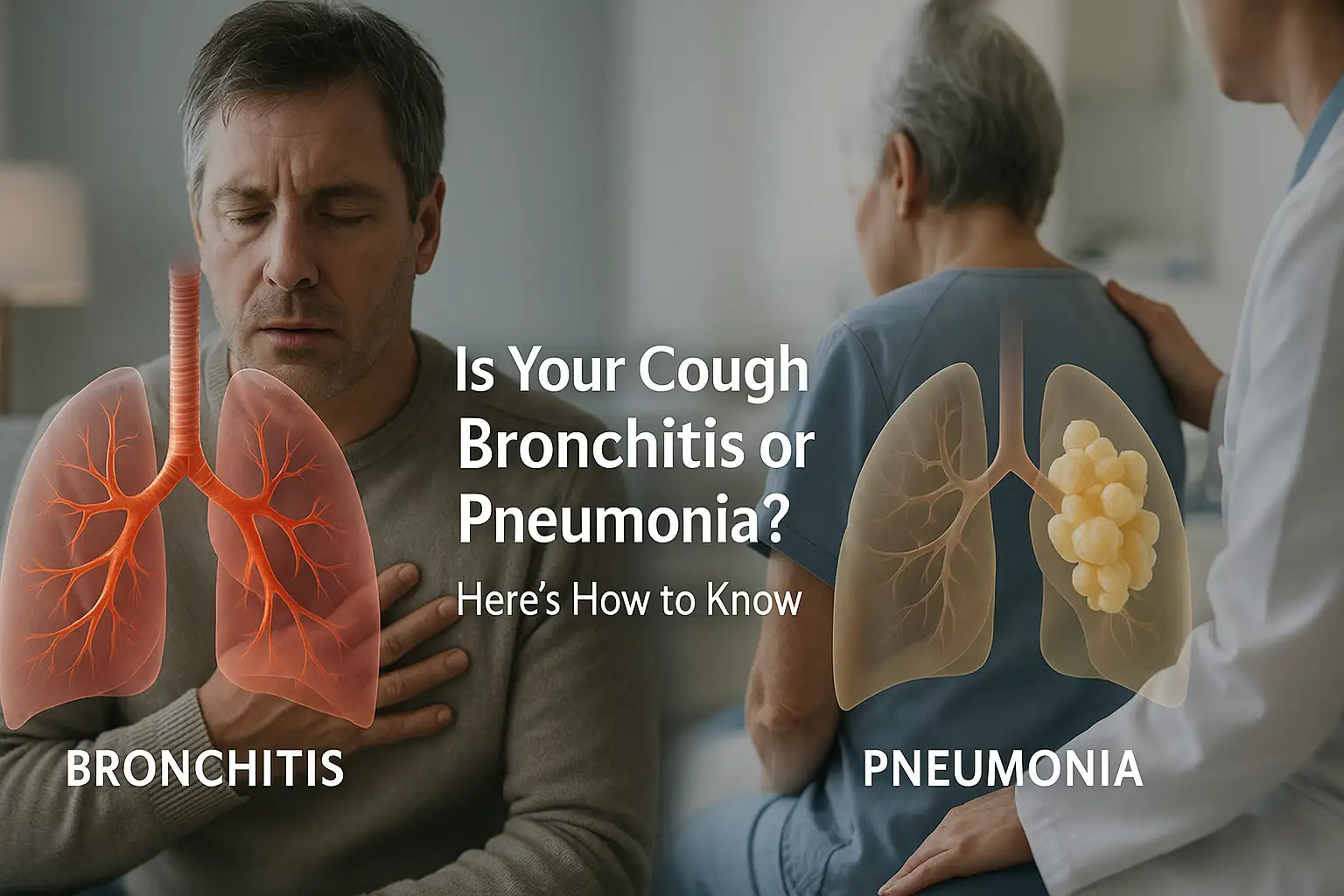
That persistent cough, the chest congestion, the general feeling of being unwell—you know you’re sick, but is it Bronchitis or Pneumonia? When a respiratory infection takes hold, figuring out which one you have is crucial, as one is often a passing illness while the other can be far more serious. While both conditions share similar symptoms like coughing and fatigue, understanding the key differences between Bronchitis or Pneumonia is the first step toward getting the right treatment and ensuring a smooth recovery.
