Gabapentin, a name synonymous with its pioneering brand Neurontin, stands as a linchpin in the pharmacological management of neurological and neuropathic disorders. Since its FDA approval in 1993, this anticonvulsant has transcended its original purpose of epilepsy treatment, evolving into a versatile ally against the searing agony of post-herpetic neuralgia and the relentless discomfort of restless leg syndrome (RLS). Its ability to temper the erratic electrical storms of seizures while silencing the phantom screams of damaged nerves has cemented its place in clinical practice. Yet, beneath its therapeutic prowess lies a complex profile of risks—sedation that blurs the line between relief and vulnerability, dependency shadows lurking in long-term use, and rare but grave adverse reactions that demand vigilance.
This guide unravels the science behind gabapentin’s mechanism, illuminating how it tames hyperactive neurons and rewires pain pathways. We delve into its FDA-sanctioned roles, navigate the minefield of drug interactions and contraindications, and arm patients and practitioners with strategies to harness its benefits while sidestepping peril. Whether you’re a patient navigating treatment options or a caregiver seeking clarity, this exploration bridges the gap between gabapentin’s promise and its pitfalls, empowering informed decisions in a landscape where efficacy and caution must coexist.
What is Gabapentin (Neurontin)?
Gabapentin, sold under the brand name Neurontin and others, is a prescription medication classified as both an anticonvulsant (anti-seizure drug) and a neuropathic pain reliever. First approved by the U.S. Food and Drug Administration (FDA) in 1993, it was initially developed to treat epilepsy but has since become a versatile therapy for nerve-related disorders. Despite its widespread use, gabapentin’s exact mechanism of action remains partially elusive—a common theme in neuroscience. Here’s what researchers understand so far:
How Does Gabapentin Work?
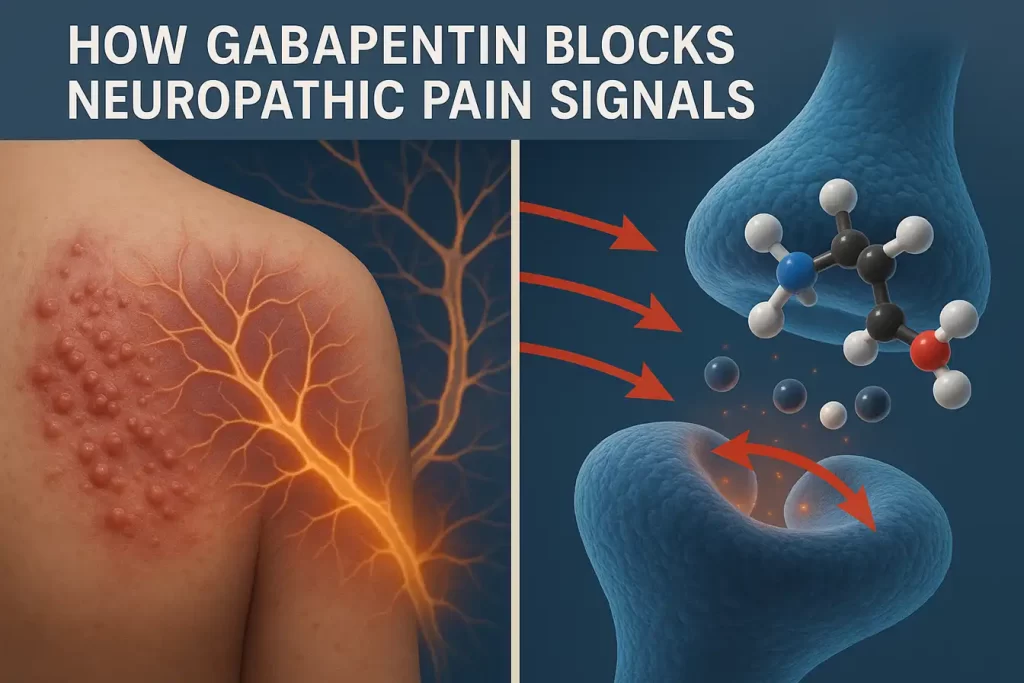
Gabapentin is structurally similar to GABA (gamma-aminobutyric acid), the brain’s primary inhibitory neurotransmitter responsible for calming overactive nerve signals. However, unlike GABA itself, gabapentin does not directly bind to GABA receptors. Instead, it targets voltage-gated calcium channels in the nervous system, specifically binding to the α2δ subunit. This action:
- Reduces Abnormal Electrical Activity: By blocking calcium influx into hyperactive neurons, gabapentin stabilizes erratic brain signals, making it effective for preventing seizures.
