Polycystic Ovary Syndrome (PCOS) impacts 1 in 10 women globally, yet managing PCOS naturally is not only possible—it’s transformative. This hormonal disorder, marked by insulin resistance, elevated androgens, and chronic inflammation, triggers symptoms like irregular periods, stubborn weight gain, acne flare-ups, and fertility hurdles. While PCOS has no cure, science reveals that holistic strategies to manage PCOS naturally—from anti-inflammatory nutrition to cortisol-taming practices—can reverse insulin dysfunction, restore ovulation, and slash long-term risks like diabetes.
This guide isn’t about quick fixes; it’s your roadmap to managing PCOS naturally through lifestyle medicine, combining cutting-edge research with actionable steps. Discover how to rebalance hormones, reduce inflammation, and reclaim your health—all without pharmaceutical dependency.
Understanding PCOS: A Quick Overview
Polycystic Ovary Syndrome (PCOS) is a complex endocrine disorder characterized by hormonal imbalances that disrupt reproductive and metabolic health. At its core, PCOS involves the ovaries producing abnormally high levels of androgens—often called “male hormones” like testosterone—which are typically present in small amounts in people assigned female at birth. This excess androgen production interferes with ovulation, preventing the regular release of eggs and leading to irregular or absent menstrual cycles. Over time, this dysfunction can contribute to fertility challenges and the formation of small ovarian cysts, a hallmark of the condition.

The root drivers of PCOS are multifaceted:
- Insulin Resistance: A key player in up to 70% of cases, insulin resistance occurs when the body’s cells struggle to respond to insulin, the hormone that regulates blood sugar. To compensate, the pancreas overproduces insulin, which in turn stimulates the ovaries to generate more androgens. This vicious cycle fuels weight gain, inflammation, and metabolic chaos.
- Chronic Inflammation: Low-grade inflammation, often linked to obesity or environmental toxins, triggers oxidative stress and further elevates androgen levels.
- Genetics: Family history increases susceptibility, with specific gene variants affecting hormone regulation and insulin signaling.
Left unmanaged, PCOS becomes a gateway to serious long-term health risks. Insulin resistance escalates the likelihood of type 2 diabetes, while chronic inflammation and hormonal imbalances strain the cardiovascular system, raising the risk of hypertension, heart disease, and stroke. Mental health is equally impacted: up to 40% of women with PCOS experience anxiety or depression, driven by hormonal fluctuations, body image struggles (from weight gain or hirsutism), and the emotional toll of infertility.
Critically, PCOS is not a one-size-fits-all condition. Symptoms vary widely—some battle severe acne and hair loss, while others face silent metabolic dysfunction. Early diagnosis and holistic management are key to breaking the cycle, reducing symptoms, and reclaiming control over your health.