Misjudging your symptoms can carry risks: ignoring the signs of pneumonia can lead to severe complications, while stressing over a common case of acute bronchitis is unnecessary. This guide will cut through the confusion, breaking down the symptoms, causes, and treatments for both, empowering you to understand what your body is telling you and know precisely when it’s time to seek professional medical care.
The Core Difference: Location Matters
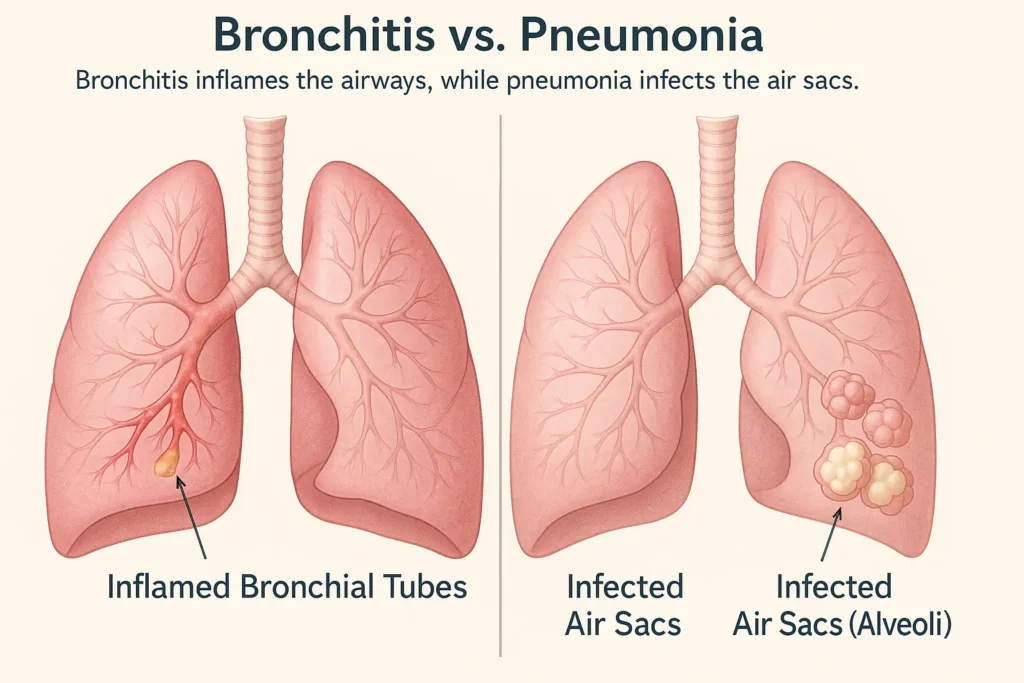
While both illnesses can start with a cough, they are fundamentally different infections that target distinct areas of your respiratory system. Understanding this geographical distinction within your lungs is the key to understanding why their symptoms and severity differ so dramatically.
What is Bronchitis? The “Highway” Inflammation
Acute bronchitis is the sudden inflammation and swelling of the bronchial tubes. To visualize this, imagine your respiratory system as an upside-down tree. The windpipe (trachea) is the trunk, which splits into two main branches (the bronchi), one for each lung. These branches then divide again and again into smaller and smaller airways (bronchioles), much like twigs on a tree.
Bronchitis is an infection of the inner lining of these “tree branches.” As the immune system fights the invader—most often a virus like the cold or flu—the bronchial tubes become inflamed and produce excess mucus. This is the source of the classic bronchitis symptom: a persistent, often productive cough.
“Think of bronchitis as a major traffic jam on the airways, the highways of your lungs,” explains Dr. Emily Thorne, a pulmonologist. “The roads themselves are swollen and clogged with debris (mucus), causing congestion and the frustrating hack. However, the destinations—the tiny air sacs where oxygen exchange happens—remain largely unaffected.” Because the infection is confined to the airways and is usually viral, antibiotics, which target bacteria, are ineffective.
