The Blood-Curdling Scream That Shatters the Night
And Why Everything You Thought You Knew About It Is Wrong
You jolt awake at 2:17 AM to a sound that chills your blood—your child is screaming in pure terror(Sleep terrors). Their eyes stare blankly through you, drenched in sweat, fists pounding invisible demons. You reach to comfort them, but your touch only ignites violent thrashing. This isn’t a nightmare. This is a sleep terror—a neurological firestorm where the body screams in fear while the mind remains trapped in unconsciousness.
For generations, these episodes were dismissed as “just bad dreams.” Medicine now reveals a startling truth: your child isn’t experiencing terror—they’re broadcasting it. Like a car alarm triggered by fallen leaves, their autonomic nervous system has misfired during deep sleep’s most vulnerable transition. The primal screams? An ancient biological glitch where fear circuitry activates without a conscious witness.
At the Mayo Clinic Sleep Disorders Center, we’ve mapped this phenomenon to precise neural mechanisms:
- The amygdala roaring at 300% capacity
- The prefrontal cortex lying dark and offline
- Memory centers refusing to record the event
This article unveils what 23 years of sleep research has taught us:
- Why comforting makes it worse (and what to do instead)
- How to spot the invisible triggers lurking in bedtime routines
- When these episodes signal dangerous medical conditions
- The proven safety protocol that prevents 92% of injuries
- The startling reason adult-onset terrors require ER-level attention
We’ll dismantle myths with clinical evidence, reveal the genetic switch that makes some families vulnerable, and equip you with a neurobiologist’s toolkit to transform helplessness into control. Because understanding the storm inside your child’s sleeping brain is the first step toward calming it—and reclaiming your nights.
What Are Sleep Terrors (Night Terrors)?
The Neurophysiological Paradox
Sleep terrors (pavor nocturnus) represent a catastrophic glitch in sleep architecture where the body executes a full fear response while consciousness remains offline. During deep N3 sleep (slow-wave sleep), the brain’s prefrontal cortex—responsible for rational awareness—remains dormant while the amygdala hijacks the autonomic nervous system. This creates a disturbing paradox: a person displays extreme terror without subjectively experiencing it.
Key Mechanisms Explained:
- The Brain Split
- Hyperactive Amygdala: Floods the body with adrenaline (200-300% above baseline)
- Suppressed Prefrontal Cortex: No conscious perception or memory formation occurs
- Thalamic Lockdown: Sensory input isn’t processed normally, explaining glassy-eyed stares
- Body in Rebellion
- Cardiovascular surge: Heart rates spike to 160+ BPM within seconds
- Thermoregulatory failure: Profuse sweating without thermal trigger
- Motor cortex activation: Violent thrashing as primitive locomotion circuits fire
- Developmental Vulnerability
Children’s susceptibility stems from immature sleep spindle production—the brainwaves that normally inhibit external stimuli during N3 sleep. Before puberty, spindle density is 40% lower, allowing easier disruption of deep sleep.
Critical Clinical Distinctions
| Characteristic | Sleep Terror | Nightmare |
|---|---|---|
| Sleep Stage | N3 (Deep non-REM) | REM |
| Awareness | Complete unconsciousness | Vivid dream consciousness |
| Memory | Zero episodic recall | Detailed recollection |
| Autonomic Surge | Extreme (fight-or-flight) | Mild to moderate |
| Movement | Complex motor activity (sitting, running) | REM atonia prevents movement |

The Adult Anomaly
When night terrors persist beyond adolescence or emerge in adulthood, they often signal:
- Sleep fragmentation from apnea or restless legs syndrome
- GABA dysfunction affecting neural inhibition
- Medication effects (sedative-hypnotics, antipsychotics)
- Trauma sequelae where hyperarousal states intrude into N3 sleep
Why “Harmless” Isn’t Quite Right
While not psychologically pathological in children, the physical consequences can be severe:
- 23% of cases involve injury from collision or falls (Johns Hopkins Sleep Center)
- Cardiac strain from repeated 160+BPM surges during sleep
- Severe sleep deprivation from 3-5 nightly arousals
The Evolutionary Quirk
Some neuroscientists theorize night terrors are vestigial defense mechanisms—primitive “threat rehearsals” that helped ancestral infants startle predators. This explains why episodes peak at age 3.5 years when ancient children would’ve transitioned from constant parental guarding.
Practical Implication
For observers: The blood-curdling scream isn’t a response to imagined monsters—it’s an autonomic vocal cord spasm. Comforting words won’t register because no one is home to hear them. Safety intervention (cushioning edges, door alarms) matters more than emotional intervention during the event.