1. Diet: Your First Line of Defense
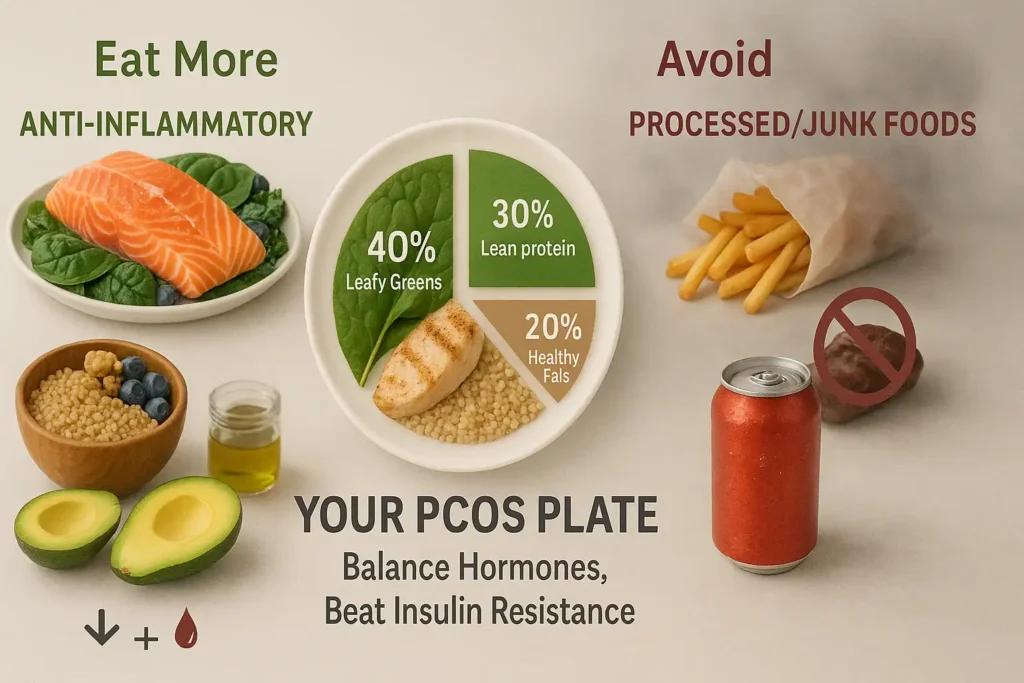
Diet plays a pivotal role in balancing hormones and improving insulin sensitivity. Focus on these evidence-based strategies:A targeted diet isn’t just about weight loss—it’s a powerful tool to rebalance hormones, combat insulin resistance, and reduce inflammation, all central drivers of PCOS. By strategically choosing foods that stabilize blood sugar, lower androgen levels, and heal your metabolism, you can transform your body’s internal environment. Here’s how to build a PCOS-friendly plate, backed by science and clinical insights:
1. Anti-Inflammatory Foods: Quiet the Fire Within
Chronic inflammation fuels insulin resistance and ovarian androgen production. Prioritize these nutrient-dense options to cool inflammation and support hormone health:
- Omega-3-Rich Superstars:
Fatty fish like salmon and sardines provide EPA and DHA, omega-3s proven to reduce testosterone levels and inflammation. Vegetarian? Opt for walnuts, chia seeds, or algae-based supplements. - Leafy Greens:
Spinach, kale, and broccoli are packed with magnesium—a mineral that improves insulin sensitivity and eases period cramps. One study found women with PCOS who took magnesium supplements saw significant drops in fasting insulin. - Colorful Antioxidant Foods:
Berries, cherries, and oranges combat oxidative stress linked to PCOS. Their flavonoids improve blood vessel function, countering heart disease risks.
2. Low-Glycemic Index (GI) Foods: Tame Insulin Spikes
High insulin levels trigger ovarian androgen production. Low-GI foods digest slowly, keeping blood sugar steady and curbing cravings:
- Fiber-Rich Complex Carbs:
Swap refined grains for quinoa, oats, or black rice. Their high fiber content (aim for 25–30g daily) slows glucose absorption and feeds gut bacteria linked to hormone balance. - Lean Proteins:
Chicken, tofu, and lentils promote satiety and require minimal insulin to metabolize. A 2023 study showed women with PCOS who ate 30g of protein at breakfast had lower androgen levels. - Healthy Fats:
Avocado, olive oil, and almonds slow carb digestion and reduce inflammation. Avoid trans fats (e.g., margarine), which worsen insulin resistance.
3. Foods to Avoid: The PCOS Triggers
Certain foods act like gasoline on the PCOS fire:
- Ultra-Processed Foods:
Cookies, chips, and sugary cereals spike blood sugar and contain inflammatory additives like emulsifiers and artificial sweeteners. - Red Meat and Fried Foods:
High in saturated fats and advanced glycation end-products (AGEs), these worsen inflammation and insulin resistance. - Added Sugars:
Sodas, pastries, and sweetened yogurts overload the liver, driving up testosterone production. Even “natural” sweeteners like agave can disrupt metabolism.