What is Pneumonia? The “Air Sac” Invasion
Pneumonia, in contrast, is an infection that bypasses the major highways and settles deep within the alveoli, the microscopic air sacs at the very ends of the bronchial “twigs.” This is where the critical work of breathing occurs: oxygen from the inhaled air passes into your bloodstream, and carbon dioxide, a waste product, is removed.
When pathogens like bacteria (the most common cause in adults) or viruses reach the alveoli, the body’s immune response causes these delicate sacs to fill with fluid, pus, and inflammatory cells. This infiltration effectively drowns the functional lung tissue, preventing oxygen transfer.
“Pneumonia is like the infection has set up camp deep in the neighborhoods of your lungs,” says Dr. Thorne. “This invasion and flooding of the lung tissue itself is what leads to the more severe, systemic symptoms like high fever, chills, and significant shortness of breath. The lungs struggle to do their primary job, which is why pneumonia can be so much more serious than bronchitis.” The severity directly correlates with how many of these “neighborhoods” are affected.
Symptom Checker: Bronchitis vs. Pneumonia
ThiThis table provides a clear, at-a-glance comparison. Use it as a guide, but remember that individual experiences can vary, especially in young children, older adults, or those with weakened immune systems.
| Symptom | Bronchitis | Pneumonia |
|---|---|---|
| Cough | Prominent and persistent. This is the hallmark symptom, caused directly by the inflammation and irritation of the bronchial tubes. The cough often produces mucus that is clear, white, or yellowish. It’s common for the cough to linger for several weeks after other symptoms have improved, as the airways take time to heal. | Present and often more productive. The cough is a result of the lungs trying to clear fluid and pus from the infected air sacs. The phlegm can be thick and may be green, yellow, or even have a rust-colored tinge, which is a sign of old blood and is a classic indicator of bacterial pneumonia. |
| Fever | Low-grade (under 100.4°F / 38°C) or absent. Since bronchitis is often a localized airway infection, it typically doesn’t trigger a significant systemic (whole-body) immune response like a high fever. | Common and can be high. A fever of 102°F (39°C) or higher is a strong indicator of pneumonia. This high fever reflects the body’s intense, systemic battle against an infection that has invaded the deep lung tissue. |
| Shortness of Breath | Usually mild, if present. Breathlessness is generally due to the narrowing of inflamed airways and chest congestion. Wheezing is a common accompanying sound. | More common and pronounced. This occurs because the fluid-filled air sacs cannot effectively transfer oxygen to the blood. This impaired gas exchange can lead to significant shortness of breath, even during rest or mild activity. |
| Chest Pain | Aching discomfort or soreness. This pain is typically muscular, resulting from the strain and fatigue of the relentless coughing spells. | Sharp or stabbing “pleuritic” pain. This pain is localized and worsens with deep breaths or coughing. It is caused by inflammation of the pleura (the lining around the lungs), which happens when the infection is adjacent to this sensitive tissue. |
| Onset | Often gradual, following a cold or flu. Symptoms typically evolve from an upper respiratory infection (runny nose, sore throat) that “moves down” into the chest over a few days. | Can be sudden or gradual. It may appear suddenly as a severe illness (especially bacterial pneumonia) or develop slowly as a worsening complication of an existing cold or bronchitis. |
| General Feeling | Feeling “rundown” and tired. You feel unwell, but it’s often manageable. The fatigue is largely from the body fighting the virus and the physical exertion of coughing. | A sudden, severe feeling of being very ill. Patients often report feeling “like they’ve been hit by a truck.” This is accompanied by shaking chills, drenching sweats, and profound fatigue due to the systemic infection. |
| Other Symptoms | Upper respiratory symptoms are common. These include a runny or stuffy nose, sore throat, and headache, reflecting the viral origin. Wheezing is a key sign of airway constriction. | Gastrointestinal symptoms can occur. Nausea, vomiting, and diarrhea are more frequent, especially in children with viral pneumonia. Confusion or delirium can be a presenting symptom in the elderly. |
Key Takeaway: While a nagging cough is central to both, the presence of a high fever (102°F+), shaking chills, significant shortness of breath, and sharp, localized chest pain are your body’s red flags, strongly indicating a deeper lung infection (pneumonia) rather than a bronchial tube issue (bronchitis). If you experience this cluster of more severe symptoms, it is essential to consult a healthcare provider promptly.
