If you’re a woman experiencing a twinge, cramp, or persistent ache in your lower right abdomen, you’re likely searching for answers. Is it a fleeting concern or a sign of something serious? This specific type of discomfort is common, and its causes can range from routine bodily functions to conditions requiring immediate care.
This area, often called the right lower quadrant, houses several organs: your appendix, parts of your large and small intestines, your right ovary and fallopian tube, and your right ureter. Pain can originate from any of these. While often mild and temporary, understanding the potential reasons empowers you to make the right decision for your health.
Let’s address your most pressing questions about pain in the lower right abdomen.
What Could Be Causing My Lower Right Abdominal Pain?
Pain in your lower right abdomen can be confusing and concerning. To understand it, it helps to think about the organs located in this region, often referred to by doctors as the Right Lower Quadrant (RLQ). This area contains parts of your digestive system (like the appendix and colon), your right urinary tract, and for women, the right ovary and fallopian tube.
Causes can be broadly grouped into general conditions that can affect anyone and conditions specific to the female reproductive system. Let’s explore the general causes first.
Common General Causes
These conditions are not gender-specific and relate primarily to the digestive and urinary systems.
1. Appendicitis
- What it is: An inflammation of the appendix, a small finger-shaped pouch attached to your large intestine.
- Pain Description: The classic sign is pain that begins around the navel and then migrates to the lower right abdomen. The pain typically becomes constant, sharp, and worsens with movement, coughing, or sneezing. It’s often accompanied by fever, loss of appetite, and nausea.
- Why it’s urgent: Appendicitis is a medical emergency. An inflamed appendix can rupture, spilling infectious material into the abdominal cavity, leading to a life-threatening infection called peritonitis.
2. Gas and Indigestion (Dyspepsia)
- What it is: Trapped gas in the intestines or discomfort that arises during or after eating.
- Pain Description: This pain is often crampy, sharp, or creates a feeling of fullness or “knots.” It may move around and is frequently relieved by passing gas or having a bowel movement. Bloating is a common companion.
- Key Note: While extremely common and usually harmless, persistent indigestion should be discussed with a doctor to rule out other conditions.
3. Kidney Stones or Infection
- What it is:
- Kidney Stones: Hard deposits of minerals and salts that form in the kidneys.
- Kidney Infection (Pyelonephritis): Often a complication of a urinary tract infection (UTI) that has spread upward.
- Pain Description: Pain from a kidney stone is famously severe, colicky (comes in waves), and can radiate from the flank (side/back) down to the lower abdomen and groin. A kidney infection often causes a duller, constant ache in the flank or lower back, usually with fever and painful urination.
4. Irritable Bowel Syndrome (IBS)
- What it is: A common, chronic functional disorder affecting the large intestine. It involves a disruption in the gut-brain interaction.
- Pain Description: The pain is typically crampy and is directly related to bowel habits. It often improves after a bowel movement. It’s associated with bloating and changes in stool frequency/consistency (diarrhea-predominant, constipation-predominant, or mixed).
- Diagnosis: IBS is a diagnosis of exclusion, meaning other conditions must be ruled out first.
5. Inflammatory Bowel Disease (IBD) – Crohn’s Disease
- What it is: A serious autoimmune condition involving chronic inflammation of the digestive tract lining, most commonly affecting the end of the small intestine (ileum) and the beginning of the colon—both located in the lower right abdomen.
- Pain Description: Pain is often crampy or persistent, and may be accompanied by diarrhea (sometimes with blood), weight loss, and fatigue. Unlike IBS, IBD causes visible inflammation and damage to the intestinal tract.
6. Hernia (Inguinal/Femoral)
- What it is: When an organ or fatty tissue squeezes through a weak spot in the surrounding muscle or connective tissue.
- Pain Description: You may feel a dull ache or a burning/tingling sensation, especially when bending over, coughing, or lifting. A visible or palpable bulge in the groin or lower abdomen is a hallmark sign. Pain can intensify if the hernia becomes “strangulated” (blood supply cut off), which is an emergency.

What Female-Specific Conditions Cause Pain in the Lower Right Abdomen?
For women, pain in the lower right abdomen often signals an issue related to the reproductive organs located in that region—primarily the right ovary and fallopian tube. Understanding these causes is crucial because they range from normal monthly cycles to life-threatening emergencies.
Here’s a detailed breakdown of the most common female-specific causes.