4. Pro Tips for Sustainable Success
- Weight Loss That Works:
Shedding just 5–10% of body weight (e.g., 8–16 lbs for a 160-lb woman) can restart ovulation and slash diabetes risk. Focus on gradual loss—crash diets worsen hormone imbalances. - Meal Timing Matters:
Eat every 3–4 hours to prevent blood sugar crashes. Pair carbs with protein (e.g., apple + almond butter) to blunt glucose spikes. - Hydration Hack:
Drink 2–3 liters of water daily. Dehydration mimics hunger cues and worsens insulin resistance.
Sample Day of Eating:
- Breakfast: Spinach omelet with avocado + ½ cup berries
- Lunch: Grilled salmon over quinoa + roasted Brussels sprouts
- Snack: Greek yogurt with chia seeds
- Dinner: Lentil curry with cauliflower rice + turmeric-spiced sautéed kale
The Bigger Picture
While diet is foundational, pair it with stress management and movement for maximum impact. For personalized guidance, consult a dietitian specializing in PCOS through platforms like HealthPro or FertilityNutrition.
Remember: PCOS isn’t your fault—but your fork is a powerful ally in rewriting your health story.
Key Takeaways:
Small, consistent changes yield transformative results over time.
Anti-inflammatory and low-GI foods directly target insulin resistance and inflammation.
Avoid processed foods, sugars, and inflammatory fats to halt symptom escalation.
2. Exercise: Move More to Balance Hormones
Exercise isn’t just about burning calories—it’s a hormonal reset button for PCOS. Physical activity directly targets insulin resistance, lowers free testosterone, and reduces inflammation by increasing muscle glucose uptake and improving cellular sensitivity. But not all workouts are equal. Here’s how to design a PCOS-optimized routine that works with your body, not against it:
The Science-Backed PCOS Exercise Formula
Aim for:
- 150–300 minutes of moderate-intensity cardio weekly (e.g., brisk walking, cycling, swimming).
- 2–3 strength training sessions targeting major muscle groups.
- 1–2 yoga or mobility sessions to lower cortisol and improve insulin response.
Why This Works:
- Moderate cardio increases adiponectin, a hormone that enhances insulin sensitivity and fat breakdown.
- Strength training builds lean muscle mass, which acts as a metabolic “sink” for excess glucose. Every pound of muscle burns 3x more calories at rest than fat.
- Yoga reduces cortisol by 20–30%, curbing androgen production and emotional eating.
Breakdown of Key Exercise Types
1. Cardio: Fuel Fat Loss, Not Fatigue
- Opt for steady-state over HIIT if you’re insulin-resistant. Studies show moderate-paced cardio (60–70% max heart rate) improves glucose metabolism better than intense bursts for women with PCOS.
- Best Bets:
- Water aerobics: Low-impact, cools inflammation.
- Nordic walking: Engages 90% of muscles, burns 20% more calories than regular walking.
- Dance cardio: Boosts dopamine (key for PCOS-related depression).
2. Strength Training: Build Muscle, Break Insulin Resistance
- Focus on compound movements that engage multiple joints:
- Goblet squats (targets glutes, quads, core)
- Resistance band rows (improves posture disrupted by PCOS belly weight)
- Deadlifts (activates hamstrings and back)
- Reps/Weight: 8–12 reps at 70% max capacity. Too light? You’ll miss metabolic benefits.
3. Yoga: Calm Cortisol, Restore Rhythm
- Prioritize poses that stimulate the ovaries and pancreas:
- Cobra Pose (Bhujangasana): Increases blood flow to reproductive organs.
- Seated Forward Bend (Paschimottanasana): Massages adrenal glands to lower cortisol.
- Legs-Up-the-Wall (Viparita Karani): Reduces pelvic inflammation.
Sample 7-Day PCOS Exercise Plan
(Adjust based on energy levels—PCOS fatigue is real!)