Why the Cause Dictates the Treatment
The fundamental difference in what causes these infections is the single most important factor determining how they are treated. Using the wrong approach is not only ineffective but can also be harmful. Understanding this “why” empowers you to have more informed discussions with your healthcare provider.
Bronchitis Treatment: Supporting Your Body’s Natural Defenses
Since over 90% of acute bronchitis cases are viral, the treatment strategy is not to fight the infection directly with medication, but to create the best possible environment for your own immune system to win the battle.
Why Viral Infections Can’t Be Treated with Antibiotics: Antibiotics are designed to target and disrupt specific life processes in bacteria. Viruses are completely different organisms; they hijack our own cells to replicate. An antibiotic has no mechanism to attack a virus, making it utterly useless against viral bronchitis. The CDC and other health bodies strongly advise against using antibiotics for viral bronchitis to prevent antibiotic resistance.
Effective Supportive Care Strategies:
- Plenty of Rest and Fluids: This is not just cliché advice; it’s essential. Rest conserves your body’s energy for the immune response. Fluids help thin the thick mucus in your inflamed bronchial tubes, making it easier to cough up and clear your airways.
- Using a Humidifier: Moist air is soothing. It helps reduce the irritation and dryness in your airways, which can calm a nagging, tickling cough and make breathing feel easier.
- Over-the-Counter Pain Relievers: Medications like ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) do not fight the virus, but they effectively manage the uncomfortable symptoms of the illness, such as low-grade fever, body aches, and headache.
- Honey in Warm Tea: Studies have shown that honey can be as effective as some over-the-counter cough suppressants. It coats and soothes the irritated throat lining, providing direct relief from the rawness caused by coughing.
- Avoiding Cough Suppressants (Sometimes): While a relentless cough is exhausting, it serves a vital purpose: it’s your body’s mechanism for clearing mucus from your lungs. Suppressing it completely can trap the infection. However, if the cough is preventing sleep, your doctor may recommend a suppressant for nighttime use.
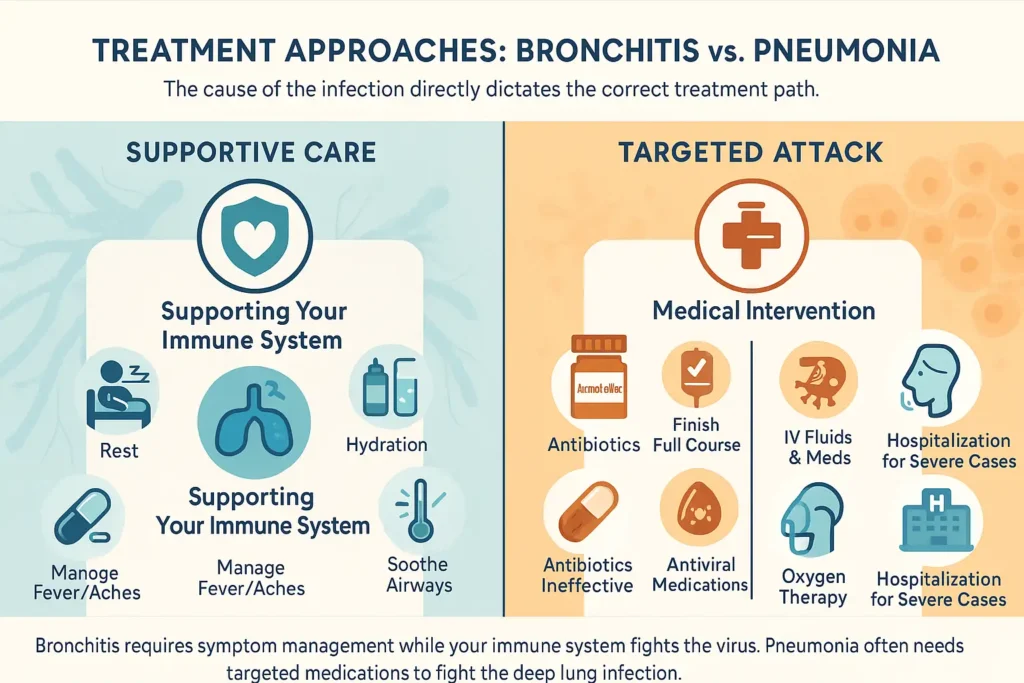
Pneumonia Treatment: A Targeted Medical Attack
Pneumonia requires a more aggressive, targeted approach because the infection is deeper and can cause significant damage to lung tissue. The treatment plan is entirely dependent on the identified or suspected cause.
