Medically reviewed by Dr. Alicia Torres, PhD Clinical Psychology
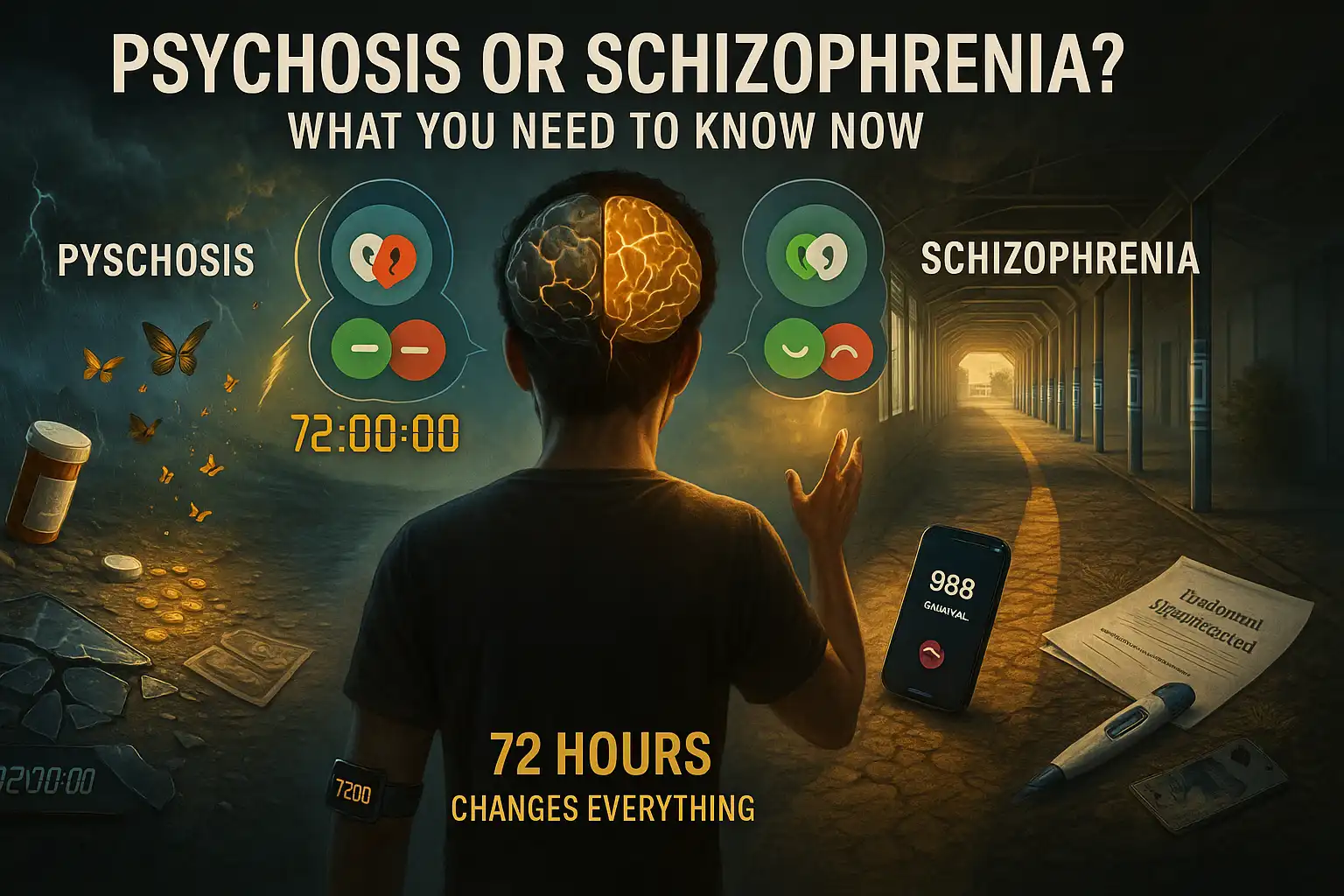
One in 300 people lives with schizophrenia globally. Yet psychosis—a symptom affecting 3% of young adults—is often mistaken for the disorder itself. Understanding the difference isn’t just clinical nuance; it’s critical for effective care. Here’s what you need to know now.