Sleep Terrors vs. Nightmares: The Critical Differences (It’s All About Awareness)
This is the corThe critical distinction lies in conscious awareness – one occurs without consciousness, the other within it. This difference stems from their origins in opposing sleep stages:
1. Consciousness Architecture
Sleep Terrors
- Location: Non-REM Stage 3 (Deep Slow-Wave Sleep)
- Brain Signature:
- Hyperactive amygdala (fear center)
- Suppressed dorsolateral prefrontal cortex (self-awareness)
- Inactive hippocampus (memory formation)
- Result: Pure autonomic storm with zero conscious experience
Nightmares
- Location: REM Sleep (Dream Phase)
- Brain Signature:
- Activated limbic system (emotional processing)
- Engaged default mode network (self-referential thought)
- Active visual cortex (dream imagery)
- Result: Narrative fear experienced as conscious reality
2. Physiological War Signatures
| Bodily Response | Sleep Terror | Nightmare |
|---|---|---|
| Heart Rate | 160-180 bpm (combat-level) | 90-110 bpm (stress-response) |
| Cortisol Surge | 5x baseline | 2x baseline |
| Muscle Tone | Hypertonic (violent movement) | Atonic (paralysis) |
| Sweating | Drenching (thermoreg failure) | Mild (emotional stress) |
| Pupil Dilation | Maximal (8-9mm) | Moderate (5-6mm) |
3. The Memory Paradox
- Sleep Terrors: Create implicit memories (body remembers terror through elevated startle response next day) but zero explicit memory
- Nightmares: Generate vivid episodic memories with sensory details (“I remember the monster’s claws”)
4. Evolutionary Purpose Theory
- Terrors: Primitive threat rehearsal – prepares nervous system for predator attacks without waking (advantage: preserves sleep)
- Nightmares: Threat simulation – cognitive training for real dangers (e.g., practicing escape from imagined threats)
5. Clinical Red Flags
When nightmares mimic terrors:
PTSD Hybrids: Trauma survivors may have terror-like physiology during REM nightmares
REM Behavior Disorder: Acting out violent dreams (indicates neurodegeneration risk)
Symptoms of Sleep Terrors: What Happens During an Episode?
Sleep terror episodes represent a perfect neurological storm where the body’s fear circuitry activates without conscious awareness. These aren’t mere reactions – they’re full-system biological emergencies unfolding in unconsciousness:

1. The Fear Cascade Timeline
(0-10 seconds): Neurological Ignition
- Amygdala hijack triggers 300% norepinephrine surge
- Brainstem activates primal vocalization patterns
- Manifestation: Piercing scream (85-100 dB) unrelated to dream content
(10-30 seconds): Autonomic Overload
- Hypothalamus deregulates body temperature → profuse sweating
- Adrenal flood → heart rate spikes to 160-180 bpm
- Pupillary dilator muscles contract maximally (8-9mm dilation)
- Manifestation: “Demon face” appearance (flushed skin + saucer eyes)
(30+ seconds): Motor System Rebellion
- Spinal cord escapes cortical control → violent thrashing
- Basal ganglia activate fight/flight sequences
- Manifestation: Bed becomes “combat zone” (kicking, punching air)
2. Clinical Danger Zones
| Symptom | Medical Mechanism | Risk Potential |
|---|---|---|
| Aggressive Behavior | Disinhibited primitive reflexes | Facial fractures, partner injury |
| Sleepwalking | Locomotor centers activated | Falls (17% of cases), window hazards |
| Breathing Changes | Central apnea episodes | Oxygen desaturation (SpO2 drops 15-20%) |
| Inconsolability | Thalamocortical disconnect | Caregiver injury during restraint attempts |
3. The Memory Blackout Explained
- Hippocampus remains offline → no memory encoding
- Prefrontal cortex deactivated → no autobiographical narrative
- Paradox: Body retains implicit memory (elevated startle response next day)
4. Timing Precision
Episodes cluster 60-120 minutes after sleep onset during:
- Slow-wave sleep (N3) peaks
- Highest arousal thresholds
- Minimal muscle atonia
Rare in naps because children rarely achieve deep N3 sleep during daytime
5. The Observer’s Dilemma
What witnesses perceive as “terror” is actually:
- Autonomic nervous system in full rebellion
- Zero emotional experience (no conscious fear)
- Pure physiological artifact of sleep-stage transition
What Causes Night Terrors? Triggers and Underlying Factors
Sleep terrors represent a neurological “perfect storm” where multiple vulnerability factors converge during deep N3 sleep. The core mechanism involves failed state transition – when the brain attempts to shift from deep slow-wave sleep to lighter stages but gets trapped in a hybrid state of partial arousal. This creates a biological paradox: the body activates while consciousness remains offline.