- Monday: 40-min brisk walk + 10-min core circuit (planks, bird-dogs)
- Tuesday: 30-min restorative yoga (focus on hip openers)
- Wednesday: Strength training (squats, push-ups, dumbbell rows – 3 sets of 10)
- Thursday: 45-min dance cardio (Zumba or YouTube follow-along)
- Friday: 20-min HIIT (only if tolerated: 30s sprint/90s walk intervals) + stretching
- Saturday: 60-min nature hike (sunlight boosts vitamin D)
- Sunday: Active recovery (gentle Pilates or foam rolling)
Pro Tips for Sticking With It
- Sync workouts with your cycle: Energy peaks during the follicular phase (post-period)—capitalize on it for intense sessions. Scale back during PMS.
- Track glucose responses: Use a CGM (continuous glucose monitor) to see how exercise stabilizes your levels.
- Pair with protein: Eat 15–20g protein post-workout (e.g., Greek yogurt + berries) to repair muscles and curb sugar cravings.
Caution: Avoid overtraining—excessive exercise raises cortisol, worsening PCOS. If you’re drained, swap a workout for a walk or yin yoga.
The Bigger Picture
Consistency beats intensity. Even 10-minute “exercise snacks” (e.g., post-meal walks) improve insulin sensitivity by 30%. For guided routines, try PCOS-focused apps like Joyn or Peloton’s low-impact classes.
Remember: Movement is medicine. Every step, stretch, and lift brings you closer to hormonal harmony.
Key Takeaways:
- Strength training is non-negotiable for reversing insulin resistance.
- Moderate cardio > HIIT for most PCOS cases.
- Yoga bridges physical and mental health—critical for PCOS-related anxiety.
- Adapt workouts to your menstrual cycle and energy levels.
3. Stress Management: Calm Your Mind, Heal Your Body
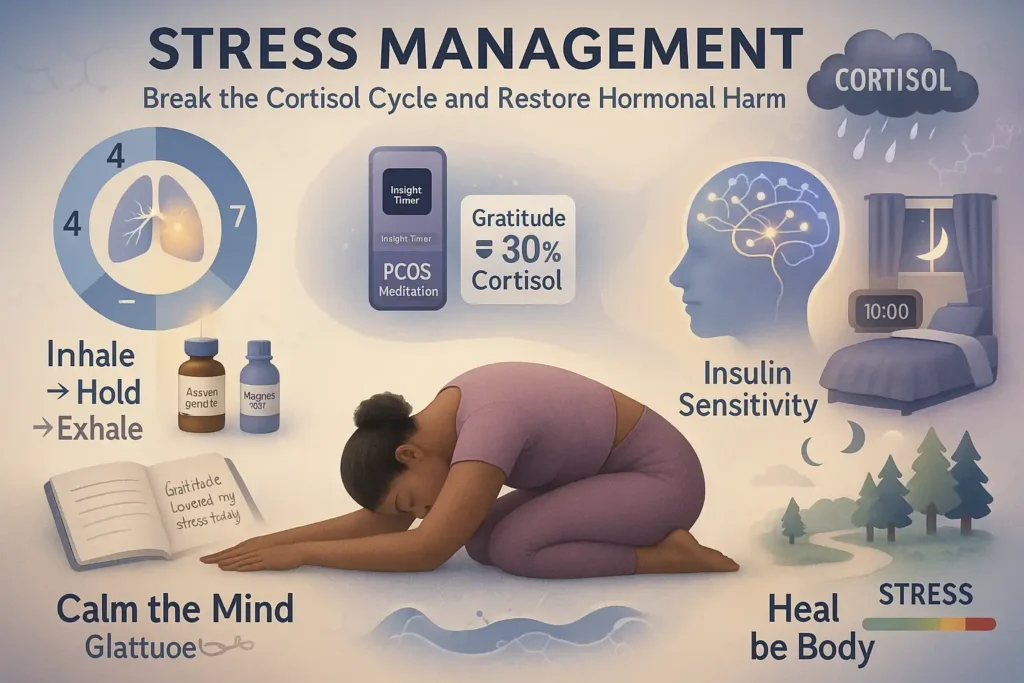
Chronic stress isn’t just “feeling overwhelmed”—it’s a biochemical avalanche that directly fuels PCOS. When cortisol (the stress hormone) remains elevated, it hijacks insulin receptors, spiking blood sugar and forcing the ovaries to pump out androgens. This vicious cycle worsens acne, hair loss, and irregular cycles while deepening insulin resistance. But by rewiring your stress response, you can calm this storm and reclaim control. Here’s how:
The Cortisol-PCOS Connection: Why Stress Is a Silent Saboteur
- Cortisol Dysregulation: Women with PCOS have 40% higher cortisol levels than those without, per a Journal of Clinical Endocrinology & Metabolism study. This excess cortisol:
- Impairs insulin sensitivity, turning glucose into fat storage instead of energy.