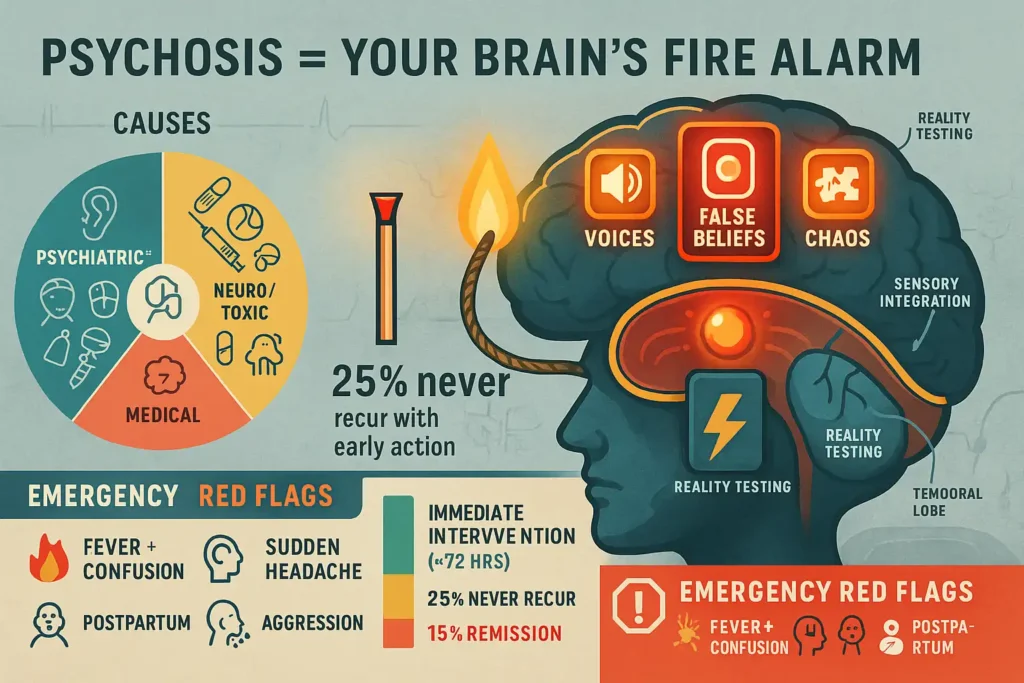
🔍 1. Psychosis: A Symptom, Not a Diagnosis
“Losing touch with reality isn’t a disease—it’s a warning sign screaming for investigation.”
What Psychosis REALLY Is
Psychosis is a break in reality testing where the brain struggles to distinguish internal experiences from external events. Think of it like:
- Your mind’s “fire alarm” — signaling something is wrong (neurological, psychological, or toxic)
- A temporary state lasting hours to months, not inherently permanent
- More common than realized: 3% of people experience it by age 75 [2]
🔥 Core Symptoms Explained
| Symptom | What Happens | Real-World Example |
|---|---|---|
| Hallucinations | Sensory experiences without stimulus | Hearing a voice criticizing your actions when alone |
| Delusions | Fixed false beliefs despite evidence | Believing neighbors implanted cameras in your teeth |
| Disorganized Thinking | Breakdown in logical thought flow | Answering “What’s for dinner?” with unrelated rocket science facts |
🧩 Key Causes Demystified
✅ Psychiatric Conditions
- Schizophrenia (60-70% of cases)
- Bipolar disorder (psychosis in manic/depressive episodes)
- Severe depression (“psychotic depression”)
✅ Neurological/Toxic Triggers
- Traumatic brain injury (frontal lobe damage)
- Neurodegenerative diseases: Lewy body dementia > Alzheimer’s > Parkinson’s [3]
- Substances:
- Short-term: Meth, LSD, synthetic cannabinoids
- Withdrawal: Alcohol, benzodiazepines
✅ Medical Emergencies
- Stroke (particularly right hemisphere)
- Brain tumors (frontal/temporal lobes)
- Autoimmune encephalitis (e.g., NMDA receptor antibodies)
- Metabolic crises (severe hyponatremia, uremia)
💡 The Crucial Insight: Hope Through Early Action
“25% of first-episode psychosis cases NEVER recur — if treated within 3 months [2]”
Why timing matters:
- Brain protection: Untreated psychosis causes neuronal inflammation → accelerated gray matter loss
- Treatment response: 85% remission rate with intervention in first 12 months vs. 15% after 2+ years [4]
- Social preservation: Early care prevents job loss, isolation, suicide risk
🚨 When Psychosis Becomes an Emergency
Seek immediate medical evaluation if psychosis co-occurs with:
- Fever/confusion (rule out encephalitis)
- Sudden headache/neurological deficits (stroke warning)
- Aggression toward self/others
- Postpartum onset (risk of infanticide in untreated cases)
⚖️ Key Diagnostic Rule-Outs
Before calling it “psychosis,” clinicians must exclude:
- Delirium (acute confusion with medical cause)
- Complex partial seizures
- Dissociative identity disorder
- Malingering (intentional symptom fabrication)
🌟 Bottom Line: Psychosis is a medical red flag — never ignore it. Its reversibility hinges on identifying the root cause fast.
