For individuals with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), the fear of the “crash” is a constant companion. This crash, known clinically as Post-Exertional Malaise (PEM), is not just simple fatigue. It’s a profound, often delayed worsening of a wide range of symptoms triggered by exertion that would be manageable for a healthy person. The key to managing ME/CFS lies not in pushing through, but in understanding your body’s unique warning signs. This guide will help you spot and avoid your personal PEM triggers.
What Exactly is Post-Exertional Malaise?
To understand Post-Exertional Malaise (PEM), it’s crucial to first dismiss the common misconception that it is simply getting tired after activity. For individuals with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), PEM is a distinct, pathological, and often debilitating response that is the core hallmark of the disease. It represents a fundamental breakdown in the body’s ability to generate and manage energy.
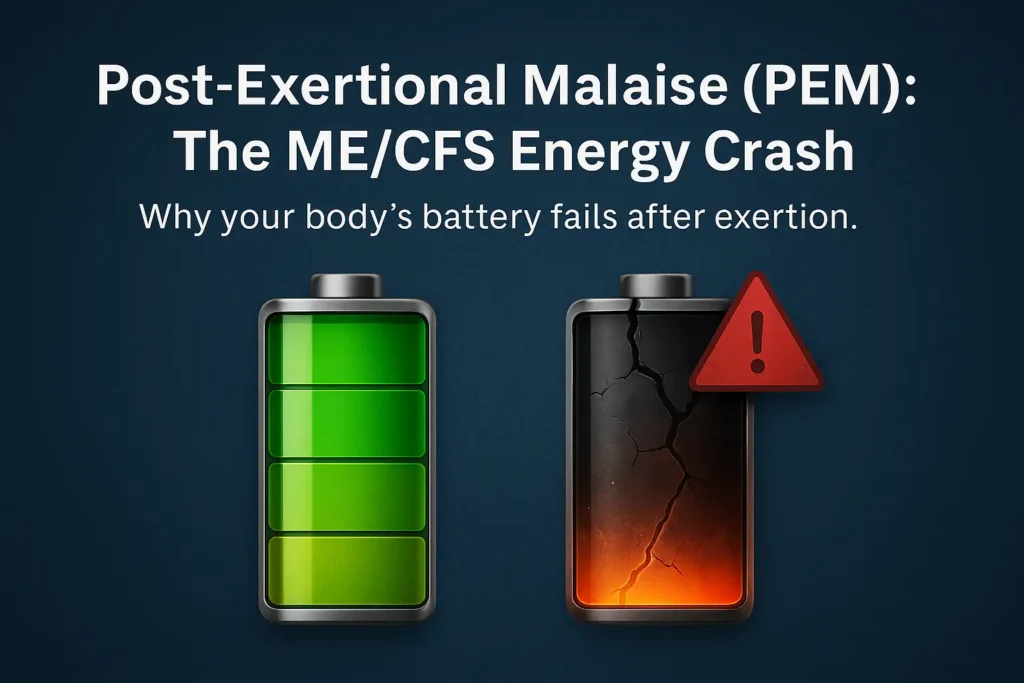
Think of a healthy body’s energy system like a well-functioning battery. After exertion, it becomes depleted but recharges efficiently with rest. For someone with ME/CFS, the battery is not only smaller and drains faster, but the charging mechanism itself is broken. PEM is the severe and prolonged “power failure” that occurs when the system is pushed beyond its limited capacity.
Here’s a breakdown of what makes PEM unique:
- A Pathological Response, Not Laziness: PEM is not a choice or a psychological state. It is a documented physiological dysfunction. Research suggests it may be linked to problems with cellular energy production (impaired ATP synthesis), neurological dysfunction, and an abnormal immune system response. The body essentially hits a hard wall, signaling a systemic failure.
- The “Payback” is Disproportionate: The defining characteristic of PEM is the severe and disproportionate worsening of symptoms relative to the exertion. A minor activity—like taking a shower, having a short conversation, or reading a few pages—can trigger a “crash” that leaves a person bedridden for days, akin to a healthy person running a marathon with a severe flu.
- The Delayed Onset: One of the most insidious aspects of PEM is its delayed timing. Symptoms typically worsen 12 to 48 hours after the triggering activity. This lag makes it incredibly difficult for patients and doctors to immediately connect the cause and effect. You might feel relatively okay the day of an activity, only to collapse two days later, creating a cycle of “boom and bust” that is hard to escape.
- A Full-Body System Collapse: PEM is not just one symptom. It’s a cascade of system-wide malfunctions. It can intensify every ME/CFS symptom, including:
- Cognitive Dysfunction: Severe “brain fog,” making it difficult to think, speak, or remember.
