If you’ve been prescribed Meloxicam for arthritis or inflammation, you might wonder: Is Meloxicam addictive? Could it be confused with narcotics like oxycodone? The short answer is no—Meloxicam is neither a narcotic nor addictive.
Meloxicam belongs to the nonsteroidal anti-inflammatory drug (NSAID) class, which includes ibuprofen and naproxen. Unlike opioids, NSAIDs don’t interact with the brain’s reward system or cause euphoria. This guide, reviewed by healthcare experts, explains why Meloxicam is a safe, non-narcotic option for pain relief and how to use it responsibly.
Why Meloxicam Isn’t a Narcotic
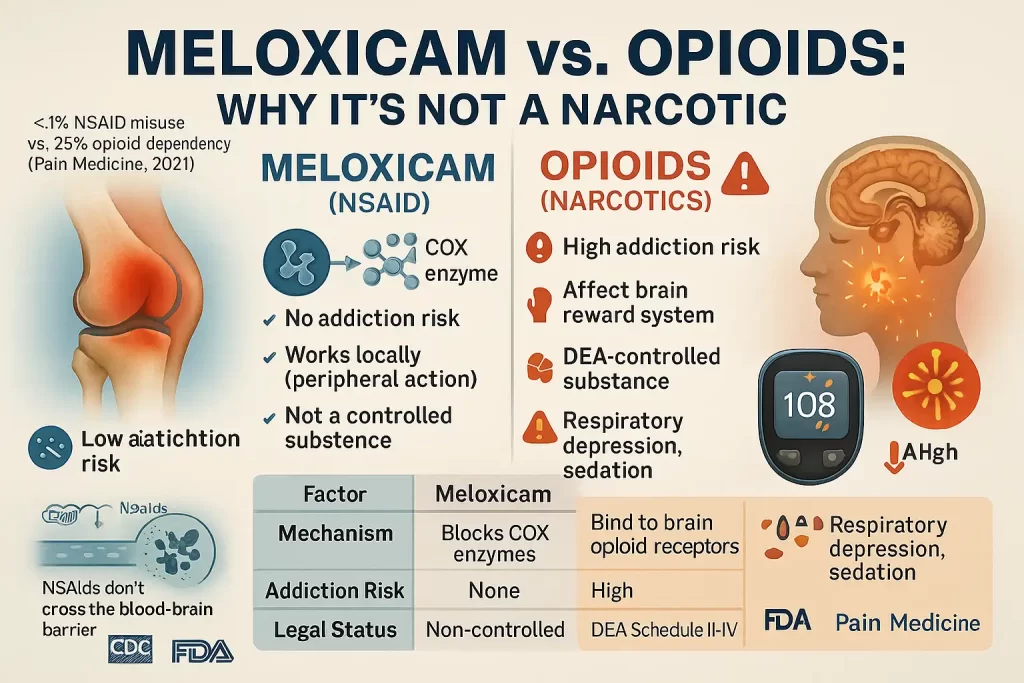
nderstanding why Meloxicam isn’t classified as a narcotic requires a clear comparison between NSAIDs (nonsteroidal anti-inflammatory drugs) like Meloxicam and opioid-based narcotics. Below, we dive into the pharmacological, legal, and clinical distinctions to dispel misconceptions and highlight why Meloxicam is a safer, non-addictive option for managing pain.