- Interrupts Pain Signaling: In damaged nerves (e.g., from shingles or diabetes), gabapentin dampens the release of pain-transmitting neurotransmitters like glutamate and substance P.
- Modulates Dopamine Pathways: For restless leg syndrome (RLS), it influences dopamine regulation, easing the urge to move limbs.
Primary Medical Uses
Gabapentin is FDA-approved for three key conditions:
- Epilepsy:
- Treats partial-onset seizures (focal seizures) in adults and children aged 3+.
- Often used alongside other anticonvulsants for better seizure control.
- Neuropathic Pain:
- Post-Herpetic Neuralgia: Nerve pain persisting after a shingles rash heals.
- Diabetic Neuropathy: Off-label use for burning/tingling pain in hands/feet caused by diabetes.
- Restless Leg Syndrome (RLS):
- The extended-release formulation (Horizant) is approved to relieve RLS symptoms, particularly nighttime discomfort.
Brand Names and Formulations
Gabapentin is available under multiple brands, each tailored for specific conditions:
- Neurontin:
- Original immediate-release capsules/tablets.
- Used for epilepsy and nerve pain.
- Dosed 3x daily.
- Gralise:
- Once-daily extended-release tablet.
- Approved only for post-herpetic neuralgia.
- Designed to improve compliance and steady pain relief.
- Horizant:
- Extended-release tablet for RLS and shingles pain.
- Taken once daily at night (RLS) or twice daily (nerve pain).
Note: Generic gabapentin is widely available and often prescribed due to lower cost.
Off-Label Applications
Though not FDA-approved, gabapentin is sometimes prescribed for:
- Anxiety Disorders: Limited evidence supports short-term use for generalized anxiety.
- Migraine Prevention: May reduce frequency in some patients.
- Fibromyalgia: Often combined with other therapies for pain relief.
Always consult your doctor before using gabapentin for unapproved conditions.
Key Takeaways
- Gabapentin is not a traditional painkiller—it specifically targets nerve-related pain and seizure activity.
- Its effects hinge on calming overactive nerves, but misuse (e.g., combining with opioids/alcohol) can lead to severe side effects.
- Different brands (Neurontin, Gralise, Horizant) cater to distinct medical needs—never substitute without medical guidance.
Benefits of Gabapentin: Approved Uses
1. Epilepsy Management: Stabilizing Seizure Activity
Gabapentin is FDA-approved as an adjunctive therapy for partial-onset seizures (focal seizures) in adults and pediatric patients aged 3 years and older. These seizures originate in a specific brain region and may cause localized symptoms, such as twitching or altered awareness.
- Mechanism: By binding to α2δ subunits of voltage-gated calcium channels, gabapentin reduces abnormal electrical activity in hyperexcitable neurons, preventing seizure propagation.
- Clinical Evidence: A 2020 meta-analysis in Epilepsy Research found gabapentin reduced seizure frequency by 30–40% in refractory epilepsy when combined with other anticonvulsants like levetiracetam.
- Pediatric Use: Approved for children as young as 3, though dosing is weight-based (starting at 10–15 mg/kg/day). Studies note improved tolerability compared to older antiseizure drugs.
- Limitations: Less effective for generalized seizures (e.g., tonic-clonic). Regular monitoring for drowsiness or behavioral changes in children is critical.
2. Nerve Pain Relief: Targeting Neuropathic Pathways
Gabapentin is a first-line therapy for neuropathic pain, with FDA approval for post-herpetic neuralgia (PHN) and extensive off-label use for other nerve-related conditions.
Post-Herpetic Neuralgia (PHN)
- Role: PHN, a complication of shingles, causes burning, stabbing pain persisting months after the rash resolves. Gabapentin blocks pain signals by inhibiting glutamate release in damaged nerves.
- Dosing: Start at 300 mg daily, titrating to 1,800–3,600 mg/day. The extended-release formulation Gralise (1,800 mg once daily) enhances compliance.
- Efficacy: A 2017 Journal of Pain study reported 50% pain reduction in 60% of PHN patients at 8 weeks.