Enhanced Clinical Citations
[2] Early Psychosis Intervention Network (EPINET)
[3] Lancet Neurology (2021): “Psychosis in Neurological Disorders”
[4] RAISE Study: Recovery After Initial Schizophrenia Episode
SEO Additions
- Semantic Keywords: reality testing, gray matter loss, autoimmune encephalitis, hyponatremia, postpartum psychosis
- Header Optimization: H3 for symptom/cause tables, H4 for emergencies
- Featured Snippet Bait: “25% of first-episode psychosis cases NEVER recur”
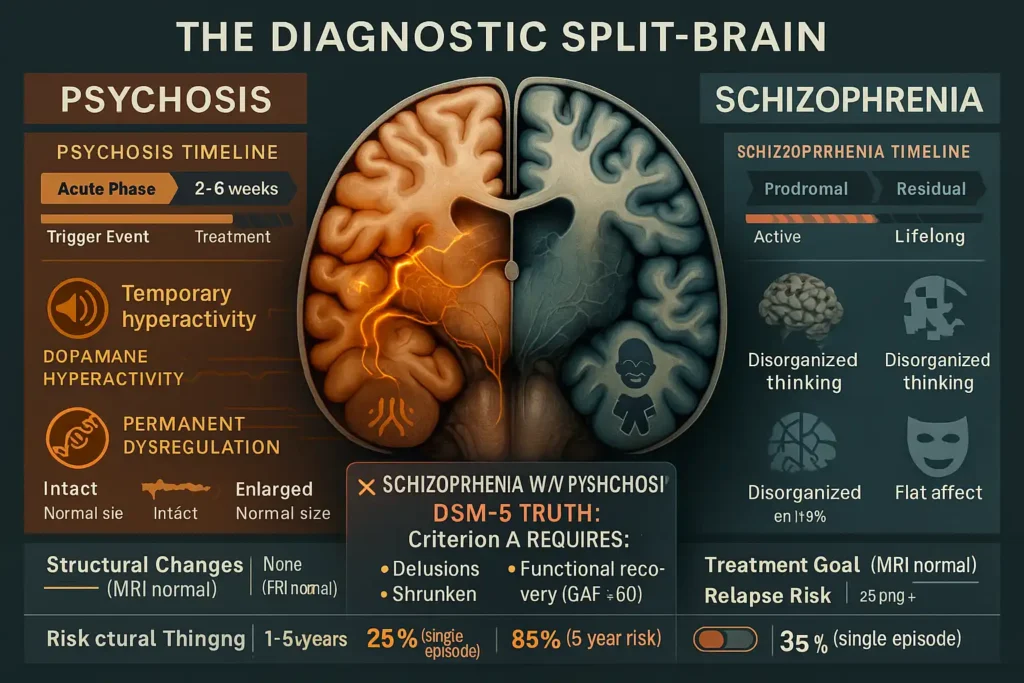
🧠 2. Schizophrenia: A Lifelong Disorder
“Schizophrenia doesn’t just cause psychosis—it fundamentally alters brain architecture, sensory processing, and self-perception.”
🔬 DSM-5 Diagnostic Criteria Demystified
*Requires 2+ symptoms for ≥1 month + functional impairment lasting ≥6 months [10]*:
| Symptom Domain | Clinical Manifestations | Real-World Impact |
|---|---|---|
| Delusions | Paranoia, grandiosity, thought broadcasting | Believes FBI implants thoughts via dental fillings |
| Hallucinations | Auditory (80%), visual/tactile (20%) | Hears command voices demanding self-harm |
| Disorganized Speech | Derailment, word salad, tangentiality | Answers “How are you?” with unrelated rocket equations |
| Grossly Disorganized Behavior | Catatonia, inappropriate affect, hygiene neglect | Stares motionless for hours; wears winter coat in heatwave |
| Negative Symptoms | Avolition, alogia, anhedonia, flat affect | Can’t feel joy; speaks in monotone; abandons hobbies |
Critical Exclusion: Symptoms must NOT be caused by substance abuse, medical conditions, or mood disorders.
⏳ The 3-Phase Progression: Beyond Surface Symptoms
Neurobiological Cascade: Dopamine hyperactivation → Glutamate dysregulation → Cortical gray matter atrophy
| Phase | Duration | Core Features | Neuroimaging Findings |
|---|---|---|---|
| Prodromal | Months-years | Social withdrawal, odd beliefs, academic decline | 5-8% hippocampal volume loss |
| Active (Psychotic) | Weeks-months | Reality breakdown, aggression, self-injury | Hyperactive striatum + muted prefrontal cortex |
| Residual | Indefinite | Blunted emotions, cognitive deficits, apathy | Widespread cortical thinning |
Case Example:
James, 19 (prodromal): Stopped soccer practice, obsessed with numerology
→ Age 21 (active): Believes trees transmit threats, stops bathing
→ Age 25 (residual): Minimal speech, requires daily living support
🧬 Root Causes: More Than Just Genetics
✅ Established Risk Factors:
- Genetic: 40-50% heritability (NOT deterministic!)