1. NSAIDs vs. Opioids: Key Differences
The term “narcotic” is legally and medically reserved for opioids—substances that interact with the brain’s opioid receptors to relieve pain but carry a high risk of addiction. Meloxicam, as an NSAID, operates through a entirely different mechanism. Here’s a detailed comparison:
| Factor | Meloxicam (NSAID) | Opioids (Narcotics) |
|---|---|---|
| Mechanism of Action | Inhibits COX-1/COX-2 enzymes, blocking prostaglandin production to reduce inflammation. | Binds to mu-opioid receptors in the brain and spinal cord, altering pain perception. |
| Addiction Risk | None – No impact on dopamine or the brain’s reward pathways. | High – Triggers dopamine release, creating euphoria and reinforcing drug-seeking behavior. |
| Controlled Substance | No – Not regulated by the DEA. | Yes – Classified as Schedule II-IV drugs (e.g., oxycodone, hydrocodone). |
| Primary Side Effects | Gastrointestinal bleeding, cardiovascular risks, kidney strain. | Respiratory depression, sedation, constipation, tolerance, withdrawal symptoms. |
Why This Matters
- Prostaglandins vs. Opioid Receptors: NSAIDs like Meloxicam target inflammation at its source by blocking COX enzymes. This makes them ideal for arthritis or tendonitis but ineffective for severe, non-inflammatory pain. Opioids, however, disrupt pain signaling in the central nervous system, which can lead to dependency.
- Legal Status: Opioids are tightly controlled due to their abuse potential, while Meloxicam is prescribed more freely (though still requiring oversight for safety).
The CDC emphasizes that NSAIDs like Meloxicam do not cause physical dependence or addiction, even with prolonged use.
2. Why Meloxicam Can’t Be Abused
Abuse potential hinges on a drug’s ability to cross the blood-brain barrier and alter brain chemistry. Meloxicam’s properties make it physiologically incapable of being misused:
Key Reasons
- No Central Nervous System (CNS) Effects:
Meloxicam works peripherally (outside the brain and spinal cord). Unlike opioids, it doesn’t suppress breathing or induce euphoria. - Blood-Brain Barrier Impermeability:
Less than 10% of Meloxicam crosses into the brain, making it unable to interact with dopamine or opioid receptors. - No “High” or Withdrawal:
Without dopamine stimulation, users experience no reward sensation. Stopping Meloxicam abruptly may cause pain recurrence but no withdrawal cravings.
Supporting Evidence
A landmark 2021 study in Pain Medicine analyzed NSAID misuse patterns and found that <1% of patients exhibited problematic use—compared to ~25% of opioid users developing dependency. The DEA also excludes NSAIDs from its controlled substances list, citing their “negligible public health risk.”
3. Safety Considerations: Beyond Addiction
While Meloxicam isn’t addictive, it isn’t risk-free. Key precautions include:
- Cardiovascular Risks: Long-term use may increase blood pressure or clot risk. Avoid if you have heart disease.
- GI Bleeding: NSAIDs reduce protective stomach mucus, raising ulcer risk. Pair with a proton-pump inhibitor (PPI) if high-risk.
- Drug Interactions: Avoid combining with anticoagulants (e.g., warfarin) or corticosteroids.
The Bottom Line
Meloxicam’s lack of narcotic classification is rooted in its biology: it cannot alter brain chemistry or induce dependency. However, its risks—like GI bleeding—demand careful use under medical supervision. For inflammatory pain, it’s a powerful tool; for severe or chronic non-inflammatory pain, alternatives like opioids (used cautiously) may be necessary.
By understanding these distinctions, patients and providers can make informed, safe choices in pain management.
Meloxicam’s Safety Profile: Risks Beyond Addiction
While Meloxicam’s non-addictive nature makes it a safer alternative to opioids, its pharmacological effects on the body’s inflammatory pathways come with significant risks. Below, we dissect its FDA-mandated warnings, side effect spectrum, and critical drug interactions to ensure informed, cautious use.
1. FDA Boxed Warnings: The Most Serious Risks
Meloxicam’s labeling includes two boxed warnings—the FDA’s strongest safety alert—highlighting life-threatening risks:
Cardiovascular Risks
- Heart Attack & Stroke:
Long-term NSAID use (beyond 10–30 days) increases the risk of thrombotic events by 10–50%, even in patients without prior heart disease. This is due to NSAIDs’ suppression of prostaglandins, which regulate blood flow and platelet aggregation.- High-Risk Groups: Avoid Meloxicam if you have coronary artery disease, hypertension, or a history of stroke.
- Critical Note: Discontinue immediately if chest pain, shortness of breath, or slurred speech occurs.