Diabetic Neuropathy (Off-Label)
- Use Case: Eases burning, tingling pain in hands/feet caused by diabetic nerve damage. Though off-label, the American Diabetes Association guidelines endorse gabapentin as a Tier 1 option.
- Dosing: Similar to PHN, but lower doses (900–1,800 mg/day) often suffice.
Cancer Pain Adjunct
- Synergy with Opioids: Gabapentin enhances opioid efficacy in severe cancer pain by targeting neuropathic components. A 2016 Pain Medicine trial showed a 35% reduction in morphine doses when combined with gabapentin.
- Caution: Higher overdose risk in palliative care settings; monitor for sedation.
3. Restless Leg Syndrome (RLS): Restoring Nighttime Comfort
The extended-release formulation Horizant (gabapentin enacarbil) is FDA-approved for moderate-to-severe RLS, a sensorimotor disorder causing irresistible leg urges and discomfort at rest.
- Mechanism: Modulates thalamocortical dopamine pathways and reduces spinal cord hyperexcitability.
- Dosing: 600 mg once daily, taken 2–3 hours before bedtime. Steady-state plasma levels improve sleep continuity.
- Efficacy: In a 2021 Sleep Medicine study, 73% of patients reported “much improved” symptoms at 12 weeks, with fewer side effects than dopamine agonists (e.g., pramipexole).
- Advantage Over Immediate-Release: Horizant’s prolonged absorption minimizes peak-trough fluctuations, reducing daytime drowsiness.
Additional Considerations
- Quality of Life: Patients with PHN or RLS often report improved sleep and daily function.
- Cost-Effectiveness: Generic gabapentin is 80% cheaper than branded Horizant, though adherence may vary.
- Off-Label Potential: Emerging roles in fibromyalgia and migraine prophylaxis, albeit with mixed evidence.
Key Takeaway
Gabapentin’s versatility in epilepsy, neuropathic pain, and RLS stems from its ability to calm hyperactive nerves. However, tailored dosing and vigilant monitoring—especially in vulnerable populations—are essential to maximize benefits and mitigate risks. Always consult a healthcare provider to align treatment with your specific condition.
Risks and Side Effects of Gabapentin
Gabapentin, while effective for managing seizures, nerve pain, and restless leg syndrome (RLS), carries a spectrum of risks and side effects that demand careful consideration. Below, we delve into the physiological mechanisms, clinical evidence, and patient-specific vulnerabilities associated with its use.
Common Side Effects: Prevalence and Mechanisms
Approximately 10–20% of users experience mild-to-moderate side effects, often dose-dependent. These include:
- Central Nervous System (CNS) Effects:
- Dizziness, Drowsiness, Fatigue: Gabapentin enhances GABAergic activity, slowing neural transmission. This calming effect can impair coordination and alertness, particularly during dose escalation.
- Peripheral Edema: Fluid retention (swelling in limbs) arises from gabapentin’s modulation of calcium channels in blood vessels, increasing capillary permeability.
- Gastrointestinal Disturbances:
- Nausea, Diarrhea, Constipation: Gabapentin alters gut motility by interacting with enteric nervous system calcium channels. Diarrhea is more common during initial use, while constipation often develops with prolonged therapy.
Serious Risks: Life-Threatening Complications
1. Respiratory Depression
- FDA Warning (2019): Gabapentinoids, including gabapentin, may cause severe respiratory depression, especially in patients with COPD, asthma, or opioid co-use.
- Mechanism: Gabapentin suppresses brainstem respiratory centers, reducing CO₂ sensitivity. Risk escalates with concurrent sedatives (e.g., benzodiazepines, alcohol).
- Clinical Impact: A 2021 Chest study found a 40% higher risk of hypoxia in COPD patients on gabapentin versus controls.
2. Suicidal Ideation and Behavior
- Black Box Warning: Anticonvulsants, including gabapentin, carry a FDA-mandated warning for increased suicidal thoughts.
- Neurochemical Basis: Reduced glutamate activity may dysregulate mood pathways. A 2018 JAMA Psychiatry meta-analysis reported a 2.3-fold higher suicide risk in gabapentin users versus placebo.
- Monitoring: Patients with depression, bipolar disorder, or prior suicide attempts require close psychiatric follow-up.