1. Ovulation Pain (Mittelschmerz)
- What it is: A normal, harmless mid-cycle event. It occurs when the follicle ruptures to release an egg from the right ovary, sometimes releasing a small amount of fluid or blood that can irritate the abdominal lining.
- Pain Description: A sharp, sudden twinge or a dull, crampy ache specifically on the lower right side. It lasts from a few minutes to 24-48 hours.
- Timing: About 14 days before your next expected period.
- Associated Signs: May coincide with clear, slippery cervical mucus (fertile discharge) or light spotting.
- Action: No treatment needed. A heating pad or over-the-counter pain reliever can ease discomfort.
2. Menstrual Cramps (Dysmenorrhea)
- What it is: Pain caused by the uterus contracting to shed its lining. While usually central, cramps can be felt more prominently on one side.
- Pain Description: A dull, throbbing, or cramping ache in the lower abdomen/pelvis. It can radiate to the lower back and thighs.
- Timing: Just before or during the first few days of your menstrual period.
- Associated Signs: Bloating, fatigue, mood changes.
- Action: Managed with heat, NSAIDs (like ibuprofen), and rest. If cramps are debilitating, see a doctor to rule out secondary causes like endometriosis.
3. Ovarian Cysts
- What it is: Fluid-filled sacs that develop on or in an ovary. Most are functional cysts (follicle or corpus luteum cysts) related to the menstrual cycle and resolve on their own.
- Pain Description:
- Large Cyst: Can cause a dull ache or feeling of heaviness/pressure on one side.
- Ruptured Cyst: Causes sudden, sharp, severe pain. Pain may be brief or persistent if fluid irritates the pelvic lining.
- Associated Signs: Bloating, pain during intercourse, irregular periods. Severe rupture can cause dizziness or fever.
- Action: Most resolve without intervention. Persistent, large, or painful cysts may require monitoring, medication (like hormonal birth control), or surgery.
4. Endometriosis
- What it is: A chronic condition where tissue similar to the uterine lining grows outside the uterus, commonly on the ovaries, fallopian tubes, and pelvic lining. This tissue bleeds and inflames each cycle, causing pain and scar tissue (adhesions).
- Pain Description: Chronic pelvic pain that is often cyclic but can become constant. It includes severe menstrual cramps, deep pain during or after sex (dyspareunia), and pain with bowel movements or urination during your period.
- Key Clue: Pain that is disproportionate to your typical period cramps and may begin before your period and extend after it ends.
- Action: Requires a gynecological evaluation. Treatment focuses on managing pain and slowing tissue growth, often with hormone therapy or surgery.
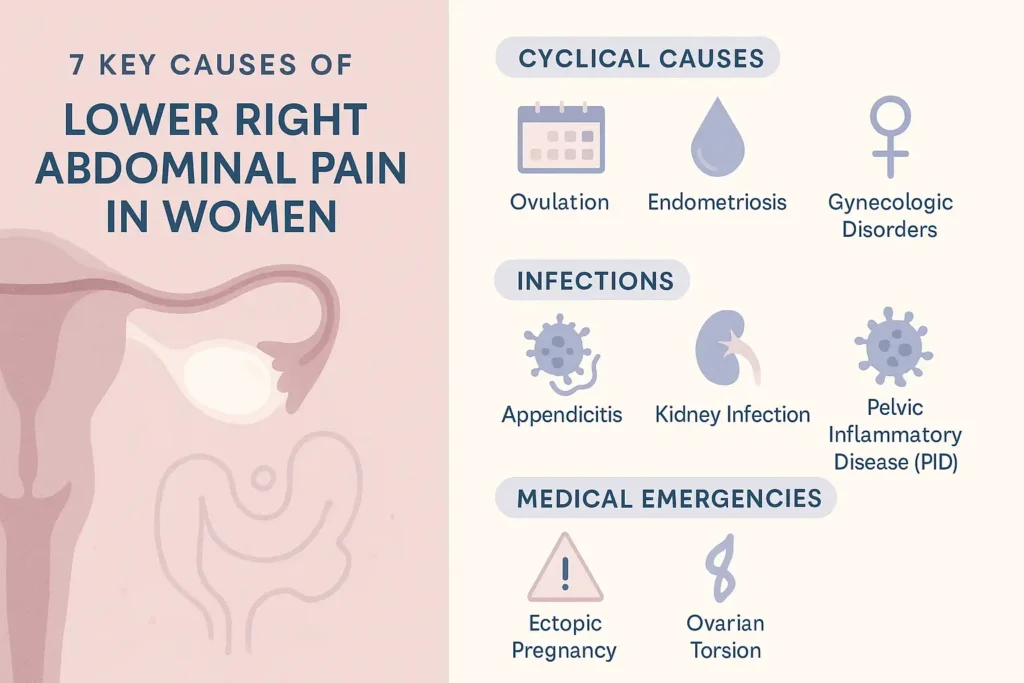
5. Pelvic Inflammatory Disease (PID)
- What it is: An infection of the upper female reproductive organs (uterus, fallopian tubes, ovaries), often caused by untreated sexually transmitted infections (STIs) like chlamydia or gonorrhea.