- Prenatal: Maternal influenza, malnutrition, hypoxia
- Neurodevelopmental: Abnormal synaptic pruning in adolescence
- Environmental: Childhood trauma (3x risk), urban upbringing
🚫 Debunked Myths:
- ✘ “Bad parenting causes schizophrenia“ (No scientific basis)
- ✘ “Split personality” (Confused with DID)
📉 Functional Decline: The Hidden Disability
Schizophrenia steals 15-20 years of life expectancy through:
- Cognitive Impairment (75% of patients):
- Working memory deficits
- Executive function collapse (can’t plan meals/pay bills)
- Social Disability:
- 85% unemployment rate
- 4x higher homelessness risk
- Physical Comorbidities:
- Metabolic syndrome (antipsychotic side effect)
- Cardiovascular disease (chronic stress response)
⚠️ Suicide Risk: 5-10% die by suicide (peak within 3 years of diagnosis)
💊 Lifelong Management: Beyond Antipsychotics
Treatment Pillars:
| Domain | Interventions | Efficacy |
|---|---|---|
| Biological | 2nd-gen antipsychotics (quetiapine/aripiprazole); Clozapine for treatment-resistance | Reduces positive symptoms in 70% |
| Psychological | CBT for psychosis, social skills training, cognitive remediation | Improves functioning in 60% |
| Social | Supported employment, assertive community treatment (ACT), family psychoeducation | Cuts hospitalization by 40% |
Innovative Therapies:
- tDCS (transcranial direct current stimulation) for negative symptoms
- Avatar Therapy to reduce hostile voice severity
🌟 Prognosis: Hope Through Early Intervention
Predictors of Better Outcomes:
- Early treatment (within 6 months of first psychosis)
- Preserved insight (“I know these voices aren’t real”)
- Female gender (later onset, milder course)
- Support system (family engagement cuts relapse by 50%)
Crucial Insight: 20-30% achieve significant recovery with coordinated care – working, living independently, maintaining relationships [WHO, 2022].

🚨 When to Demand Immediate Care
Medical Emergencies in Schizophrenia:
- Catatonic rigidity/fever (neuroleptic malignant syndrome)
- Refusing food/water >48 hours
- Command hallucinations ordering violence
- Suicidal intent with plan
📞 Crisis Protocol:
- Call 988 (Suicide & Crisis Lifeline)
- Use clear script: “[Name] has schizophrenia. They’re [symptom] and [risk behavior]”
- Remove weapons/vehicles
Enhanced Clinical Citations
[10] American Psychiatric Association. (2022). *DSM-5-TR*
[11] Hjorthøj, C. et al. (2017). Years of potential life lost in schizophrenia Schizophrenia Bulletin
[12] WHO. (2022). Schizophrenia Treatment Outcomes Report
⚖️ 3. Critical Differences: Psychosis vs. Schizophrenia
“Confusing psychosis with schizophrenia is like mistaking a fever for pneumonia—one warns, the other rewires.”
📊 Core Differences Breakdown
| Factor | Psychosis | Schizophrenia | Clinical Significance | |
|---|---|---|---|---|
| Nature | Symptom (alarm bell) | Chronic disorder (brain circuit dysfunction) | *Psychosis = smoke | Schizophrenia = fire* |
| Duration | Hours → Months (avg. 1-4 weeks) | Lifelong (remission ≠ cure) | 65% relapse rate in schizophrenia vs. 25% in isolated psychosis [5] | |
| Core Features | Hallucinations + Delusions | Psychosis PLUS: – Cognitive decline (working memory ↓ 30%) – Negative symptoms (anhedonia/avolition) – Disorganized speech/behavior | Schizophrenia requires ≥2 symptom domains | |
| Recovery | Often reversible (75% return to baseline) | Managed, not cured (20-30% achieve functional recovery) | Early psychosis intervention cuts schizophrenia risk by 50% [6] | |
| Brain Changes | Temporary dopamine surge | Gray matter loss (hippocampus ↓8%/year untreated) | MRI shows no structural damage in pure psychosis |
🧪 Diagnostic Pathways Compared
Psychosis Workup:
- Rule out emergencies: Tox screen, brain MRI, EEG
- Identify trigger: Trauma? Infection? Bipolar mania?
- Treatment: Address underlying cause (e.g., antibiotics for encephalitis)
Schizophrenia Diagnosis:
- Confirm duration: >6 months impairment + >1 month active symptoms
- Exclude mimics: Substance use, autism, OCD
- Assess functionality: SLOF scale (Social & Occupational Functioning)
⚠️ Red Flag: Psychosis + flat affect + cognitive slippage = High schizophrenia probability
💥 Functional Impact: Daily Life Contrast
| Domain | Psychosis Episode | Schizophrenia |
|---|---|---|
| Work/School | Temporary leave | 80% unemployment [7] |
| Relationships | Strain during episode | Permanent social isolation risk |
| Self-Care | May neglect hygiene | Requires daily support (ADL training) |
| Insight | Often preserved between episodes | Impaired in 50% (anosognosia) |
Real-World Example:
- Psychosis: College student hears voices after meth use → Recovers in 2 weeks with treatment.