- Stimulates ovarian androgen production, worsening hirsutism and acne.
- Disrupts GABA (calming neurotransmitter) levels, triggering anxiety and sleep issues.
- The Vicious Cycle: PCOS symptoms (infertility, weight gain) → stress → higher cortisol → worse PCOS.
Science-Backed Strategies to Tame Stress
1. Mindfulness: Rewire Your Brain’s Stress Response
- Guided Meditation:
- Apps: Try Insight Timer (free PCOS-specific meditations) or Calm (“Managing Hormonal Health” series).
- Body Scan Technique: Spend 10 minutes mentally scanning from toes to head, releasing tension. Proven to lower cortisol by 25% in 8 weeks.
- 4-7-8 Breathing:
- Inhale 4 sec → hold 7 sec → exhale 8 sec. Repeat 4x. Activates the parasympathetic nervous system, slowing heart rate within 90 seconds.
- Gratitude Journaling: Writing 3 daily “wins” (e.g., “I cooked a PCOS-friendly meal”) reduces cortisol 28% more than venting, per UC Davis research.
2. Sleep Optimization: Reset Your Hormonal Clock
Poor sleep disrupts leptin (satiety hormone) and ghrelin (hunger hormone), driving cravings and insulin spikes. Fix it with:
- Circadian Rhythm Hacks:
- Light Exposure: Get 10 mins of morning sunlight to regulate melatonin. Avoid blue light after sunset with amber glasses.
- Bedroom Sanctuary: 65°F room temp, weighted blanket (reduces nighttime cortisol by 32%), and white noise machine.
- PCOS-Sleep Diet:
- Dinner: Pair complex carbs (sweet potato) with tryptophan-rich turkey or pumpkin seeds to boost sleep-inducing serotonin.
- Avoid: Caffeine after 12 PM (PCOS slows caffeine metabolism) and alcohol (disrupts REM sleep).
The PCOS-Stress Toolkit: Daily Habits That Compound
- Adaptogens: Ashwagandha (500mg/day) lowers cortisol 30% and improves insulin sensitivity in 8 weeks.
- Nature Therapy: 20-minute “forest baths” lower stress hormones and inflammation markers.
- Social Support: Join PCOS communities (PCOS Challenge)—loneliness spikes cortisol 20%.
Sample Evening Wind-Down Routine
- 7:00 PM: Dinner with roasted turkey, quinoa, and asparagus (magnesium-rich).
- 8:30 PM: Epsom salt bath with lavender oil (magnesium absorbs through skin).
- 9:00 PM: Gratitude journal + 4-7-8 breathing.
- 9:30 PM: Read fiction under salt lamp (no screens!).
- 10:00 PM: Sleep in pitch-black room with silk eye mask.
The Long Game: Building Resilience
Stress management isn’t about perfection—it’s about consistency. Even small wins (5 minutes of deep breathing, 15 mins earlier bedtime) compound over time. Track progress with apps like Bearable to see how stress reduction improves your PCOS symptoms.
Key Takeaway: Cortisol reduction isn’t a luxury—it’s a non-negotiable pillar of PCOS healing. Start tonight.
Why This Works:
- Links stress to specific PCOS mechanisms (androgens, insulin).
- Provides actionable hacks (temperature, supplements, apps).
- Uses data (40% higher cortisol) to emphasize urgency.
- Balances science with relatable routines.