- Pain Description: A dull, constant ache or tenderness in the lower abdomen/pelvis, often on both sides. The pain may worsen during intercourse, a pelvic exam, or when having a bowel movement.
- Associated Signs: Fever, unusual vaginal discharge (often foul-smelling), painful urination, and irregular bleeding.
- Action: Prompt antibiotic treatment is essential to prevent permanent damage to the reproductive organs, which can lead to chronic pain, infertility, or ectopic pregnancy.
6. Ectopic Pregnancy
- What it is: A life-threatening emergency where a fertilized egg implants and grows outside the uterus, most commonly in a fallopian tube. As it grows, it can rupture the tube.
- Pain Description: Often begins as sharp, stabbing, or cramping pain on one side of the lower abdomen/pelvis. Pain may radiate to the shoulder if internal bleeding occurs.
- Associated Signs: Vaginal spotting or bleeding (different from a normal period), dizziness, fainting, signs of pregnancy (missed period, breast tenderness), and a positive pregnancy test.
- Action: This is a medical emergency requiring immediate hospital care. Treatment is necessary to stop the bleeding and remove the ectopic pregnancy.
7. Ovarian Torsion
- What it is: A surgical emergency where an ovary (and sometimes the fallopian tube) twists around its supporting tissues, cutting off its blood supply. It is often associated with an ovarian cyst.
- Pain Description: Sudden onset of severe, sharp, and constant pain on one side. The pain may be intermittent if the ovary twists and untwists initially.
- Associated Signs: Sudden nausea and vomiting, fever, and a possible tender mass felt on examination.
- Action: Requires immediate emergency surgery to untwist the ovary and restore blood flow to prevent tissue death (necrosis) and loss of the ovary.
When Should I Worry? Warning Signs Requiring Immediate Care.
Navigating lower abdominal pain often involves careful observation. While much of the discomfort can be benign, certain symptoms are red flags that should never be ignored. These signs indicate that your body may be fighting a severe infection, experiencing internal bleeding, or that an organ is at risk.
If you experience pain in your lower right abdomen alongside any of the following symptoms, seek emergency medical attention immediately. Do not wait to see if the pain subsides, and do not drive yourself to the hospital.
Critical Warning Signs and What They Mean
1. Pain That is Sudden, Severe, and Unrelenting
- What to Feel For: Pain that strikes like a light switch being flipped, is so intense it takes your breath away, or is steadily worsening by the minute.
- Why It’s Serious: This is the hallmark of catastrophic events like a ruptured appendix, a ruptured ectopic pregnancy, ovarian torsion, or a ruptured ovarian cyst. These conditions cause immediate internal trauma or cut off blood supply, requiring emergency surgery.
2. Fever and Chills with Abdominal Pain
- What to Feel For: A temperature over 100.4°F (38°C), often accompanied by shaking chills or feeling feverish.
- Why It’s Serious: Fever is a clear signal of a systemic infection. Combined with abdominal pain, it strongly suggests conditions like severe appendicitis, diverticulitis, pelvic inflammatory disease (PID), or a kidney infection that may be spreading.
3. Persistent Nausea and Vomiting (Inability to Keep Liquids Down)
- What to Feel For: Repeated vomiting, especially if you cannot sip water without vomiting it back up, or if you are vomiting dark material.
- Why It’s Serious: This indicates a significant bowel obstruction, severe inflammation, or systemic illness. It leads rapidly to dehydration and electrolyte imbalances, complicating any underlying emergency.
4. Dizziness, Lightheadedness, or Fainting
- What to Feel For: Feeling woozy, weak, or like the room is spinning when you stand up, or actually passing out.