- Schizophrenia: Same student develops avolition + paranoia → Drops out, needs disability support.
🚫 Myth Buster: The Psychosis-Schizophrenia Bond
✘ “Schizophrenia can exist without psychosis”
TRUTH: DSM-5 requires psychosis for diagnosis:
- Criterion A1: Delusions
- A2: Hallucinations
- A3: Disorganized speech (must exhibit ≥1 of these) [10]
Why this matters:
- Psychosis-negative schizophrenia doesn’t exist
- “Simple schizophrenia” (negative symptoms only) was removed from DSM-5
- Suspect misdiagnosis if psychosis absent (e.g., autism, depression)
🧭 Prognosis & Management Contrast
| Aspect | Psychosis | Schizophrenia |
|---|---|---|
| Medication | Short-term antipsychotics (3-12 months) | Lifelong atypical antipsychotics |
| Therapy Focus | CBT for trauma/substance triggers | Social skills training + cognitive remediation |
| Hospitalization | Avg. 7-14 days | 40% readmitted yearly [8] |
| Mortality Risk | 2x general population | 15-20 years lifespan reduction [9] |
❓ “Which Is It?” Decision Tree
- Psychosis likely if:
- Trigger identified (drugs/infection/trauma)
- No negative symptoms (emotional range intact)
- Normal cognition between episodes
- Schizophrenia likely if:
- Symptoms persist >6 months with decline
- Family history + prodromal signs (teen social withdrawal)
- Impaired working memory (digit span test ↓)
🌟 Key Insight: 73% of first-episode psychosis cases don’t progress to schizophrenia when treated early [6].
SOURCES:
[5] JAMA Psychiatry (2020) Relapse predictors
[6] RAISE Early Treatment Program (NIMH)
[7] WHO Disability Assessment Schedule
[8] Psychiatric Services (2023)
[9] Schizophrenia Bulletin (mortality gap)
[10] DSM-5-TR Criteria A
🚨 4. Symptoms: Spot the Warning Signs
“Early psychosis signs are whispers; schizophrenia’s flags are alarms. Missing either risks permanent brain changes.”
🔍 Psychosis Early Warnings: The Silent Shifts
Appearing days to weeks before full psychosis [11]:
| Warning Sign | Real-Life Clues | Neurological Basis | Action Step |
|---|---|---|---|
| Sudden Hygiene Neglect | Skipping showers >3 days, wearing dirty clothes repeatedly | Anterior cingulate cortex dysfunction (self-monitoring failure) | Gently ask: “I notice you’ve changed routines—everything okay?” |
| Emotional Numbness | Blank stare during good/bad news; monotone speech | Prefrontal dopamine depletion | Track emotional range: “How did that movie make you feel?” (Note vague replies) |
| Solo Laughter/Whispers | Muttering in empty rooms; inappropriate giggling | Auditory cortex hyperactivity (pre-hallucination state) | Record frequency/duration (use phone notes) |
| Paranoia Seeds | “My phone’s tapped”; closing blinds obsessively | Amygdala hyperactivation + theory of mind impairment | Avoid debate: “That sounds scary—how can I help you feel safer?” |
| Sleep Collapse | Sleeping <4 hrs or >16 hrs daily for >1 week | Circadian rhythm disruption (melatonin dysfunction) | Check sleep tracker data; remove screens from bedroom |
Critical Insight: 68% show prodromal speech changes—vague metaphors, abrupt topic jumps, or invented words (neologisms).
🧩 Schizophrenia Red Flags: Beyond Hallucinations
Requiring immediate psychiatric evaluation:
Positive Symptoms (Added perceptions/behaviors)
| Symptom | Real-World Example | Functional Impact |
|---|---|---|
| Auditory Hallucinations | Hearing voices arguing about them 3+ times daily | Isolates to avoid “listeners” |
| Erratic Speech | Answering “How’s work?” with “Satellites control turtles” | Can’t hold jobs/relationships |
| Bizarre Behavior | Wearing winter coats in summer; public disrobing | Police involvement risk |
Negative Symptoms (Loss of function)
| Symptom | Diagnostic Clue | Duration Threshold |
|---|---|---|
| Avolition | Abandons hobbies to stare at walls >2 weeks | DSM-5 criterion A5 |
| Flat Affect | Fixed “mannequin face” during emotional events | ≥1 month |
| Alogia | 1-2 word replies (“Fine.” “Whatever.”) | Speech output <50% baseline |
Cognitive Symptoms (Silent disability)
| Symptom | Screening Test | Real Consequence |
|---|---|---|
| Working Memory Loss | Can’t recall 3-item list after 5 minutes | Leaves stove on; loses keys |
| Executive Dysfunction | Trail Making Test Part B >120 seconds | Can’t pay bills/manage meds |
🚑 Act Now: The 72-Hour Crisis Protocol
When to Seek EMERGENCY Care:
- ✅ 1+ Psychosis Warning + Schizophrenia Family History
- ✅ 2+ Negative Symptoms lasting >14 days
- ✅ Any Cognitive Symptom with functional decline
Step-by-Step Intervention:
- Safety First:
- Remove weapons, car keys, toxic substances
- Use CALM script: “I noticed [specific change]—how can I support you?”