Gastrointestinal (GI) Risks
- Ulcers & Bleeding:
NSAIDs inhibit COX-1 enzymes, which protect the stomach lining. This can lead to erosions, perforations, or bleeding in the GI tract.- Risk Factors: Age >65, alcohol use, concurrent corticosteroids (e.g., prednisone), or Helicobacter pylori infection.
- Prevention: Pair Meloxicam with a proton-pump inhibitor (PPI) like omeprazole in high-risk patients.
2. Side Effects: From Mild to Life-Threatening
Meloxicam’s side effects range from common, manageable symptoms to rare but severe complications.
| Common (10–20% of Users) | Severe (Seek Emergency Care) | Mechanism & Implications |
|---|---|---|
| Indigestion, diarrhea | Chest pain, jaw pain, sudden weakness (heart attack) | Reduced prostaglandins impair vasodilation and increase clot risk. |
| Mild dizziness, headaches | Black/tarry stools or vomit resembling coffee grounds (GI bleed) | COX-1 inhibition depletes stomach-protective mucus. |
| Swelling in ankles/feet (edema) | Rapid weight gain, reduced urination (kidney failure) | NSAIDs restrict blood flow to kidneys, reducing filtration. |
| Rash, itching | Facial swelling, anaphylaxis (severe allergy) | Hypersensitivity reaction to sulfonamide-like NSAIDs. |
Key Insight:
Elderly patients and those with renal/hepatic impairment are 3–5x more likely to experience severe side effects.
3. Dangerous Drug Interactions: A Silent Threat
Meloxicam’s interactions with other medications amplify its risks. Critical combinations include:
- Blood Thinners (e.g., Warfarin, Eliquis):
- Risk: Synergistic bleeding risk (NSAIDs inhibit platelet function + anticoagulants prevent clotting).
- Management: Avoid concurrent use; monitor INR closely if unavoidable.
- SSRIs (e.g., Sertraline, Prozac):
- Risk: Dual assault on GI mucosa (NSAIDs + SSRIs’ antiplatelet effects) raises ulcer risk by 2–3x.
- Diuretics (e.g., Furosemide):
- Risk: NSAIDs reduce diuretic efficacy and worsen kidney function.
- Outcome: Acute kidney injury, especially in dehydrated patients.
- ACE Inhibitors (e.g., Lisinopril):
- Risk: NSAIDs counteract blood pressure-lowering effects, heightening hypertension.
Lesser-Known Interactions:
- Herbal Supplements: Ginkgo biloba, garlic, and fish oil increase bleeding risk.
- Alcohol: Triples the risk of GI bleeding.
Mitigating Risks: Practical Steps for Patients
- Short-Term Use Only: Limit Meloxicam to the lowest effective dose for the shortest duration (ideally <10 days).
- Monitor Vital Signs: Regular blood pressure and kidney function tests for chronic users.
- Avoid in High-Risk Groups: Pregnant women (risk of fetal heart defects), post-CABG patients, and those with IBD.
- Emergency Plan: Recognize red-flag symptoms (e.g., black stools) and seek care immediately.
Expert Perspective
Dr. Anita Patel, a gastroenterologist, warns:
“Meloxicam’s GI risks are often underestimated. In my practice, I’ve seen NSAID-induced ulcers progress to perforation within weeks in patients ignoring early symptoms like indigestion.”
The Bottom Line
Meloxicam’s safety profile demands respect, not fear. While it avoids the addiction pitfalls of narcotics, its cardiovascular and GI risks require vigilant monitoring. Always weigh its anti-inflammatory benefits against individual risk factors—and never hesitate to ask your provider for safer alternatives.
Expert Insights: When to Use Meloxicam vs. Opioids
Pain management requires a nuanced approach, balancing efficacy, safety, and patient-specific factors. To clarify the roles of Meloxicam (an NSAID) and opioids, we consulted Dr. Laura Simmons, PharmD, and synthesized insights from clinical guidelines. Here’s a comprehensive breakdown of when each medication is most appropriate:
Mechanistic Foundations: Why Meloxicam and Opioids Work Differently
- Meloxicam:
- Mechanism: Inhibits COX-1/COX-2 enzymes, reducing prostaglandin production. This suppresses inflammation, making it ideal for pain rooted in inflammation (e.g., arthritis).