1. Bacterial Pneumonia: The Role of Antibiotics
- This is the most common type of pneumonia in adults. When a healthcare provider diagnoses bacterial pneumonia, they will prescribe a specific antibiotic to target the underlying bacteria.
- Crucial Note: Finishing the entire course of antibiotics is non-negotiable, even if you start feeling better after a few days. Stopping early can allow the hardiest bacteria to survive and multiply, leading to a relapse and contributing to the global crisis of antibiotic-resistant bacteria.
2. Viral Pneumonia: Antiviral Support
- While less common, viruses like influenza (flu), RSV, and SARS-CoV-2 (COVID-19) can cause pneumonia.
- Treatment: Antibiotics are ineffective. For certain viruses like influenza, antiviral medications (e.g., oseltamivir/Tamiflu) can be prescribed. These drugs work best when started early in the illness and can help reduce the severity and duration. For many other viruses, treatment remains supportive (rest, fluids, fever control), similar to bronchitis but with closer monitoring.
3. Severe Cases: Hospitalization for Intensive Care
Pneumonia can become life-threatening, especially for the very young, elderly, or those with compromised immune systems. Hospitalization is necessary when the body needs more support than can be provided at home. This may include:
- Intravenous (IV) Fluids and Antibiotics: To deliver medication and hydration directly into the bloodstream for faster and more effective action.
- Oxygen Therapy: To ensure the blood gets enough oxygen when the lungs are too compromised to do so on their own. In the most critical cases, a patient may require a ventilator (breathing machine).
Conclusion: The treatment path diverges sharply at diagnosis. Bronchitis calls for patience and supportive self-care, while pneumonia demands a precise, medically-supervised attack on the specific pathogen. This is why getting an accurate diagnosis from a healthcare provider is so critical.
When to Stop Guessing and See a Doctor
It’sWhile many cases of acute bronchitis resolve on their own, it is always best to err on the side of caution. Self-diagnosing can be risky, as pneumonia requires a professional diagnosis and specific treatment. You should consult a healthcare provider if you experience any of the following red-flag symptoms, which indicate your body is fighting a significant battle that may need medical intervention.
Seek Prompt Medical Care if You Experience:
- A cough that lasts more than three weeks. A persistent cough suggests that your airways are taking too long to heal or that the initial diagnosis may have been incorrect. It could signal a lingering infection, developing asthma, or another underlying condition that needs evaluation.
- A fever of 102°F (39°C) or higher that persists for more than a day or two. A high, persistent fever is a classic sign that your body is fighting a serious infection, most commonly associated with bacterial pneumonia. This is not a typical feature of simple bronchitis and warrants investigation.
- Shortness of breath, wheezing, or a feeling that you can’t catch your breath. While mild breathlessness can occur with bronchitis, significant shortness of breath—especially when you are at rest—suggests your lungs are struggling to oxygenate your blood. This is a key symptom of pneumonia, where the air sacs are compromised.