- Immune Response: Flu-like symptoms such as sore throat, swollen lymph nodes, and feverishness.
- Neurological Issues: Dizziness, noise/light sensitivity, and pain.
- Energy Depletion: A profound, crushing fatigue that rest does not alleviate.
In essence, Post-Exertional Malaise is the body’s severe and punishing response to energy expenditure that it cannot tolerate. Understanding that PEM is a biological reality—a literal “sickness after exertion”—is the first and most critical step in learning to manage ME/CFS and validate the experiences of those who live with it.
The Many Faces of a PEM Crash: Recognizing the Symptoms
Understanding Post-Exertional Malaise requires recognizing that a “crash” is not a single sensation but a complex, multi-system failure. The symptoms of PEM can vary dramatically from one person to another and can even shift from one episode to the next in the same individual. This variability often makes PEM difficult to explain to others. Below is a detailed breakdown of the common symptom categories, with specific examples to help you identify your own experience.
1. Severe Flu-Like Symptoms & Immune Response
Your body reacts as if it’s fighting a major infection, even when no virus is present.
- In Detail: This isn’t just “feeling a bit off.” It’s a profound, whole-body malaise. You might experience a raw, sore throat without being sick, tender, swollen lymph nodes in your neck or armpits, deep muscle aches similar to the flu, unexplained chills or night sweats, and debilitating headaches that can be tension-related or even migraine-like.
- Why it matters: This immune system activation is a key indicator that PEM is a biological, inflammatory response, not psychological.
2. Crushing Fatigue & Energy Depletion
This is a fatigue so profound it defies description. It’s not simply feeling sleepy.
- In Detail: Often described as a “lead blanket” sensation or feeling like your bones are filled with concrete. The energy required to lift a remote control or speak a full sentence can feel insurmountable. This is a pathological exhaustion where the body’s basic energy production systems have shut down. It is not relieved by sleep or rest.
3. Cognitive Dysfunction (“Brain Fog”)
PEM directly impacts brain function, making mental tasks impossible and isolating you from the world.
- In Detail: This goes beyond simple forgetfulness. You may experience:
- Impaired Short-Term Memory: Forgetting what you were saying mid-sentence or why you entered a room.
- Difficulty Processing Information: Struggling to follow the plot of a simple TV show or understand a recipe.
- Word-Finding Problems: Being unable to recall common words, making speech slow and labored.
- Poor Concentration: Being unable to focus on a task for more than a few minutes.
4. Neurological & Sensory Sensitivities
Your nervous system becomes hyper-aroused and overwhelmed by ordinary stimuli.
- In Detail: Everyday environmental input becomes painful or intolerable. Light may feel unbearably bright, forcing you to wear sunglasses indoors. Everyday sounds (like dishes clinking or a conversation in another room) can feel jarring and abrasive. Smells (from perfume, food cooking, or cleaning products) can trigger nausea or headaches.
5. Sleep Disruption & Unrefreshing Sleep
Sleep, the one thing that should help, becomes dysfunctional.
- In Detail: You might struggle with insomnia despite utter exhaustion. More commonly, you may sleep for 10, 12, or even 14 hours and wake up feeling completely unrefreshed, as if you hadn’t slept at all. This is a hallmark of ME/CFS and is severely exacerbated during PEM.
6. Orthostatic Intolerance
Your body has trouble regulating blood flow, especially when you are upright.
- In Detail: Upon standing, you may feel a sudden wave of dizziness, lightheadedness, or vertigo. Your heart may race or palpitate (POTS is a common co-condition). You might feel faint, nauseous, or have blurred vision. This often forces you to lie down immediately.
7. Pain and Weakness
A deep, pervasive physical discomfort is common.
- In Detail: This can include widespread muscle pain, joint pain without swelling or redness, and a significant loss of muscle strength, making your limbs feel weak, shaky, or unstable.
Key Takeaway: The combination, severity, and prominence of these symptoms create the unique “face” of your PEM crash. One episode might be dominated by crushing fatigue and brain fog, while another might be characterized by severe flu-like symptoms and pain. Recognizing this full spectrum is the first step toward connecting your activities to their consequences and validating the very real, physiological nature of your experience.
Your Personal PEM Trigger Checklist: What to Look For
The most challenging aspect of PEM is that triggers are highly individual. What causes a crash in one person may be manageable for another. The key is to think beyond strenuous exercise. Triggers often fall into several categories.
1. Physical Exertion Triggers
This is the most widely recognized category, but the level of activity can be surprisingly low.