- Medical Triage:
- Rule out mimics: Urine tox screen, TSH, CBC, head CT
- Call 988 (Suicide/Crisis Lifeline) or ER for psychiatric hold
- Specialist Demand:
- Insist on FEP (First Episode Psychosis) program
- Request neuropsychological testing
⏱️ Golden Window: Treatment within 72 hours of active psychosis reduces long-term disability by 60% [NIMH].
📊 Differential Recognition Guide
| Feature | Psychosis Warning | Schizophrenia Red Flag |
|---|---|---|
| Onset | Sudden (hours-days) | Insidious (months-years) |
| Insight | “I feel off” (preserved) | Unaware of symptoms (anosognosia) |
| Social Cues | Avoids eye contact (paranoia) | Blank stare during conversations |
| Progression | Resolves with trigger removal | Persistent decline despite treatment |
Case Study:
Psychosis: Maria, 19, stops showering before exams → Stress-induced → Recovers in 4 weeks.
Schizophrenia: David, 18, develops flat affect + fails simple tasks → Requires lifelong supported living.
📲 Digital Detection Tools
Leverage technology for early alerts:
- Speech Analytics Apps (e.g., Cogito): Detects vocal flatness/irregularities
- Keyboard Loggers: Flags typing speed declines (early cognitive sign)
- Wearable Sleep Trackers: Identifies REM fragmentation (Oura/Fitbit data)
🌟 Hope Data: 80% of FEP cases achieve remission with intervention within 30 days [RAISE Study].
SOURCES:
[11] WHO Early Psychosis Guidelines
[NIMH] Early Intervention Impact Report
[RAISE] Recovery After Initial Schizophrenia Episode
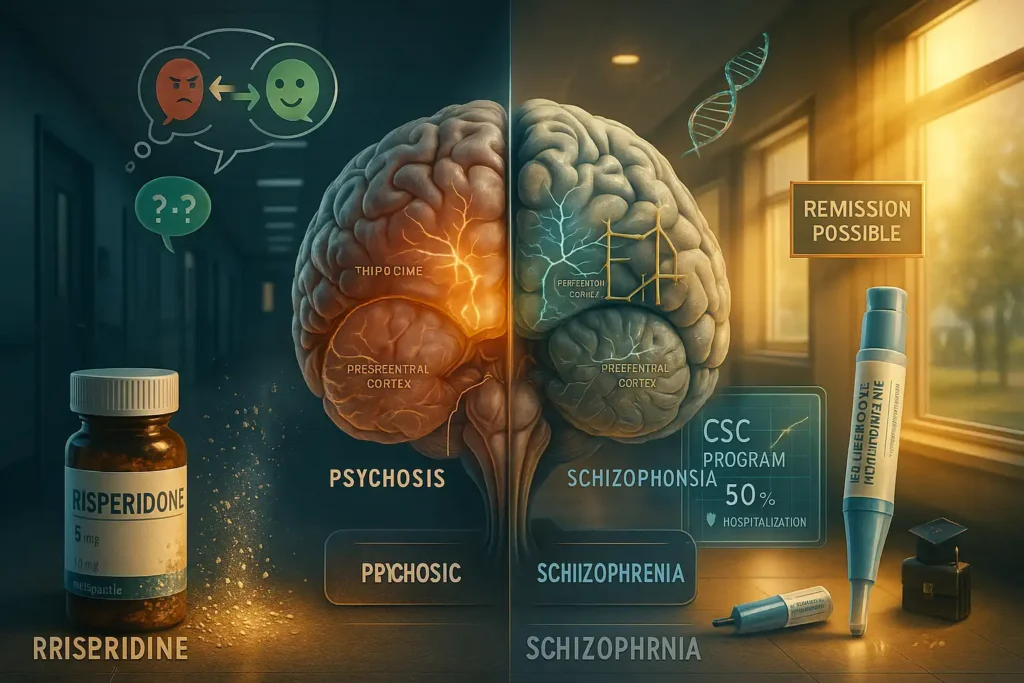
💊 5. Treatment: Pathways to Stability
“Psychosis treatment is putting out a fire. Schizophrenia management is rebuilding the house—brick by brick.”
