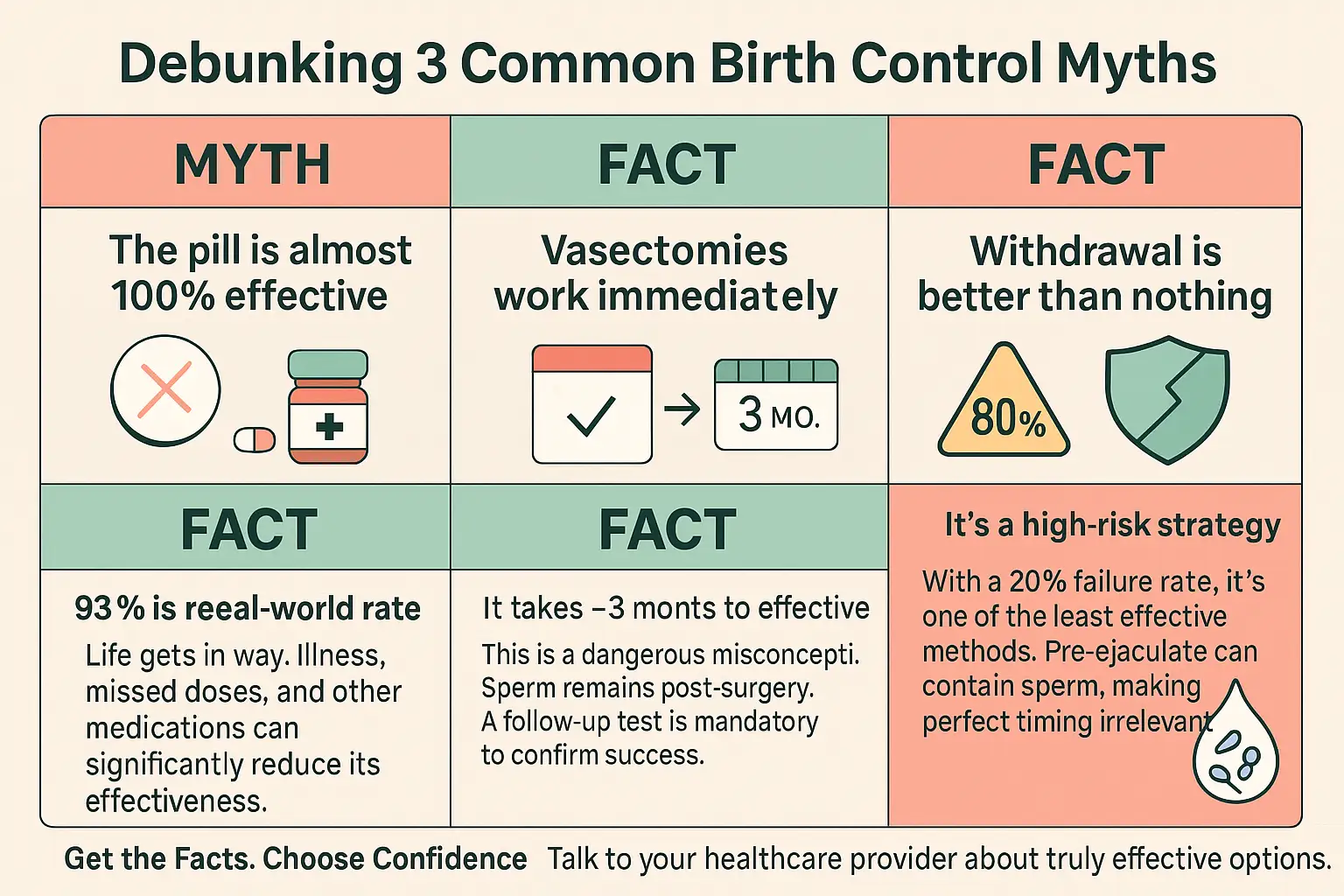
Myth 3: “Withdrawal is better than nothing.”
The Myth: This old adage frames the withdrawal method (pulling out) as a legitimate, albeit less ideal, backup plan. It implies a level of effectiveness that is misleading.
The Reality: While technically true that some protection is better than none, this myth minimizes the extreme risk involved. With a typical use effectiveness rate of only 80%, withdrawal is one of the least reliable methods available.
The high failure rate is due to two key factors:
- Pre-ejaculate (Pre-cum): This fluid, which emerges before ejaculation, can contain live sperm from previous ejaculations that remain in the urethra. This makes perfect timing irrelevant.
- The Demand for Perfect Control: The method requires the man to correctly identify and act on the point of no return—every single time—amid the passion and distraction of sex. This is a notoriously difficult task.
The Bottom Line: Framing withdrawal as “better than nothing” is like saying a paper umbrella is better than nothing in a hurricane. It offers minimal protection. For anyone serious about pregnancy prevention, it is a high-risk strategy that should not be considered a primary form of birth control.
How to Find Your Truth: Choosing the Right Method
The most powerful truth about Birth Control Effectiveness is this: the best method isn’t necessarily the one with the highest statistic—it’s the one that aligns perfectly with your body, your life, and your goals. A 99% effective method is useless if you forget to use it, can’t afford it, or hate its side effects.
Finding your match requires looking inward as much as you look at the data. It’s about honest self-reflection. Here is a guide to navigating that choice.
1. Audit Your Lifestyle & Personality
Your daily routine and habits are the biggest factor in the real-world success of “you-dependent” methods. Be brutally honest with yourself.