- Obvious Triggers: Grocery shopping, walking for more than a few minutes, household chores like vacuuming or cleaning.
- Subtle Triggers: Taking a shower (the standing and temperature changes), getting dressed, cooking a simple meal, brushing your hair.
2. Cognitive Exertion Triggers
Mental activity requires significant energy and can be just as draining as physical tasks.
- Examples: Concentrating on work or studies, reading a complex book, having a long conversation, making decisions, managing finances, playing strategic games.
3. Emotional and Sensory Triggers
This category is often overlooked but can be incredibly potent.
- Emotional Exertion: Stress, anxiety, excitement (even positive events), arguments, or emotional conversations.
- Sensory Input: Exposure to loud noises, bright or flickering lights, strong smells (perfume, chemicals, cooking odors).
4. Other Potential Triggers
- Illness: Fighting off a common cold or infection.
- Weather Changes: Shifts in barometric pressure, extreme heat or cold.
How to Spot Your Unique Triggers: The Power of the PEM Diary
If managing ME/CFS is like being a detective on a complex case, then your PEM Diary is your most crucial piece of evidence. It transforms vague feelings of “I overdid it” into clear, actionable data. Because of the delayed nature of PEM (12-48 hours), our brains are not wired to connect Tuesday’s errands with Thursday’s collapse. A journal bridges this gap, revealing the hidden patterns that govern your energy.
Think of it not as a chore, but as a tool for empowerment—your personal roadmap to a more stable life.
Step 1: Choosing Your Tool and Setting a Routine
- Tool Options: Choose a method that feels easiest for you.
- Notebook: Simple and accessible. Create a simple table with columns for each element below.
- Digital Spreadsheet (Excel/Google Sheets): Highly recommended. It allows you to easily sort, filter, and visualize your data over time.
- App: Some people use habit-tracking apps, notes apps, or dedicated symptom tracker apps.
- Routine: The key is consistency. Set a reminder to spend just 5 minutes each evening filling it out. Brief, daily entries are far more sustainable and useful than long, infrequent ones.
Step 2: What to Record – The Three Core Components
Your diary should capture three interconnected areas: Activities, Exertion, and Symptoms.
1. Record Daily Activities in Detail: The “What”
Go beyond the obvious. The triggers for PEM are often hidden in “minor” daily tasks. Be specific.
- Physical: Showering, getting dressed, preparing a meal, walking to the mailbox, folding laundry, standing for 5 minutes.
- Cognitive: Reading, writing emails, paying bills, having a phone call, making decisions, concentrating on a TV show.
- Social/Emotional: A visitor coming over, a stressful news item, a joyful but exciting event, a difficult conversation.
- Sensory: Exposure to loud noises (e.g., a vacuum cleaner), bright lights, or strong smells.
2. Rate Your Exertion: The “Cost”
For each significant activity, assign two exertion scores on a scale of 1-10. This quantifies the “energy cost.”
- Physical Exertion (1-10): How demanding was this on your body?
- *1 = Minimal (lying in bed watching TV)*
- *5 = Moderate (preparing a simple meal while sitting down)*
- *10 = Maximum (Unable to do; would cause immediate collapse)*
- Mental/Cognitive Exertion (1-10): How demanding was this on your brain?
- *1 = Minimal (listening to calming music)*
- *5 = Moderate (having a light conversation)*
- *10 = Maximum (taking a timed test, managing a crisis)*
3. Track Symptoms Faithfully: The “Result”
Each day, log the severity of your key symptoms. You can use a simple scale like Mild (1), Moderate (2), Severe (3), or a 1-10 scale.
- Core Symptoms to Track: Fatigue, Brain Fog, Pain (muscle/joint), Flu-like feelings (sore throat, etc.), Sleep Quality, Orthostatic Intolerance (dizziness).
- Notes Section: Jot down anything unusual. e.g., “Woke up at 3 AM with heart racing,” or “Couldn’t find words during afternoon call.”
Putting It All Together: A Sample Diary Entry
| Date | Activities & Exertion Ratings (P=Physical, M=Mental) | Symptoms (Scale 1-3) & Notes |
|---|---|---|
| Monday | AM: Showered (P:7, M:2), Made tea & toast (P:4, M:3). PM: 20-min phone call with friend (P:1, M:6). Watched a movie (P:1, M:4). | Fatigue: 2, Brain Fog: 1, Pain: 2. Felt relatively okay today. |
| Tuesday | AM: Doctor’s appointment (drive, waiting room, talking) (P:8, M:9). PM: Crashed on couch, rest only. | Fatigue: 3, Brain Fog: 3, Pain: 3, Flu-like: 2. Sore throat started. Severe crash. Can’t think. |
| Wednesday | Total rest day. Only got up for bathroom. | Fatigue: 3, Brain Fog: 2, Pain: 3. Still in crash. Unrefreshing sleep. |
Step 3: Analyze for Patterns: Becoming Your Own Detective
After 2-4 weeks, review your journal. Look backward from your crash days.