- Why It’s Serious: This is often a sign of significant internal bleeding (from a ruptured ectopic pregnancy or cyst) or severe infection leading to sepsis. It means your blood pressure is dropping, and your brain isn’t getting enough oxygenated blood.
5. Unusual Vaginal Bleeding or Discharge
- What to Look For: Heavy bleeding outside your normal period, especially with clots; spotting accompanied by pain; or foul-smelling, yellow, or green vaginal discharge.
- Why It’s Serious: This can be a key sign of ectopic pregnancy, miscarriage, or a severe pelvic infection (PID). These conditions require immediate diagnosis and treatment to preserve fertility and health.
6. Signs of Shock: The Ultimate Medical Emergency
- What to Look/Feel For:
- Cold, clammy, pale, or blotchy skin
- Rapid, shallow breathing or shortness of breath
- Confusion, agitation, or lethargy
- A rapid, weak pulse
- Why It’s Serious: Shock occurs when vital organs do not get enough blood flow. It is a life-threatening endpoint of severe internal bleeding, massive infection (sepsis), or organ rupture. This requires immediate, lifesaving intervention.
What Should I Do For Less Severe Pain?
If your pain is mild to moderate, comes and goes (intermittent), and you have none of the emergency warning signs, you can often manage it safely at home while you monitor your symptoms. The goal is to provide comfort, reduce inflammation, and gather useful information for a potential doctor’s visit.
Follow this expanded, practical guide for self-care:
1. Prioritize Rest
- Action: Temporarily pause strenuous activities, heavy lifting, and intense exercise. Listen to your body’s signals.
- Why it helps: Physical rest reduces metabolic demand and inflammation in the affected area. It allows strained muscles to relax and can prevent irritation of digestive or reproductive organs. Consider resting in a comfortable position, such as lying on your back with a pillow under your knees to relieve abdominal tension.
2. Apply Targeted Heat
- Action: Use a heating pad, hot water bottle, or a microwavable heat wrap on the lower right abdomen for 15-20 minutes at a time. Always place a cloth layer between the heat source and your skin to prevent burns.
- Why it helps: Heat increases blood flow to the skin’s surface, which can soothe pain signals, relax tight muscles, and ease cramping in the uterine or intestinal muscles. It’s particularly effective for pain related to menstruation, ovulation, or mild digestive spasms.
3. Stay Thoughtfully Hydrated
- Action: Sip clear fluids consistently throughout the day. Optimal choices include water, electrolyte drinks, clear broths, and herbal teas like ginger or peppermint (which can also soothe digestion).
- Why it helps: Hydration helps maintain normal bowel function, preventing constipation that can worsen abdominal pressure and pain. It also supports kidney function to flush out irritants. Avoid large amounts of caffeine, sugary drinks, or carbonated beverages, which can contribute to bloating and gas.
4. Use Over-the-Counter (OTC) Medications Wisely
- Action: For inflammatory pain (like menstrual cramps or discomfort from IBS), consider a non-steroidal anti-inflammatory drug (NSAID) like ibuprofen (Advil, Motrin) or naproxen (Aleve). For pain primarily from gas or spasms, simethicone (Gas-X) or an antispasmodic might be more appropriate.
- Crucial Note: Always follow package dosage instructions. Do not take NSAIDs on an empty stomach. Avoid aspirin for pain relief in this context, as it can thin the blood. If you are pregnant, have kidney issues, or are on other medications, consult a pharmacist or doctor before taking any OTC medication.
5. Implement the “BRAT” Diet for Digestive Upset
- Action: If your pain seems related to a digestive bug or IBS flare-up, consider eating bland, easy-to-digest foods for 24-48 hours. The classic BRAT diet consists of Bananas, Rice, Applesauce, and Toast. You can also add plain crackers, boiled potatoes, and clear soups.
- Why it helps: This gives your digestive system a break, reduces irritation, and can help firm up stools if diarrhea is present. Gradually reintroduce your regular diet as symptoms improve.
6. Monitor and Log Your Symptoms
- Action: Keep a simple “Symptom Diary.” Note the date, time, and details every time you feel pain.
- What to Record:
- Intensity: Rate it on a scale of 1-10.
- Character: Sharp, dull, crampy, burning?
- Duration: How long did it last?
- Triggers: Did it occur after eating a specific food, during stress, or at a certain point in your menstrual cycle?