- Chest pain that is sharp, stabbing, or localized, and worsens when you breathe deeply or cough. This type of pain, known as pleuritic pain, indicates inflammation of the pleura (the lining around the lungs). This is a common complication of pneumonia and is not typical of the general chest soreness caused by bronchitis coughing fits.
- Coughing up blood (hemoptysis) or rust-colored mucus. Blood-tinged sputum is a serious sign. Rust-colored mucus is a classic indicator of pneumococcal (bacterial) pneumonia. Coughing up any amount of bright red blood requires immediate medical attention to determine the source of the bleeding.
- Symptoms that improve initially but then return, worse than before. This “double-sickening” pattern can be a sign of a secondary bacterial infection. For example, you might start with a viral bronchitis, only to have bacteria invade the weakened airways or lungs, leading to a more severe case of bacterial pneumonia.
What to Expect at the Doctor’s Visit
When you see a healthcare provider with these symptoms, they will work to determine the root cause:
Chest X-Ray: This is the definitive test to diagnose pneumonia. An X-ray can clearly show the cloudy areas of consolidation (fluid and pus) in the air sacs that are not present in bronchitis.
Physical Exam: The doctor will listen to your lungs with a stethoscope. Crackling, bubbling, or rumbling sounds can indicate fluid in the alveoli (pneumonia), while wheezing is more characteristic of narrowed airways (bronchitis).
Pulse Oximetry: A small device clipped to your finger painlessly measures the oxygen level in your blood. A low reading is a strong indicator of pneumonia.
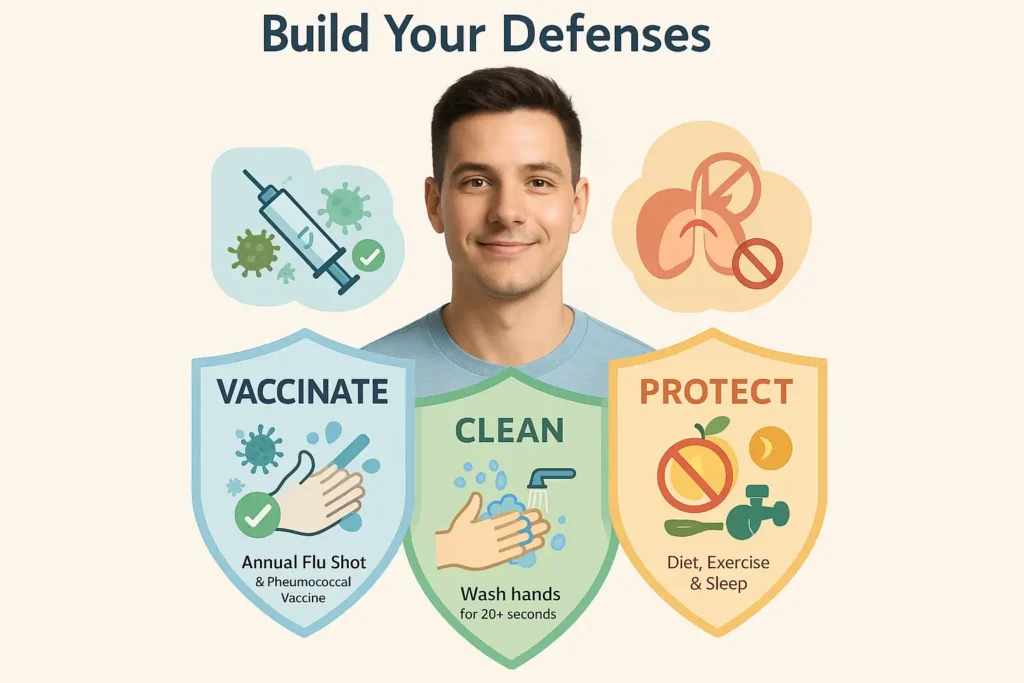
Prevention is the Best Medicine
While you can’t eliminate all risk, proactively strengthening your body’s defenses is the most powerful way to reduce your chances of developing bronchitis or pneumonia. Think of it as building a multi-layered shield for your respiratory system. Here’s how you can fortify your defenses.