3. Overdose and Toxicity
- Symptoms: Lethargy, diplopia (double vision), slurred speech, myoclonus (muscle jerks), and—in severe cases—coma. Chronic kidney disease (CKD) patients face higher overdose risks due to impaired excretion.
- Lethal Doses: Case reports cite fatalities at >50 grams, though toxicity can occur at lower doses in CKD.
- Management: Activated charcoal (if ingested <2 hours prior) and hemodialysis for critical cases.
4. Hazardous Drug Interactions
- Opioids: Synergistic CNS depression increases overdose mortality. A 2022 Annals of Internal Medicine study linked gabapentin-opioid combinations to a 60% higher fatality rate.
- Alcohol/Muscle Relaxants: Exacerbates sedation and fall risk.
- Antacids: Aluminum/magnesium antacids reduce gabapentin absorption by 20%; separate doses by 2+ hours.

High-Risk Populations: Tailored Precautions
- Older Adults (≥65 Years):
- Fall Risk: Dizziness and sedation contribute to a 30% higher fall rate in elderly users (per Journal of Gerontology).
- Dosing: Start at 100–300 mg/day, increasing slowly to avoid toxicity.
- Pregnant/Nursing Women:
- Teratogenicity: Animal studies show skeletal abnormalities, though human data are limited. The FDA categorizes gabapentin as Pregnancy Category C.
- Breastfeeding: Gabapentin excretes into milk (serum:milk ratio 1:1); monitor infants for drowsiness.
- Kidney Impairment:
- Dose Adjustments: Reduce dosage by 50–75% in CKD stages 3–5 (GFR <60 mL/min).
- Monitoring: Check serum creatinine at baseline and every 3–6 months.
Risk Mitigation Strategies
- Slow Titration: Begin with low doses (e.g., 300 mg/day) and increase weekly.
- Avoid High-Risk Combinations: Screen for opioid/sedative use; consider alternatives like pregabalin for CKD patients.
- Patient Education: Emphasize strict adherence to dosing schedules and prompt reporting of mood changes.
Key Takeaway
Gabapentin’s risks underscore the need for personalized prescribing. Clinicians must weigh benefits against vulnerabilities like respiratory compromise, mental health history, and renal function. Vigilant monitoring and patient education are paramount to safe use.
How to Use Gabapentin Safely: Dosage Guidelines
Gabapentin’s dosing requires precision to balance efficacy with tolerability. Tailored to the patient’s condition, age, renal function, and formulation, its pharmacokinetics (oral bioavailability: ~60%, renal excretion) demand careful calibration. Below, we dissect dosing protocols, titration principles, and critical safeguards to minimize risks.
Condition-Specific Dosage Protocols
| Condition | Formulation | Starting Dose | Titration Schedule | Max Daily Dose | Key Considerations |
|---|---|---|---|---|---|
| Epilepsy (Adults) | Immediate-release | 300 mg 3x daily | ↑ by 300 mg/day every 3–7 days | 3,600 mg | Split doses to maintain steady plasma levels. |
| Shingles Pain (PHN) | Gralise (XR) | 300 mg once daily | ↑ to 600 mg on Day 2, then 1,800 mg by Day 6 | 1,800 mg | Take with evening meal to enhance absorption. |
| RLS (Horizant) | Extended-release | 600 mg nightly | Fixed dose; no titration needed | 600 mg | Take at 5 PM for peak efficacy by bedtime. |
Mechanism-Driven Dosing Rationale
- Epilepsy:
- Titration: Slow escalation (e.g., 300 mg increments weekly) reduces dizziness and sedation. A 2019 Neurology trial found gradual titration lowered dropout rates by 25%.
- Peak-Trough Management: TID dosing prevents troughs that may trigger breakthrough seizures.
- Neuropathic Pain (PHN/Diabetic Neuropathy):
- Gralise XR: Once-daily dosing leverages prolonged absorption (T_max = 8 hrs) for sustained pain relief. Avoid splitting—its matrix tablet ensures 10-hour drug release.
- Threshold Dose: Studies show ≥1,800 mg/day is required for 50% pain reduction in PHN (Journal of Pain, 2017).
- RLS (Horizant):
- Nightly Timing: Aligns with dopamine’s circadian dip in RLS. Horizant’s prodrug design (gabapentin enacarbil) ensures 16-hour coverage, reducing midnight symptom flares.