- What helped? Did rest, heat, or medication relieve it?
- Why it helps: This log transforms vague complaints into concrete data. It is an invaluable tool for your doctor, helping them identify patterns and make a faster, more accurate diagnosis.
The Bottom Line: Your Action Plan
- Listen to Your Body. Persistent pain in the lower right abdomen that lasts more than a few days or recurs cyclically warrants a visit to your doctor or gynecologist for evaluation.
- Don’t Ignore Red Flags. Severe pain with any of the emergency symptoms listed above means you should go to the ER or call 911. It’s always better to err on the side of caution with conditions like appendicitis or ectopic pregnancy.
- Prepare for Your Appointment. Note your symptoms, their timing related to your menstrual cycle, and any questions you have. This helps your provider make an accurate diagnosis.
While this guide answers your key questions, it is not a substitute for professional medical advice. A healthcare provider can perform the necessary exams—like a pelvic exam, ultrasound, or blood tests—to determine the specific cause of your pain in the lower right abdomen and recommend the right treatment for you.
FAQ: Your Top Questions About Pain in the Lower Right Abdomen (For Women), Answered
Q1: When is pain in my lower right abdomen a medical emergency?
A: Seek immediate emergency care if the pain is sudden, severe, and unbearable, or if it’s accompanied by:
- Fever and chills.
- Persistent vomiting (especially if you can’t keep liquids down).
- Signs of shock: dizziness, lightheadedness, rapid heart rate, or cold, clammy skin.
- Severe tenderness where even light touch to the abdomen is painful.
- Abdominal swelling or rigidity (a hard, board-like stomach).
These symptoms, especially combined with the pain, can indicate life-threatening conditions like appendicitis, a ruptured ovarian cyst, ectopic pregnancy, or ovarian torsion.
Q2: Could this pain just be from my period or ovulation?
A: Absolutely. Cyclical causes are very common:
- Ovulation Pain (Mittelschmerz): If the pain is mild, sharp, or crampy and occurs roughly halfway through your menstrual cycle (around day 14), it’s likely related to ovulation from your right ovary.
- Menstrual Cramps: Cramps can be one-sided. If the pain coincides with the start or duration of your period and is dull and aching, it may be primary dysmenorrhea.
However, if the pain is significantly worse than your typical cycle symptoms, lasts longer, or occurs at a different time, it’s wise to consult your doctor to rule out other conditions like endometriosis.
Q3: What will the doctor do to diagnose the cause?
A: Your doctor will start with a detailed history and physical exam (which may include a pelvic exam). Based on their initial assessment, they may order tests such as:
- Imaging: An ultrasound is often the first step to visualize your ovaries, appendix, and other organs. A CT scan may be used for a more detailed view.
- Lab Tests: Blood tests to check for signs of infection (high white blood cell count), inflammation, or pregnancy. A urinalysis to rule out a urinary tract or kidney infection.
- Diagnostic Laparoscopy: In some persistent, unexplained cases, a surgeon may use a small camera inserted through a tiny abdominal incision to look directly at the organs.
Q4: How can I describe my pain to the doctor effectively?
A: Being specific helps tremendously. Be prepared to describe:
- Location: Point to exactly where it hurts. Does it stay in one spot or radiate to your back or groin?
- Character: Is it sharp, stabbing, dull, achy, crampy, or burning?
- Timing: When did it start? Is it constant or does it come and go (intermittent or colicky)?
- Triggers/Alleviators: Does anything make it worse (movement, eating) or better (rest, a certain position, passing gas)?
- Associated Symptoms: Note any fever, nausea, changes in bowel habits, vaginal discharge, or menstrual changes.
Q5: Are ovarian cysts always a serious problem?
A: No. Most ovarian cysts are functional cysts (like follicular or corpus luteum cysts) related to your menstrual cycle. They often form and disappear on their own with no symptoms. Treatment becomes necessary if a cyst is large, causes persistent pain, doesn’t go away after a few cycles, or has concerning features on an ultrasound. A ruptured cyst, while painful, often heals on its own with conservative care, but severe rupture requires medical attention.
Q6: What’s the difference between IBS and pain from a gynecological issue?
A: This can be tricky, as symptoms overlap. Key differentiators include:
- IBS-Related Pain is typically linked to bowel function. It often improves after a bowel movement and is associated with bloating, gas, and changes in stool consistency (diarrhea or constipation).