- Key Benefit: Targets the source of pain (e.g., joint swelling) rather than masking it.
- Opioids:
- Mechanism: Bind to mu-opioid receptors in the brain and spinal cord, blocking pain signals and altering perception.
- Key Benefit: Rapid relief for severe, non-inflammatory pain (e.g., trauma, visceral pain).
Approved Uses for Meloxicam: Targeting Chronic Inflammation
Meloxicam is FDA-approved for:
- Osteoarthritis (Adults):
- Manages cartilage degeneration-related pain. Studies show a 30–50% reduction in pain scores with daily use.
- Rheumatoid Arthritis (Adults):
- Reduces joint stiffness and swelling by lowering inflammatory cytokines (e.g., TNF-α, IL-6).
- Juvenile Rheumatoid Arthritis (Children 2+):
- Pediatric formulations (e.g., oral suspension) are weight-adjusted to minimize toxicity risks.
Off-Label Uses:
- Mild to moderate back pain (with confirmed inflammation).
- Acute gout flares (short-term use).
When Opioids Are More Appropriate: Navigating High-Risk Scenarios
Opioids are reserved for cases where NSAIDs are ineffective or contraindicated:
- Severe Acute Pain:
- Examples: Post-surgical recovery, major fractures, burns.
- Rationale: Opioids provide rapid, potent relief when inflammation isn’t the primary driver.
- End-of-Life Care:
- Examples: Advanced cancer, palliative care.
- Rationale: Quality of life outweighs long-term addiction risks here.
- NSAID Contraindications:
- Patient Profiles:
- Renal impairment (eGFR <30 mL/min).
- History of GI bleeding or ulcers.
- Heart failure (NSAIDs exacerbate fluid retention).
- Patient Profiles:
Risk-Benefit Analysis: Meloxicam vs. Opioids
| Factor | Meloxicam | Opioids |
|---|---|---|
| Best For | Chronic inflammatory pain (e.g., arthritis) | Severe acute/non-inflammatory pain (e.g., post-op) |
| Addiction Risk | None | High (25% of long-term users develop dependency) |
| Key Risks | GI bleeding, cardiovascular strain | Respiratory depression, sedation, tolerance |
| Monitoring Needs | Blood pressure, renal function | Respiratory rate, prescription drug monitoring |
Dr. Simmons’ Clinical Pearls
“Meloxicam shines in arthritis care but falls short in trauma or neuropathic pain. For example, a patient with rheumatoid arthritis might thrive on Meloxicam, while someone with metastatic bone pain needs opioids. Always cross-check comorbidities—like hypertension or GERD—before choosing NSAIDs.”
![MELOXICAM1 Meloxicam and Addiction: Why This NSAID Isn’t a Narcotic [Expert Guide]](https://healthysimo.com/wp-content/uploads/2025/05/MELOXICAM1-1024x683.webp)
Emerging Alternatives and Adjuncts
When neither Meloxicam nor opioids fit:
- NSAID Alternatives: Celecoxib (lower GI risk), topical diclofenac.
- Non-Opioid Options:
- Gabapentin: For neuropathic pain.
- Physical Therapy: Enhances mobility in chronic conditions.
- Corticosteroid Injections: Localized inflammation control.
The Bottom Line: A Patient-Centered Approach
- Meloxicam First: For inflammatory pain in patients without cardiovascular/GI risks.
- Opioids as a Last Resort: Short-term use with strict monitoring (per CDC 2022 guidelines).
- Hybrid Strategies: Combine Meloxicam with acetaminophen for synergistic relief, reducing opioid reliance.
Pro Tip: Use tools like the Pain Assessment Toolkit to differentiate inflammatory vs. neuropathic pain and guide drug choice.