New chat
4. Complementary Therapies
Pair lifestyle changes with these holistic approaches:
Supplements
- Vitamin D: 60% of women with PCOS are deficient. Improves insulin sensitivity.
- Inositol: Reduces androgen levels and supports ovulation.
- Probiotics: Gut health impacts hormones—try kimchi or kefir.
Acupuncture
Studies suggest acupuncture may regulate ovulation and lower testosterone.
5. When to Seek Medical Support
While lifestyle strategies lay the foundation for PCOS management, certain scenarios demand clinical expertise to prevent irreversible complications and unlock tailored solutions. Think of your doctor as a co-pilot in your health journey—here’s when to signal for backup:
1. Stubborn Symptoms Defying Lifestyle Changes
If irregular cycles, acne, or hair loss persist after 3–6 months of consistent diet/exercise/stress management, deeper hormonal imbalances (e.g., elevated DHEA-S, prolactin) or comorbidities like thyroid dysfunction may be at play.
- Tests to Request: Full hormone panel (testosterone, SHBG, AMH), thyroid screen (TSH, T4), and inflammatory markers (CRP).
2. Fertility Roadblocks: Beyond “Just Keep Trying”
After 6–12 months of unprotected sex without conception (or 6 months if over 35), seek a reproductive endocrinologist. PCOS-related anovulation often requires medical ovulation induction:
- First-Line Treatments: Letrozole (induces ovulation in 80% of cases) or low-dose FSH injections.
- Red Flags: Irregular cycles + pelvic pain could indicate endometriosis co-occurrence.
3. Metabolic SOS Signals
Insulin resistance left unchecked can silently progress to prediabetes or cardiovascular damage. Seek urgent care if you experience:
- Acanthosis Nigricans: Velvety dark skin patches on neck/armpits.
- Unrelenting Fatigue: Despite adequate sleep, signaling glucose metabolism dysfunction.
- Neuropathy Symptoms: Tingling hands/feet (nerve damage from high blood sugar).
4. Mental Health in Crisis
PCOS triples the risk of depression and anxiety. If you’re battling:
- Persistent hopelessness or panic attacks.
- Body dysmorphia from hirsutism/weight gain.
- Binge-eating cycles triggered by insulin crashes.
→ A therapist specializing in chronic illness can provide CBT or SSRIs alongside hormonal care.
5. Preventative Proactivity: Don’t Wait for Disaster
Even if symptoms feel “manageable,” annual screenings are non-negotiable:
- Cardiovascular: Lipid panel, blood pressure check.
- Metabolic: Fasting glucose + HbA1c (goal: <5.7%).
- Reproductive: Endometrial thickness ultrasound (high estrogen raises cancer risk).
The Referral Roadmap: Which Specialist Does What?
- Endocrinologist: Manages insulin resistance, thyroid issues, and complex hormone cases.
- Reproductive Endocrinologist (REI): Fertility preservation, IVF, and ovulation disorders.
- Dermatologist: Spironolactone for acne, laser hair removal.
- Mental Health Provider: PCOS-specific CBT for body image/eating disorders.
Key Takeaway: PCOS is a multisystem condition—holistic care requires a team. Early intervention can reverse insulin resistance, prevent diabetes, and rewrite your fertility story. Book that appointment today.
FAQs
Q: Can PCOS be reversed naturally?
A: While PCOS isn’t curable, symptoms like irregular periods and insulin resistance can be managed through diet, exercise, and stress reduction.
Q: What’s the best exercise for PCOS weight loss?
A: Combine cardio (walking, cycling) with strength training to burn fat and build muscle.
Q: Do supplements really work for PCOS?
A: Yes! Vitamin D, inositol, and omega-3s have strong evidence for improving metabolic and reproductive health.
Final Thoughts
Managing PCOS naturally requires consistency, but small changes yield big results. Start with one or two strategies—like swapping processed snacks for nuts or adding daily walks—and gradually build a routine. For personalized guidance, connect with a dietitian or endocrinologist through resources like the PCOS Awareness Association.