- Ask Key Questions:
- “What did I do 24-48 hours before this crash?”
- “Was there a combination of activities that pushed me over the edge?” (e.g., The doctor’s appointment on Tuesday combined physical travel, mental concentration, and emotional stress).
- “What is my baseline on a ‘good’ day? What activities can I do without causing a crash?”
From Data to Action: Using Your Findings for Pacing
The ultimate goal of the PEM Diary is not just to identify triggers, but to redefine your “Energy Envelope.”
- Establish Your Baseline: Discover the total amount of physical and mental exertion you can handle in a day without triggering PEM.
- Plan and Pace: Use this knowledge to plan your week. Space out demanding activities. Schedule mandatory rest before and after known triggers.
- Communicate with Your Doctor: Bring your diary to appointments. It provides objective evidence of your disability and the impact of PEM, which can be invaluable for diagnosis and management.
By faithfully keeping a PEM Diary, you shift from being a passive victim of your symptoms to an active manager of your health. It is the single most powerful tool for learning to live within your energy limits and reduce the frequency and severity of devastating crashes.
Strategies to Avoid Triggers and Manage Your Energy
Identifying your triggers through a PEM diary is the first half of the battle. The second, more crucial half, is implementing proactive strategies to navigate your life within your body’s strict energy limits. This practice is known as pacing, and it is the cornerstone of managing ME/CFS. It’s not about curing the illness, but about preventing the devastating PEM crashes that worsen your baseline over time.
Think of pacing as a continuous process of budgeting your most valuable currency: your energy.
1. Master Your Energy Envelope: The Golden Rule
Your “Energy Envelope” is the finite amount of physical and cognitive energy you can spend in a day without triggering PEM. The goal is to live within this envelope, not constantly test its limits.
- How to Define It: Use your PEM Diary to find your baseline. On days that were not followed by a crash, what was the total amount and type of activity you did? That is your current energy envelope. It is not a goal to exceed; it is a ceiling to respect.
- Practical Application: If your diary shows that a 10-minute shower, preparing one simple meal, and a 15-minute phone call is your safe limit, then that is your budget for a “active” day. Any additional activity, like an unexpected visitor, means you must subtract another activity to stay within budget.
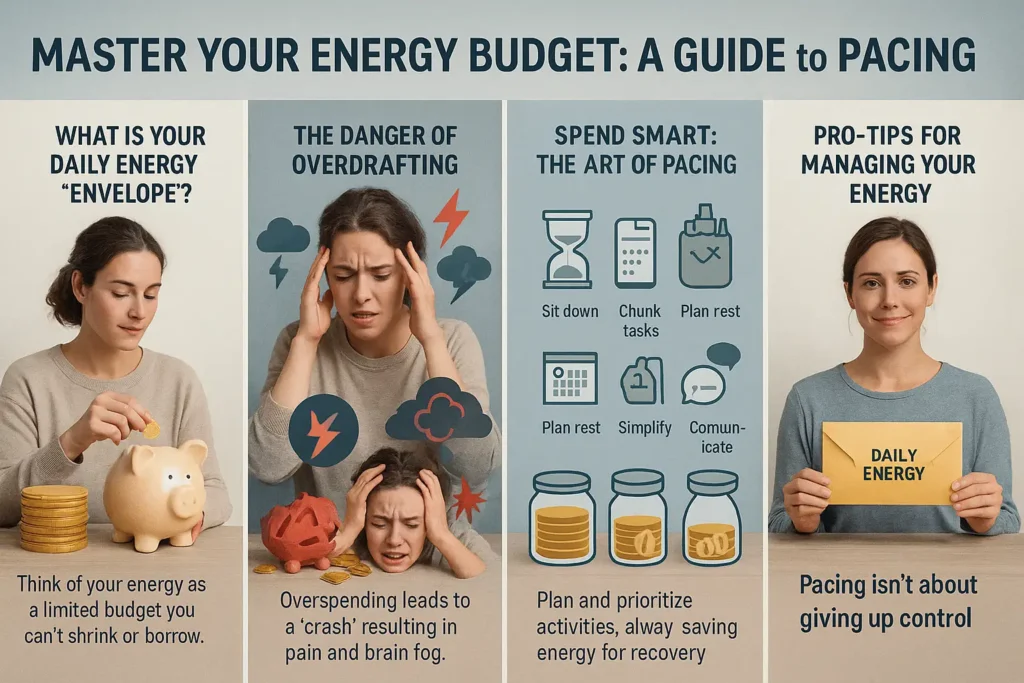
2. The Power of Strategic Rest: Proactive, Not Reactive
Rest is not a reward for exhaustion; it is a vital tool to be used strategically throughout the day to conserve energy.