FAQs: Addressing Common Concerns
1. Can Meloxicam cause withdrawal symptoms?
No. Stopping Meloxicam abruptly won’t trigger withdrawal, but inflammation or pain may return.
2. Is Meloxicam a controlled substance?
No. It requires a prescription but isn’t regulated like opioids.
3. Why do people confuse NSAIDs with narcotics?
Misuse of the term “narcotic” and outdated beliefs about painkillers contribute to confusion.
Non-Addictive Alternatives to Meloxicam
When Meloxicam isn’t suitable—due to cardiovascular risks, gastrointestinal concerns, or drug interactions—patients and providers can turn to a spectrum of non-addictive alternatives. Below, we explore evidence-based pharmacological, topical, and lifestyle interventions that prioritize safety without compromising efficacy.
1. Alternative NSAIDs: Tailoring to Patient Risk Profiles
NSAIDs remain a cornerstone of anti-inflammatory therapy, but individual risks vary. Consider these options:
| NSAID | Best For | Key Advantages | Risks to Monitor |
|---|---|---|---|
| Naproxen (Aleve) | Intermittent inflammatory pain (e.g., gout) | Longer half-life (8–12 hrs), fewer doses/day | GI bleeding (lower risk than Meloxicam) |
| Celecoxib (Celebrex) | High GI risk patients | COX-2 selective → Reduced stomach irritation | Cardiovascular risks (similar to Meloxicam) |
| Ibuprofen (Advil) | Mild acute pain (e.g., sprains) | OTC availability, rapid onset | Kidney strain with chronic use |
Clinical Note: Celecoxib is preferred for patients with a history of ulcers but avoid in those with heart disease.
2. Topical Therapies: Local Relief, Systemic Safety
Topical treatments bypass the digestive system, minimizing systemic side effects:
- Diclofenac Gel (Voltaren Gel):
- Mechanism: Inhibits COX enzymes locally in joints/muscles.
- Efficacy: Reduces osteoarthritis pain by 40–50% with negligible blood absorption.
- FDA-Approved Uses: Hands, knees, ankles.
- Capsaicin Cream:
- Mechanism: Depletes substance P (a pain neurotransmitter).
- Best For: Neuropathic pain (e.g., diabetic neuropathy).
- Lidocaine Patches:
- Use Case: Post-herpetic neuralgia or localized nerve pain.
3. Lifestyle Modifications: Addressing the Root Cause
Chronic pain often responds to holistic strategies. Key approaches include:
Physical Therapy (PT)
- Mechanism: Strengthens muscles, improves joint stability, and reduces inflammation through movement.
- Conditions Supported:
- Osteoarthritis (land-based or aquatic therapy).
- Chronic lower back pain (core stabilization exercises).
- Evidence: A 2022 JAMA meta-analysis found PT reduces pain scores by 30–60% in knee OA.
Weight Management
- Impact: Every 1 lb of weight loss reduces knee joint load by 4 lbs, slowing cartilage degeneration.
- Strategies:
- Mediterranean diet (anti-inflammatory fats, antioxidants).
- Low-impact exercise (cycling, swimming).
![MELOXICAM risiks1 Meloxicam and Addiction: Why This NSAID Isn’t a Narcotic [Expert Guide]](https://healthysimo.com/wp-content/uploads/2025/05/MELOXICAM-risiks1-1024x683.webp)
Mind-Body Interventions
- Yoga/Tai Chi: Improves flexibility and reduces stress-related pain amplification.
- Cognitive Behavioral Therapy (CBT): Rewires pain perception in chronic cases.
4. Supplements & Nutraceuticals: Nature’s Anti-Inflammatories
While evidence varies, these supplements show promise under medical supervision:
| Supplement | Mechanism | Evidence | Dosage |
|---|---|---|---|
| Turmeric/Curcumin | Inhibits NF-κB (pro-inflammatory pathway) | Moderate OA pain reduction (500–1,000 mg/day) | 500 mg 2x daily |
| Omega-3s (EPA/DHA) | Lowers prostaglandin E2 and leukotrienes | 2.5g/day reduces RA stiffness by 30% | 1,200–2,400 mg/day |
| Boswellia Serrata | Blocks 5-LOX enzyme (lowers leukotrienes) | Effective in knee OA (150–250 mg/day) | 100–250 mg/day |
Critical Caveat:
- Supplements can interact with medications (e.g., omega-3s + blood thinners → bleeding risk).