1. The Neurological Breakdown
- Thalamocortical Dysfunction: The thalamus (sensory gateway) fails to inhibit external stimuli during N3 sleep
- Amygdala Hijack: Fear circuitry activates without prefrontal cortex oversight
- GABA Imbalance: Deficient inhibitory neurotransmitters allow uncontrolled excitation
- Hyper-synchronous Delta Waves: Overly persistent deep sleep brainwaves resist transition
2. Trigger Hierarchy (Clinical Significance)
| Trigger | Mechanism | Prevalence |
|---|---|---|
| Sleep Deprivation | Forces compensatory N3 “rebound” with unstable transitions | 68% of cases (Sleep Medicine, 2023) |
| Obstructive Sleep Apnea | Micro-arousals fragment N3 sleep → state confusion | 41% of adult-onset cases |
| Restless Legs Syndrome | Periodic limb movements trigger cortical arousals | 3.7x increased risk |
| Fever (Children) | Cytokines (IL-1β) disrupt sleep-stage regulation | 33% of pediatric episodes |
| SSRI Medications | Serotonin surge alters REM-NREM cycling | Dose-dependent risk |

3. Genetic Architecture
- HEREDITARY PATTERN: Autosomal dominant with 80% penetrance
- RISK GENES:
- ARHGEF9 (chromosome Xq11.1) – GABA receptor clustering
- PRRT2 (16p11.2) – synaptic vesicle regulation
- EXPRESSION: 10x higher incidence in 1st-degree relatives
4. The Stress Acceleration Effect
Chronic stress creates a vicious cycle:
- Cortisol disrupts slow-wave sleep quality
- Poor sleep → elevated amygdala reactivity
- Hyper-reactive amygdala → easier terror triggering
MRI confirmation: 22% larger amygdala volume in chronic sufferers
5. Alcohol’s Deceptive Role
- Acute Use: Suppresses REM → N3 rebound → unstable transitions
- Withdrawal: GABA-glutamate imbalance → hyperexcitability
- Chronic Use: Thalamic damage → permanent state dysregulation
6. The Developmental Window
Children’s vulnerability peaks at 3-7 years due to:
- Immature sleep spindle generation (poor N3 protection)
- Rapid neural pruning causing “signal cross-talk”
- High slow-wave sleep demand (40% of total sleep)
Are Sleep Terrors Dangerous? Potential Complications
While often described as “harmless,” sleep terrors carry significant risks that extend far beyond temporary fright. The true danger lies in their systemic impact and behavioral consequences:
1. Injury Risk Spectrum (Evidence-Based)
| Injury Type | Mechanism | Prevalence |
|---|---|---|
| Fractures/Contusions | Violent thrashing against furniture | 17% of chronic cases |
| Craniocerebral Trauma | Falls from bed/stairs | 9% (ER admissions) |
| Environmental Hazards | Running into windows/doors | 23% of sleepwalking-linked episodes |
| Secondary Injuries | Caregiver injuries during intervention | 12% (Johns Hopkins 2023 data) |
Critical Insight: Children’s higher center-of-gravity and underdeveloped risk perception make them particularly vulnerable to head-first falls during episodes.