1. Prioritize Vaccination: Your First Line of Defense
Vaccines are the most effective tool for preventing specific infections that can lead to these illnesses.
- The Annual Flu Shot: Influenza is a major cause of both viral bronchitis and viral pneumonia. Getting vaccinated every year significantly reduces your risk of catching the flu, thereby preventing a potential cascade into a more serious lower respiratory infection.
- Pneumococcal Vaccines: These vaccines specifically protect against Streptococcus pneumoniae, the most common cause of bacterial pneumonia. The CDC recommends them for:
- All children under 2 years old.
- Adults 65 years and older.
- Anyone over 2 with chronic health conditions (e.g., heart disease, diabetes, COPD) or a weakened immune system.
- Other Relevant Vaccines: Stay up-to-date on other vaccines like COVID-19 and RSV (recommended for older adults and infants), as these viruses can also lead to pneumonia.
2. Master Hand Hygiene: Break the Chain of Infection
Your hands are the primary transporters of germs to your eyes, nose, and mouth.
- Technique is Key: Wash your hands thoroughly with soap and clean water for at least 20 seconds (about the time it takes to sing “Happy Birthday” twice). Scrub the backs of your hands, between your fingers, and under your nails.
- When to Wash: Make it a habit before eating, after using the restroom, and after being in public spaces.
- Use Hand Sanitizer: When soap and water aren’t available, use an alcohol-based hand sanitizer with at least 60% alcohol as an effective alternative.
3. Avoid Lung Irritants: Protect Your Natural Defenses
Your respiratory tract has tiny hair-like structures called cilia that sweep mucus and debris out of your airways. Irritants paralyze and damage these crucial defenders.
- Quit Smoking: Smoking is one of the most significant risk factors for severe respiratory infections. It damages the cilia and lung tissue, making it easier for pathogens to take hold and harder for your body to clear them out.
- Avoid Secondhand Smoke: Even occasional exposure can irritate and inflame the airways, weakening their local immunity.
- Limit Exposure to Pollution and Chemicals: On high-pollution days, limit your time outdoors. If you work with chemical fumes or dust, always use appropriate protective equipment like a respirator mask.
4. Maintain a Healthy Lifestyle: Fortify Your Immune System
A well-functioning immune system is your best internal army. Support it with these foundational habits:
- Balanced Diet: Fuel your body with a variety of fruits, vegetables, lean proteins, and whole grains. These foods provide essential vitamins (like C and D) and zinc that are critical for immune cell function.
- Regular Exercise: Moderate, consistent exercise has been shown to improve immune surveillance, helping your body detect and fight off pathogens more effectively. Aim for at least 150 minutes of moderate activity per week.
- Adequate Sleep: During sleep, your body produces and distributes key immune cells like cytokines. Consistently getting 7-9 hours of quality sleep is non-negotiable for a robust immune response.
- Manage Stress: Chronic stress elevates cortisol levels, which can suppress the immune system. Incorporate stress-reduction techniques such as meditation, deep breathing, or yoga into your routine.
Conclusion:
Listening to your body is key. While a nagging cough is often just bronchitis, the presence of severe, systemic symptoms like high fever, chills, and significant breathing problems is your body’s signal that something more serious, like pneumonia, could be at play. Use this knowledge not to self-diagnose, but to have an informed conversation with your healthcare provider to get the care you need and get back on the path to health.
Ressources
- Centers for Disease Control and Prevention (CDC) – Pneumonia
- www.cdc.gov/pneumonia
- For: Comprehensive overview, prevention tips, and vaccination guidelines.
- American Lung Association – Bronchitis
- www.lung.org/bronchitis
- For: Detailed patient-focused information on symptoms, causes, and management of bronchitis.
- Mayo Clinic – Pneumonia
- www.mayoclinic.org/pneumonia
- For: In-depth, easy-to-understand explanations of symptoms, causes, and treatment options.
- National Heart, Lung, and Blood Institute (NHLBI) – Bronchitis
- www.nhlbi.nih.gov/bronchitis
- For: Science-based details on the diagnosis and treatment of bronchitis.