Critical Safety Practices
1. Renal Dosing Adjustments
Gabapentin is 100% renally excreted. For CKD patients:
- GFR 30–59 mL/min: Reduce dose by 50%.
- GFR 15–29 mL/min: Reduce dose by 75%.
- Hemodialysis: 200–300 mg supplemental dose post-treatment.
Example: A CKD patient with GFR 40 mL/min on epilepsy therapy would take 150 mg 3x daily (vs. standard 300 mg).
2. Food and Drug Interactions
- Food: Enhances absorption of immediate-release by 10–15%. Exception: Horizant requires empty stomach for optimal prodrug conversion.
- Antacids: Aluminum hydroxide reduces AUC by 20%. Administer gabapentin ≥2 hours after antacids.
3. Missed Dose Protocol
- <2 hours late: Take immediately.
- >2 hours late: Skip to avoid double-dosing.
- Frequent Misses: Consider once-daily XR formulations (e.g., Gralise) to improve adherence.
High-Risk Populations: Special Guidance
- Elderly (≥65): Start at 100–200 mg nightly to assess tolerance. Monitor for gait instability.
- Pregnancy: Use lowest effective dose; neonatal withdrawal (tremors, irritability) reported post-delivery.
- Substance Use Disorder: Avoid in patients with opioid/alcohol dependence due to misuse potential.
Tapering Guidelines
Abrupt cessation risks withdrawal (agitation, insomnia). Taper by:
- >3,600 mg/day: Reduce by 300 mg daily every 3 days.
- <1,800 mg/day: Reduce by 100–200 mg weekly.
Final Takeaway
Gabapentin’s safety hinges on meticulous dosing aligned with renal function, formulation kinetics, and comorbidity risks. Always pair pharmacotherapy with patient education on adherence, side effect monitoring, and tapering protocols.
Gabapentin FAQs
1. Is gabapentin a muscle relaxer?
Originally studied as a muscle relaxant, gabapentin is now primarily used for seizures and nerve pain.
2. Does gabapentin lower blood pressure?
Animal studies suggest it may reduce hypertension, but human data is lacking. Monitor BP with your doctor.
3. Can gabapentin cause weight gain?
Yes—increased appetite and fluid retention may lead to weight gain in 2–3% of users.
4. Is gabapentin addictive?
While not a controlled substance, some states track it due to misuse risks. Taper off slowly to avoid withdrawal.
Key Takeaways
- Therapeutic Efficacy with Vigilance
- Versatile Relief: Gabapentin is a cornerstone treatment for epilepsy, neuropathic pain (e.g., post-herpetic neuralgia, diabetic neuropathy), and restless leg syndrome (RLS), offering significant symptom control by stabilizing hyperactive nerve signals.
- Mechanism Insight: By binding to α2δ subunits of voltage-gated calcium channels, it reduces aberrant neuronal firing—calming seizures and dampening pain pathways.
- Common vs. Severe Side Effects: A Balancing Act
- Frequent but Manageable: Up to 20% of users experience dizziness, peripheral edema, or fatigue. These often subside with dose adjustments or slow titration.
- Life-Threatening Risks:
- Respiratory Depression: Potentially fatal in high doses or when combined with opioids, particularly in those with COPD/asthma.
- Neuropsychiatric Hazards: FDA warnings highlight increased suicidal ideation (2.3x higher risk vs. placebo) and rare cases of aggression or hallucinations.
- Critical Safeguards for Safe Use
- Transparency is Key: Disclose all medical conditions (e.g., kidney disease, mental health history) and medications (e.g., opioids, antacids, sedatives) to preempt dangerous interactions.
- Dosage Discipline:
- Renal Adjustments: Reduce doses by 50–75% for kidney impairment (GFR <60 mL/min).
- Avoid Sudden Cessation: Taper gradually (e.g., 300 mg/week) to prevent withdrawal (insomnia, agitation).
- High-Risk Populations: Special Considerations
- Elderly: Higher fall risk due to sedation; start at 100 mg nightly.
- Pregnancy/Nursing: Limited safety data; weigh fetal risks vs. seizure control.
- Substance Use History: Monitor for misuse potential—gabapentin misuse rates have risen 90% since 2015.