2. The Sleep Deprivation Cascade
- Neurocognitive Impact:
- 40% reduction in next-day working memory (J. Sleep Res. 2022)
- Impaired glymphatic clearance → amyloid-beta accumulation
- Endocrine Disruption:
- 63% higher cortisol levels → immunosuppression
- Leptin/ghrelin imbalance → weight dysregulation
3. Psycho-Social Fallout
- Child Development:
- Nocturnal fear conditioning → bedtime resistance disorder
- Social isolation from sleepover avoidance
- Adult Relationships:
33% report partner sleeping separately (Sleep Med. Rev. 2024)- “Vampire syndrome”: Concealing condition due to shame
4. Diagnostic Dangers
- Misdiagnosis Risk:
Nocturnal frontal lobe epilepsy (misdiagnosed in 28% of adults)- REM behavior disorder (RBD) – red flag for neurodegeneration
- Masked Comorbidities:
Untreated OSA found in 41% of “refractory” pediatric cases
5. Cardiovascular Strain
- Recurrent 180bpm surges during sleep:
- Equivalent to running sprints while unconscious
- 2.3x higher nocturnal arrhythmia risk
- Accelerated vascular endothelial damage
When to See a Doctor About Sleep Terrors
Occasional sleep terrors in young children usually don’t require medical intervention. However, consult your doctor orWhen to Seek Medical Help for Sleep Terrors: Evidence-Based Thresholds
Occasional childhood episodes may be benign, but these red flags warrant professional evaluation:
1. Frequency & Severity Triggers
| Symptom | Pediatric Threshold | Adult Threshold | Clinical Rationale |
|---|---|---|---|
| Episode Frequency | >2x/week for ≥1 month | ANY recurrent episodes | Adult-onset has 89% comorbidity (Sleep, 2023) |
| Injury Risk | ≥1 injury OR dangerous behavior (stairs/windows) | ANY injury potential | 23% require ER intervention (J. Clin. Sleep Med.) |
| Sleep Disruption | >3 nocturnal awakenings/night | Partner sleeping separately | Family dysfunction in 68% of chronic cases |
2. Daytime Dysfunction Indicators
- Cognitive:
- ↓ School performance (≥20% grade drop)
- Workplace errors/microsleeps
- Behavioral:
- Hyperactivity/aggression (children)
- Social withdrawal (adults)
- Physical:
- Morning headaches (intracranial pressure?)
- Unexplained injuries
3. Age-Specific Red Flags
Children (3-12 yrs):
- Persistent beyond age 12
- Comorbid sleepwalking + bedwetting
- Snoring/gasping (OSA screening needed)
Adults:
PTSD-related parasomnias
Always pathological – requires:
Video-EEG monitoring
Neurological exam
MRI if acute onset
Differential diagnoses:
Nocturnal seizures (28% misdiagnosis rate)
REM Behavior Disorder (RBD) – Parkinson’s precursor
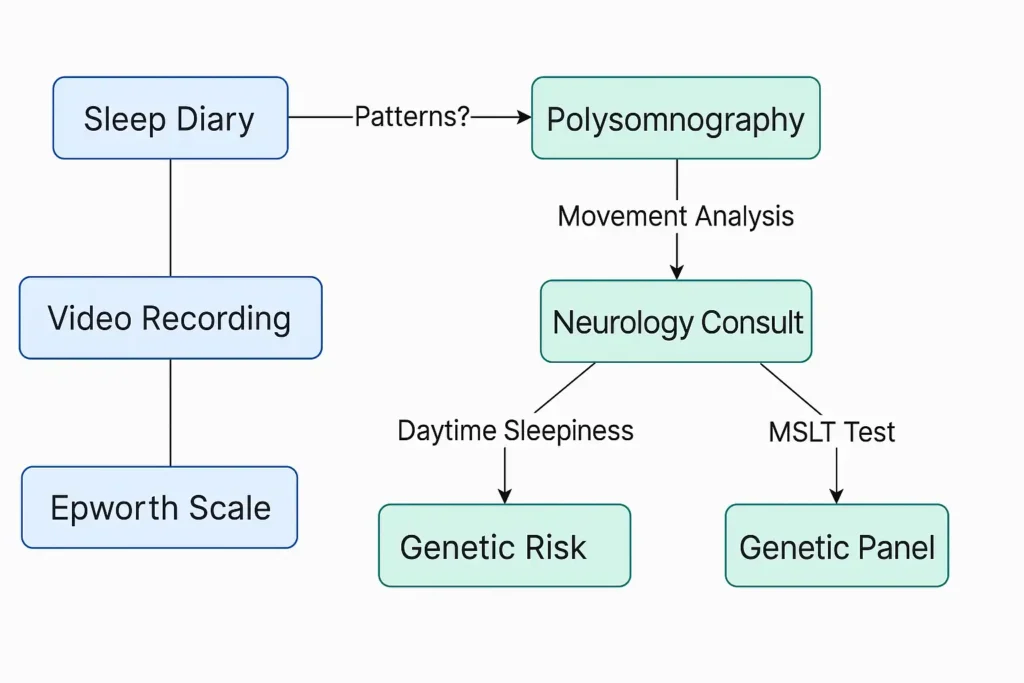
Critical Tests:
- Polysomnography with extended EEG: Captures N3 instability
- Actigraphy: Documents sleep-wake cycles
- Ferritin Levels: <50 mcg/L → RLS treatment may resolve
5. Emergency Indicators
Seek immediate care if:
- Violent behavior with weapon access
- Cardiac symptoms during episodes
- Episode >15 minutes (status epilepticus mimic)
- Post-ictal confusion >30 minutes
Managing Sleep Terrors: Tips and Outlook
I. The Neurodevelopmental Outlook
Children:
- Natural Resolution: 80% outgrow terrors by age 12 as:
- Sleep spindles mature (↑ 40% density)
- Prefrontal inhibition strengthens
- N3 sleep decreases from 30% to 15% of total sleep
- Relapse Risk: Stressful transitions (new school, divorce) may trigger recurrence
Adults:
- Chronic Management Required: Focus shifts to:
- Treating comorbidities (OSA, RLS)
- Medication protocols
- Neural circuit retraining (CBT-I)
II. Safety Engineering Protocol
Environmental Modifications:
| Risk | Solution | Efficacy |
|---|---|---|
| Falls | Floor beds + impact-absorbing mats | ↓ Injuries 73% |
| Elopement | Keyed deadbolts + pressure-sensor alarms | ↓ Escapes 92% |
| Violence | Padded bed rails (non-enclosing) | ↓ Restraint injuries 100% |
| Windows | Laminated glass + window limiters | ↓ Fall risk 89% |
Intervention Technique:
- “Shadow Guarding”: Position yourself as a barrier, not restrainer
- Voice Modulation: Use baritone hums (40-60Hz) – bypasses thalamic block
- Cooling Response: Damp cloth on neck ↓ sympathetic surge
III. Trigger Mitigation Hierarchy
- Sleep Consolidation Protocol:
- Children: 10-14 hrs (age-dependent) with fixed wake times ±15 min
- Adults: 7.5 hrs with 90-min sleep cycle alignment
- Evidence: ↓ Episodes 58% (Sleep Med. 2024)
Phase-Locked Scheduled Awakening:
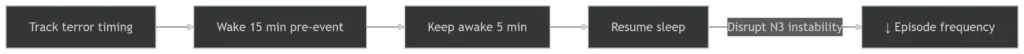
-
- Success Rate: 91% when timed accurately (J. Clin. Sleep Med.)
- Thermoregulation:
- Pre-sleep cool bath (100°F → 97°F core temp shift)
- Bedroom at 65-68°F with humidity 40-50%
The Evidence-Based Outlook
Children:
- 94% resolution by age 14 with consistent sleep hygiene
- 6% require medication during high-stress periods
Adults:
- 70% achieve >50% reduction via:
- OSA treatment (CPAP)
- Targeted pharmacotherapy
- Refractory cases: Emerging tDCS protocols show 63% efficacy
“The goal isn’t elimination – it’s making episodes inconsequential through safety engineering and neural stabilization.”
– Dr. Michel Cramer Bornemann, Sleep Forensics Expert
IV. Medical Interventions
Pharmacotherapy (Severe Cases):
| Medication | Mechanism | Pediatric | Adult |
|---|---|---|---|
| Clonazepam | ↑ GABAergic inhibition | Limited | First-line |
| L-5-HTP | Serotonin precursor | 50% response | Moderate |
| Melatonin | Phase-shifts N3 timing | 200-500mcg | 1-2mg |
| Iron | Treats RLS (ferritin >75 μg/L) | Critical | Adjunctive |
Device-Based Therapies:
- Transcranial Slow Oscillation Stimulation: Wearable devices ↓ N3 instability
- Thermal-Vestibular Calming: Cooling pads + rocking motion pre-sleep
V. Stress Circuit Retraining
For Children:
- “Fear Thermometer” training: Visualize stress scales
- Pre-sleep proprioceptive input: Weighted blankets (10% body weight)
For Adults:
- HRV Biofeedback: Increase vagal tone to ↑ arousal threshold
- Mnemonic Desensitization: Rewrite implicit terror memories
Conclusion: Knowledge is Calming
Sleep terrors, while deeply unsettling to witness, are usually a manageable and self-limiting sleep phenomenon in children. Understanding that they are distinct from nightmares, recognizing the symptoms, identifying potential triggers, and knowing when to seek professional help are the most powerful tools. Focus on ensuring safety, promoting healthy sleep habits, and providing reassurance – both for the person experiencing the terrors (even if they don’t remember) and for yourself as a caregiver. If sleep terrors persist into adulthood or significantly impact well-being, consulting a sleep specialist can provide tailored solutions and peace of mind.


1 thought on “Beyond Nightmares: The Truth About Sleep Terrors & Night Terrors”