- Gynecological Pain is more often linked to your menstrual cycle (timing with ovulation/periods) and may be accompanied by changes in bleeding, vaginal discharge, or pain during intercourse (dyspareunia). Keeping a symptom diary tracking pain, bowel habits, and your cycle can provide crucial clues for your doctor.
Q7: Can lifestyle changes help prevent or manage this pain?
A: For non-emergency, functional causes, yes. Strategies include:
- For Digestive Issues (IBS, Gas): Identify and avoid trigger foods (common ones are dairy, gluten, high-FODMAP foods), eat smaller meals, stay hydrated, and manage stress.
- For Menstrual Cramps: Regular exercise, using a heating pad, and dietary adjustments (reducing caffeine and salt) can help. Your doctor may also recommend specific supplements or medications.
- General Wellness: Maintaining a healthy weight, practicing good posture, and engaging in regular, moderate exercise can support overall abdominal and pelvic health.
Q8: Is it possible for the pain to be from my appendix even if it doesn’t feel extremely severe?
A: Yes. While classic appendicitis presents with severe pain, early or atypical presentations can cause milder, vague discomfort that gradually worsens over 12-24 hours. A hallmark sign is pain that migrates from the center of your abdomen to the lower right quadrant. Any persistent, worsening pain in the lower right abdomen should be evaluated by a doctor to rule out appendicitis.
Q9: Should I go to the ER or schedule a doctor’s appointment?
A: Use this rule of thumb:
- Go to the ER: For severe, sudden pain or any pain with the emergency symptoms listed in Q1.
- Schedule an Appointment: For mild to moderate pain that is persistent (lasts more than a few days), recurrent (comes back every cycle), or causes you enough concern to search for answers online. Start with your primary care physician or gynecologist.
Q10: I’m worried, but not sure it’s an emergency. What’s my first step?
A: Your first step is to call your primary care doctor’s office or gynecology clinic. Describe your symptoms to the nurse or scheduler. They can provide triage advice—whether you should be seen that day, schedule an appointment for later in the week, or proceed to urgent care/ER. Never hesitate to seek professional guidance when you’re concerned about your health.
Ressources
Professional Medical Organizations & Guidelines
- American College of Obstetricians and Gynecologists (ACOG): The leading authority on women’s health. Search their “Patient FAQs” for detailed fact sheets on endometriosis, ovarian cysts, pelvic pain, and more.
- Website: www.acog.org/womens-health
- The American College of Gastroenterology (ACG): Provides expert-informed patient education on digestive conditions like IBS, IBD, and gallstones.
- Patient Resources: gi.org/patients/
- The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Part of the NIH, this site offers in-depth, science-based information on digestive diseases and kidney conditions.
- Health Topics: www.niddk.nih.gov/health-information
Comprehensive Health Portals & Clinics
- Mayo Clinic: Renowned for its detailed, easy-to-understand symptom checkers and disease guides. An excellent resource for understanding causes, diagnosis, and treatment options.
- Abdominal Pain Guide: www.mayoclinic.org/symptoms/abdominal-pain
- Cleveland Clinic: Provides high-quality health information with a strong focus on patient education. Their articles are regularly reviewed by clinicians.
- Women’s Health Section: health.clevelandclinic.org/category/womens-health
Condition-Specific Support & Advocacy
- Endometriosis Foundation of America: A vital resource for information, community support, and advocacy for those with endometriosis.
- Website: www.endofound.org
- The IBS Network (UK): A leading charity offering evidence-based information, a self-care plan, and support for people living with Irritable Bowel Syndrome.
- Website: www.theibsnetwork.org
- Crohn’s & Colitis Foundation: The leading non-profit dedicated to finding cures for Crohn’s Disease and Ulcerative Colitis and improving patients’ quality of life.
- Website: www.crohnscolitisfoundation.org
Urgent Health Information & Tools
- CDC: Pelvic Inflammatory Disease (PID) – Detailed Guide: Essential reading on symptoms, causes, treatment, and prevention of PID from the Centers for Disease Control and Prevention.
- Page: www.cdc.gov/std/pid
- When to Go to the Emergency Room: A helpful guide from the American College of Emergency Physicians to help you make that critical decision.
- Poison Control & Emergency Hotline (USA): For any questions about poisoning or ingestion of unknown substances, call or visit online.
- Hotline: 1-800-222-1222
- Website: www.poison.org