- Scheduled Rest Breaks: Plan rest before, during, and after any activity.
- Before: Rest for 20-30 minutes before a known activity, like a doctor’s appointment.
- During: Break tasks into “chunks.” For example, instead of tidying the whole living room, rest for 15 minutes after putting away the books.
- After: Following any significant exertion, schedule a “rest day” or a day of significantly reduced activity. This is non-negotiable for PEM prevention.
- What is True Rest? This means activities that require minimal physical and mental energy: lying down in a quiet, dark room; listening to calming music without focusing; gentle breathing exercises. Scrolling on your phone or watching an intense TV show is not restful for the brain.
3. Simplify and Adapt: Redefining “Normal”
The key to conserving energy is to relentlessly eliminate unnecessary exertion from daily tasks. This is not about giving up, but about smart adaptation.
- Physical Simplification:
- Seated Everything: Use a shower chair in the bathroom. Sit on a stool while cooking or washing dishes.
- Reduce Steps: Keep a water bottle and snacks by your bed or sofa. Use a rolling cart to move items around the house.
- Online Services: Utilize grocery delivery, online shopping, and automatic bill pay to conserve colossal amounts of cognitive and physical energy.
- Cognitive Simplification:
- Use Technology: Set reminders and alarms for everything (medications, appointments) to conserve mental RAM.
- Limit Decisions: Simplify your wardrobe or meal planning to reduce decision fatigue.
- Communicate in Writing: For complex conversations, use text or email instead of verbal discussions, which can be more draining.
4. Plan and Pace Your Week: The “Boom and Bust” Antidote
A common pattern is doing too much on a “good day” (boom), leading to a crash (bust). Pacing flattens this cycle.
- Create a Weekly Plan: At the start of the week, look at your commitments. If you have a necessary, high-energy task on Wednesday (e.g., a medical appointment), intentionally schedule Monday and Tuesday as very light days, and block out Thursday and Friday for mandatory rest. Spread activities out. What a healthy person might do in one day, you might need to spread over three or four.
5. Communicate Your Needs Clearly and Confidently
Your health depends on setting boundaries. This requires clear communication with friends, family, and healthcare providers.
- Use a Medical Explanation: Frame your limits in terms of your illness. Instead of “I’m too tired to visit,” try: “I have to manage my energy very carefully to avoid a serious symptom flare-up called PEM. A long visit would be medically harmful for me, but a short 20-minute visit would be wonderful.”
- Offer Alternatives: Suggest manageable alternatives. “I can’t go out to dinner, but I’d love it if you could come over for a quiet cup of tea for half an hour.”
- Be a Broken Record: You may need to repeat your explanations. Remember that protecting your health is your top priority.
A Final Note on Setbacks: Pacing is a skill that takes time to learn. You will have setbacks. The goal is not perfection, but progress. When you do crash, return to your PEM diary. Analyze what happened, adjust your understanding of your energy envelope, and refine your strategies. This is a lifelong journey of listening to your body with profound respect. By mastering these strategies, you take back a measure of control and create a more stable and predictable life.
A Final Word: Empowerment Through Understanding
Managing ME/CFS is a lifelong journey of listening to your body with profound attention. By learning to spot and avoid your personal PEM triggers, you move from being a passive victim of crashes to an active manager of your health. This process is not about giving up activities, but about strategically conserving energy so you can have a more predictable and stable quality of life. Remember, fearing PEM is not a phobia; it is a rational response to a very real physiological consequence. Your experience is valid, and with careful observation, you can learn to navigate life with ME/CFS more safely.
Helpful Resources & Further Reading
- Solve M.E. – For research, advocacy, and patient support: solvecfs.org
- ME Action – Global network for news and advocacy: meaction.net
- Bateman Horne Center – Expert clinical resources on PEM and ME/CFS: batemanhornecenter.org
- PEM Activity Log (Workwell Foundation) – A practical diary for tracking triggers: Download PDF
- The Spoon Theory – A simple way to explain energy limitation: Read the Essay
Important Disclaimer:
This information is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Management strategies should be discussed with a healthcare provider familiar with ME/CFS.