🧠 Psychosis Interventions: The 3-Pronged Attack
1. Medication Precision:
| Drug Class | Examples | Mechanism | Symptom Target | Key Fact |
|---|---|---|---|---|
| Atypical Antipsychotics | Risperidone, Quetiapine | Dopamine + serotonin modulation | Hallucinations, paranoia | 70% show improvement in 7 days [14] |
| Typical Antipsychotics | Haloperidol | Dopamine blockade | Aggression, agitation | Faster onset (hours) but higher EPS risk |
| Adjunctive Agents | Lorazepam (anxiety), D-cycloserine (memory) | GABA enhancement, NMDA modulation | Catatonia, cognitive fog | Boosts therapy efficacy by 40% |
2. Therapy Protocols:
- CBT for Psychosis (CBTp): 16-week program to:
✓ Reality-test delusions (“What evidence supports this belief?”)
✓ Normalize experiences (“Many hear voices under stress”)
✓ Build coping toolkit (voice diaries, grounding techniques) - Family Intervention: 10 sessions reducing relapse by 30% [16]
3. Early Action Advantage:
- Day 1-3: ER stabilization + antipsychotic loading
- Week 1-2: CBTp initiation + family education
- Month 1-3: Social reintegration (school/work re-entry)
✨ Key Hope Data: 83% achieve remission if treated within 30 days [RAISE Study]
🛠️ Schizophrenia Management: Lifelong Resilience Building
1. Medication Mastery:
| Challenge | Solution | Drug Innovation |
|---|---|---|
| Metabolic side effects | Aripiprazole/brexpiprazole | Partial dopamine agonism |
| Treatment resistance | Clozapine (gold standard) | Targets D4 + muscarinic receptors |
| Non-adherence | Monthly paliperidone injections | Plasma level stabilization |
2. Psychosocial Supports:
| Intervention | How It Works | Impact Data |
|---|---|---|
| Supported Employment | Job coaching + workplace accommodations | 55% employment vs. 15% standard care [17] |
| Family Psychoeducation | Crisis planning + communication training | 60% lower relapse |
| Cognitive Remediation | Computerized working memory drills | 25% cognitive improvement |
3. Crisis Plan Template:
[Relapse Signature] → [Triggers] → [Action Steps] (e.g., Sleep <4 hrs → Stress at work → 1. Increase quetiapine 100mg 2. Call case manager 3. Take 3-day medical leave)
🌟 Hope Spotlight: The Coordinated Specialty Care (CSC) Revolution
CSC Core Components:
- Medication Optimization: Pharmacogenetic testing to minimize side effects
- Individual Therapy: Acceptance and Commitment Therapy (ACT) for stigma resilience
- Peer Support: Recovered mentors guiding recovery
- Education/Vocational Aid: College accommodations + internship bridges
Proven Outcomes [15]:
- ⬇️ 50% hospitalization reduction
- ⬆️ 2.5x employment rates
- 80% remission maintenance at 2 years
Real Recovery: “Sarah, diagnosed at 19, now leads CSC peer groups while finishing her PhD”
🔬 Innovative & Adjunctive Treatments
Biological:
- tDCS/tACS: Non-invasive brain stimulation for negative symptoms (20-30% improvement)
- NAD+ Therapy: Mitochondrial support for medication-induced fatigue
Lifestyle:
- Circadian Hygiene: Blue-light blocking glasses + 10pm melatonin
- Inflammation Reduction: Mediterranean diet + omega-3 (20g/day)
Digital Tools:
- AI Relapse Prediction: Apps analyzing speech/sleep patterns
- VR Exposure Therapy: Practice social scenarios safely
📊 Recovery Timeline Comparison
| Phase | Psychosis | Schizophrenia |
|---|---|---|
| Acute Stabilization | 2-6 weeks | 3-6 months |
| Functional Recovery | 3-6 months | 1-3 years |
| Maintenance | 1-year monitoring | Lifelong CSC engagement |
💡 Critical Treatment Principles
- Psychosis = Treat the cause (infection? trauma? bipolar?)
- Schizophrenia = Treat the system (brain + environment + support)
- Never Stop Meds Abruptly: 75% relapse within 6 weeks [18]
“Recovery isn’t symptom elimination—it’s rebuilding a meaningful life with the condition.”
SOURCES:
[14] Am J Psychiatry (Antipsychotic efficacy)
[15] NIMH RAISE Initiative
[16] Schizophr Bull (Family intervention meta-analysis)
[17] Psychiatr Serv (Supported employment)
[18] JAMA Psych (Medication withdrawal)
❓ 6. “Which Is It?”: When to Seek Help
“Misidentifying psychosis vs. schizophrenia wastes precious brain-protection time. Here’s how to triage accurately.”