- Opt for third-party tested brands (USP, NSF certifications).
5. Non-Pharmacologic Medical Interventions
For refractory pain, consider these clinically validated options:
- Acupuncture: Stimulates endogenous opioid release without addiction risk. FDA-approved for chronic lower back pain.
- Transcutaneous Electrical Nerve Stimulation (TENS): Disrupts pain signaling via low-voltage currents.
- Corticosteroid Injections: Local anti-inflammatory effects (e.g., knee OA), limited to 3–4 doses/year.
6. Emerging Alternatives: The Future of Pain Management
- Monoclonal Antibodies (e.g., Tanezumab): Targets nerve growth factor (NGF) for OA pain; avoids NSAID/opioid risks.
- Low-Dose Naltrexone (LDN): Modulates glial cells to reduce neuroinflammation (off-label for fibromyalgia).
Expert Insight: A Pharmacist’s Perspective
Dr. Emily Carter, PharmD, advises:
*“For high-risk patients, I layer therapies—like combining topical diclofenac with PT and omega-3s. This multimodal approach minimizes reliance on systemic NSAIDs while addressing pain holistically.”*
The Bottom Line
Meloxicam alternatives exist on a spectrum from NSAIDs to lifestyle changes, each with unique benefits and limitations. The key is personalization:
- Prioritize topicals for localized pain.
- Pair supplements with PT for synergistic effects.
- Reserve advanced interventions (e.g., biologics) for refractory cases.
Always consult a healthcare provider to tailor strategies to your medical history and pain type.
Conclusion
Meloxicam occupies a critical niche in pain management as a potent NSAID that sidesteps the addiction pitfalls of narcotics. Its ability to target inflammation at its source makes it indispensable for conditions like osteoarthritis and rheumatoid arthritis, offering millions a reprieve from chronic pain without the specter of dependency. Yet, this therapeutic power comes with sobering caveats.
The drug’s boxed warnings—cardiovascular thrombosis and gastrointestinal bleeding—are not mere footnotes but urgent reminders that no medication is universally safe. For some patients, particularly those with hypertension, a history of ulcers, or renal impairment, Meloxicam’s risks may eclipse its benefits. This underscores a cardinal rule in pharmacology: the right drug for the right patient at the right dose.
Key Takeaways for Patients and Providers
- Non-Addictive ≠ Risk-Free: While Meloxicam lacks opioid-like addiction potential, its systemic effects demand vigilance. Regular monitoring of blood pressure, kidney function, and GI health is non-negotiable for long-term users.
- Alternatives Abound: From topical NSAIDs like diclofenac gel to mind-body therapies (e.g., yoga, acupuncture), a spectrum of options exists for those incompatible with Meloxicam.
- Personalization is Paramount: A 55-year-old with controlled hypertension might thrive on Meloxicam, while a 70-year-old with prior GI bleeding should avoid it entirely.
A Call to Action: Collaborate, Don’t Guess
Pain management is not a solo endeavor. Before starting or stopping Meloxicam:
- Ask your provider: “Do my benefits outweigh my risks?”
- Consult a pharmacist: Review drug interactions (e.g., SSRIs, blood thinners).
- Explore multidisciplinary care: Rheumatologists, physical therapists, and dietitians can build a safety net around your treatment plan.
In an era shadowed by the opioid crisis, Meloxicam represents progress—but progress with boundaries. By pairing its anti-inflammatory prowess with informed, individualized care, patients can navigate pain relief without trading one set of dangers for another.
Sources:
- FDA Meloxicam Label. (2023).
- CDC Guideline for Prescribing Opioids. (2022).
- Pain Medicine Study on NSAID Abuse Potential. (2021).