- The Realist: Are you organized, punctual, and blessed with a perfect memory? A daily pill or monthly ring might work well for you.
- The Free Spirit: Do you have an irregular schedule, travel frequently, or simply struggle to remember daily tasks? Your truth likely points to a low-maintenance LARC (IUD or implant) or the quarterly birth control shot. These methods forgive a busy or unpredictable lifestyle.
- The Planner: Do you prefer spontaneity in your sex life? Methods that require preparation (like a diaphragm or cervical cap) may feel like an obstacle. A method that’s always “on” might be a better fit.
2. Define Your Future Plans
Your reproductive timeline is the North Star for this decision. It helps narrow the field between reversible and permanent options.
- “I want kids soon (within a few years).”
- Focus on: Short-acting, highly reversible methods. The pill, patch, ring, or condoms offer flexibility. An IUD (which can be removed at any time by a provider) is also a fantastic, “set-and-forget” option for this stage.
- “I want kids, but not for many years.”
- Focus on: Long-Acting Reversible Contraceptives (LARCs). IUDs and implants provide powerful, hassle-free protection for 3-10 years, and fertility returns quickly after removal.
- “I am certain I do not want children, ever.”
- Focus on: Permanent sterilization. For women, this is a tubal ligation (“getting your tubes tied”). For men, it’s a vasectomy (a less invasive procedure with a easier recovery). This is the ultimate “set-and-forget” solution.

3. Consult Your Health History
Your body’s unique needs will dictate what is safe and suitable for you. This is non-negotiable.
- Health Conditions: Do you have a history of migraines with aura, high blood pressure, blood clots, or certain types of cancer? These can be contraindications for estrogen-based methods (like the combination pill, patch, or ring). Progestin-only options (the mini-pill, implant, IUD, or shot) may be safer alternatives.
- Medications: Certain antibiotics, antifungals, and anti-seizure medications can reduce the effectiveness of hormonal birth control. Always discuss your full medication list with your provider.
4. Prioritize STI Protection: The Non-Negotiable Truth
This is the most critical factor often overlooked in the effectiveness conversation.
- The Fact: With the sole exception of condoms (male and female), no birth control method protects against sexually transmitted infections (STIs).
- The Strategy: Your choice is not necessarily either/or. The most comprehensive protection strategy is dual protection.
- Example: You might choose an IUD for its 99% effectiveness against pregnancy and pair it with condoms to protect against STIs. This combines the best of both worlds: supreme pregnancy prevention and essential infection control.
Your Next Step: Use these reflections as a starting point for a conversation with your healthcare provider. They are your partner in translating your personal truth into a safe, effective, and empowering birth control choice.
From Confusion to Confidence
The journey through the numbers, myths, and methods boils down to one undeniable conclusion: knowledge is your most powerful form of contraception. The anxiety and confusion that comes from not understanding Birth Control Effectiveness can be completely replaced by the confidence of having clear, factual information.
This isn’t just about choosing the method with the highest percentage. It’s about making a smarter, more personalized choice—one that balances statistical success with the reality of your unique body, your daily life, and your long-term goals. The most effective method is the one that works for you, not just on paper.
You now possess the key insights:
- The critical difference between “perfect use” and “typical use.”
- The undeniable superiority of “set-and-forget” methods in real-world application.
- The sobering facts that debunk common and dangerous myths.
- The framework to evaluate what matters most to you—lifestyle, future plans, and health.
The time for guessing is over. The time for action is now.
Stop wondering and start knowing. Armed with these facts, you are prepared to have a productive, informed conversation with the most important person in this decision: your healthcare provider. They can translate your personal truth into a safe, effective, and empowering prescription for your life.
Schedule that appointment. Your peace of mind is worth it.
Resources and Further Reading
For more information and to continue your research, please explore these trusted resources from leading health organizations.
Authoritative Organizations & general Information:
- The American College of Obstetricians and Gynecologists (ACOG): Your premier resource for evidence-based information on all aspects of women’s health.
- Website: www.acog.org/womens-health
- Specific Page on Birth Control: www.acog.org/topics/birth-control
- Planned Parenthood: A leading provider and advocate for reproductive health care and education, offering detailed guides on every method.
- Website: www.plannedparenthood.org
- Birth Control Section: www.plannedparenthood.org/learn/birth-control
- Centers for Disease Control and Prevention (CDC): The definitive source for data and statistics on contraceptive effectiveness and use.
- Office on Women’s Health (U.S. Department of Health & Human Services): Provides comprehensive, easy-to-understand information on birth control options.
- World Health Organization (WHO): Provides global perspectives and medical guidance on family planning and contraception.
Method-Specific Information:
- Bedsider: An engaging, patient-friendly resource operated by the National Campaign to Prevent Teen and Unplanned Pregnancy. Excellent for comparing methods side-by-side.
- Website: www.bedsider.org
- Mayo Clinic & Johns Hopkins Medicine: For in-depth, medically-reviewed explanations of how different methods work, their benefits, and their risks.
Finding a Healthcare Provider:
- Physician Locators: Use the “Find an OB-GYN” tool on the ACOG website or the “Find a Health Center” tool on Planned Parenthood’s site to locate a qualified healthcare provider near you for a consultation.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Please consult with a qualified healthcare professional for personalized medical advice and to discuss the best birth control option for your individual health needs.


4 thoughts on “Setting the Record Straight: The Truth About Birth Control Effectiveness”