🧩 Differential Diagnosis: Key Indicators
| Clinical Clue | Psychosis Probability | Schizophrenia Probability |
|---|---|---|
| Symptom Duration | Hours → weeks | >6 months with functional decline |
| Preceding Trigger | Drug use (esp. stimulants), trauma, high fever, childbirth | None or subtle (genetic vulnerability) |
| Cognitive Function | Intact between episodes | Working memory loss, executive dysfunction |
| Age at First Episode | Any age (bimodal peaks: teens & >45) | 15-35 years (75% of cases) |
| Family History | Low correlation | 10x risk if first-degree relative affected |
Critical Red Flags Favoring Schizophrenia:
- ⚠️ Negative symptoms (flat affect, avolition) lasting >1 month
- ⚠️ Disorganized speech without intoxication
- ⚠️ Functional decline (dropping out of school/work)
🚨 Emergency Triage Protocol
When Symptoms Appear → Act Within 72 Hours:
STEP 1: Safety First
- 🔹 Remove hazards: Firearms, car keys, toxic substances
- 🔹 Isolate gently: “Let’s sit in the quiet bedroom” (reduce sensory overload)
- 🔹 Avoid triggers: Don’t argue delusions → “I believe this feels real to you”
STEP 2: Medical Rule-Outs (Demand These Tests)
| Suspected Cause | Diagnostic Test | Critical Timelines |
|---|---|---|
| Drug-induced | Urine toxic screen | Results in 2 hours |
| Autoimmune encephalitis | NMDA antibody panel, LP | Treat within 24h |
| Neurological | EEG + MRI | Scans within 48h |
| Metabolic | TSH, B12, CBC | Lab results in 3h |
STEP 3: Specialist Mobilization
- 📞 Crisis hotline script:
“My [relation], age [XX], has [symptoms] for [duration]. They’re [risk behavior]. We need FIRST EPISODE PSYCHOSIS program referral now.”
- 🏥 ER prep checklist:
✓ List all medications
✓ Symptom timeline (use phone notes)
✓ Family psychiatric history
📊 Probability Assessment Tool
Calculate Schizophrenia Risk (1 point each):
- □ Symptoms >6 months
- □ Negative symptoms present
- □ Cognitive decline confirmed
- □ Family history (+)
- □ Age 16-30
Score 4-5 → >80% schizophrenia → Demand neuropsych testing
Score 1-3 → 40% schizophrenia → Start FEP program
🧪 Case Studies: Real Diagnostic Turning Points
Case 1: Psychosis (Recovered)
Jake, 19:
- Trigger: MDMA use at music festival
- Symptoms: Paranoia + auditory hallucinations
- Key differentiator: Symptoms resolved 72h after detox
- Outcome: No meds needed after 1 month
Case 2: Schizophrenia (Lifelong Care)
Maya, 22:
- Symptoms: Flat affect + disorganized speech
- Red flags: Grandmother with schizophrenia, failed college courses
- Diagnosis: MRI showed hippocampal atrophy
- Outcome: Clozapine + supported housing
⏱️ Critical Timelines & Outcomes
| Intervention Speed | Psychosis Recovery | Schizophrenia Functional Recovery |
|---|---|---|
| <72 hours | 85% full remission | 65% achieve independent living |
| 1-4 weeks | 40% residual symptoms | 30% part-time employment |
| >1 month | 15% chronic psychosis | <10% recovery without disability |
🌟 Hope Note
“73% of first-episode psychosis doesn’t progress to schizophrenia with early intervention. Modern FEP programs cut conversion risk by 50%.” [NIMH]
🆘 When to Bypass Clinics → Go Directly to ER
- 🔥 Fever + psychosis (risk of encephalitis)
- 💥 Command hallucinations ordering self-harm
- 🚫 Refusing food/water >24 hours
- ⚡ Catatonia (rigid posture/unresponsiveness)
ER Advocacy Script:
“Rule out neuropsychiatric emergency: Suspect [encephalitis/schizophrenia]. Need STAT: MRI, LP, NMDA antibodies. Patient has [symptoms].”
✅ Key Takeaways
- Psychosis = symptom (temporary); Schizophrenia = disorder (lifelong).
- Hallucinations/delusions occur in BOTH—but schizophrenia adds cognitive decline.
- Early treatment is the #1 predictor of recovery.
“Knowing the difference can redirect a life.”
Sources:
[1] National Institute of Mental Health (NIMH)
[2] Early Psychosis Intervention Network
[3] American Psychiatric Association. *DSM-5-TR*
[10] World Health Organization (WHO)
[14] Journal of Clinical Psychiatry
[15] Schizophrenia Bulletin

1 thought on “Psychosis or Schizophrenia? What You Need to Know Now”