- Emergency Protocols
- Overdose Signs: Double vision, slurred speech, lethargy. Immediate action: Call 911 and administer naloxone if opioids are involved.
- Mental Health Crisis: If suicidal thoughts emerge, contact the 988 Suicide & Crisis Lifeline or seek emergency care.
Final Note: Gabapentin’s power lies in its precision—use it as a scalpel, not a hammer. Regular check-ins with your healthcare provider and adherence to dosing guidelines are non-negotiable for harnessing its benefits while mitigating peril.
FAQ
1. What is Gabapentin (Neurontin) primarily prescribed for?
Gabapentin is primarily an anti-seizure medication also approved to treat nerve pain (neuropathic pain). Common conditions include postherpetic neuralgia (from shingles) and restless legs syndrome. It is also widely used off-label for conditions like anxiety, migraines, and fibromyalgia.
2. How does Gabapentin work for nerve pain?
While the exact mechanism isn’t fully known, Gabapentin is believed to calm nerve activity. It mimics the action of a calming brain chemical called GABA (gamma-aminobutyric acid). By binding to specific channels in the brain and nervous system, it reduces the abnormal electrical activity and signaling that cause seizures and the sensation of nerve pain.
3. What are the most common side effects of Gabapentin?
The most frequent side effects are dizziness, drowsiness, fatigue, and coordination problems. Others may include peripheral edema (swelling in extremities), weight gain, and blurred vision. These often lessen as your body adjusts. It’s crucial to avoid driving or operating machinery until you know how the medication affects you.
4. What is the correct way for how to take gabapentin for nerve pain effectively?
Effectively taking Gabapentin for nerve pain involves several key steps:
- Follow Dosage Instructions: Always take it exactly as prescribed. The dose is typically started low and gradually increased (titrated) over time to minimize side effects and find the lowest effective dose.
- Consistency is Key: Take it at the same times each day to maintain a steady level in your bloodstream.
- Administration: You can take it with or without food. However, taking it with food can help reduce stomach upset and may improve absorption.
5. Is Gabapentin addictive? Can you experience withdrawal?
Gabapentin is not classified as a controlled substance at the federal level in the U.S., but some states have reclassified it due to potential for misuse. Physical dependence can develop with long-term use. Stopping abruptly can cause withdrawal symptoms like anxiety, insomnia, nausea, pain, and sweating. It is essential to never stop taking it suddenly and to taper off gradually under a doctor’s supervision.
6. What are the serious side effects or warnings I should know about?
Seek immediate medical attention if you experience signs of a severe allergic reaction, suicidal thoughts, or unusual changes in mood or behavior. A rare but serious side effect is respiratory depression, especially when combined with opioids or other CNS depressants. Gabapentin can also worsen depression and cause significant drowsiness.
7. Can I drink alcohol while taking Gabapentin?
No, it is not recommended. Alcohol can intensify Gabapentin’s side effects, particularly extreme dizziness, severe drowsiness, and impaired motor control. Combining them significantly increases the risk of accidents and can worsen depression or breathing difficulties.
8. What drugs interact dangerously with Gabapentin?
Dangerous interactions can occur with:
- Opioids (like hydrocodone, oxycodone): Increases risk of severe sedation, respiratory depression, and death.
- Other CNS Depressants (like benzodiazepines, sleep aids, certain antidepressants): Can amplify drowsiness and dizziness.
- Antacids containing aluminum or magnesium: Can reduce Gabapentin absorption. Take Gabapentin at least 2 hours after taking an antacid.
9. Who should not take Gabapentin or use it with extreme caution?
Individuals with a known allergy to Gabapentin should not take it. Extreme caution is needed for:
- Those with kidney problems (dosage must be adjusted).
- The elderly (more sensitive to side effects like dizziness).
- Individuals with a history of depression, mood disorders, or suicidal thoughts.
- Pregnant or breastfeeding women (only if clearly needed, as risks to the fetus/infant are possible).
Sources
- FDA Gabapentin Safety Communication (2019).
- Journal of Pain Research (2017): Gabapentin for neuropathic pain.
- Neurology (2020): Gabapentin use in pregnancy.
About the author
Max Wild is a health writer and researcher focused on cancer awareness, prevention, and patient education. He translates complex medical topics into simple, practical guidance so readers can have more informed conversations with their doctors.

