Are you locked in a frustrating battle with deep, painful bumps that stubbornly camp out on your lower face? If you’ve tried every cream, wash, and internet hack only to see them return again and again, you’re not alone—and you’re not doing anything wrong. What you’re experiencing is the classic signature of Hormonal Chin Acne.
Unlike surface-level breakouts, Hormonal Chin Acne is an internal battle. But that doesn’t mean you are powerless against it. This guide is your definitive roadmap, designed to dive deep into the root causes and provide you with a clear, actionable plan to finally conquer these stubborn breakouts and achieve the clear, confident skin you deserve.
What Exactly is Hormonal Acne? It’s More Than Just “That Time of the Month”
When you hear “hormonal acne,” you might immediately think of a single pimple that pops up before your period. But true Hormonal Chin Acne is often a more persistent and frustrating issue. It’s a chronic skin condition primarily driven by internal shifts in your body’s chemistry, not just a monthly blip.
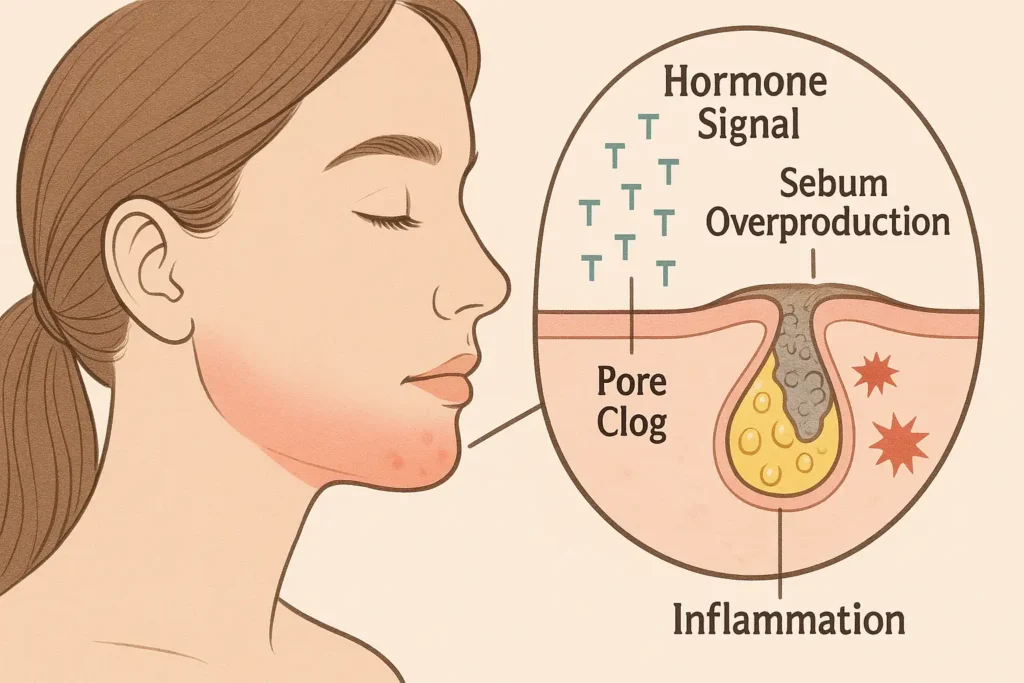
Think of your hormones as messengers telling your body what to do. For Hormonal Chin Acne, the key messengers are androgens, which are hormones like testosterone. It’s a common misconception that only men have testosterone; women produce it too, just in smaller amounts. The problem arises when these androgen levels fluctuate or your skin’s oil glands become overly sensitive to them.
Here’s a step-by-step look at what happens inside your skin:
- The Signal: Androgen hormones (like testosterone) surge or your skin becomes more reactive to them. This can be triggered by your menstrual cycle, stress, diet, or underlying conditions like PCOS.
- The Overproduction: These androgens act like a “start your engines” signal to your sebaceous (oil) glands, telling them to go into overdrive and produce excess sebum (oil).
- The Clog: This surplus of thick, sticky oil mixes with dead skin cells that are naturally shedding inside your pore. Instead of flowing out smoothly, they form a sticky plug, effectively clogging the pore.
- The Inflammation: Inside this clogged, oil-rich pore, bacteria that normally live on your skin (called C. acnes) begin to multiply rapidly. Your body’s immune system recognizes this as a problem and sends inflammatory cells to attack, resulting in the red, swollen, and painful bumps known as cystic acne.
So, why the chin and jawline?
This area is sometimes called the “hormonal mask” because the pores here have a high concentration of hormone receptors. They are simply more sensitive and responsive to the internal fluctuations of androgens than the pores on, say, your cheeks or forehead. This is why Hormonal Chin Acne acts as a direct billboard for what’s happening inside your body.
The Tell-Tale Signs: Is Your Chin Acne Really Hormonal?
Not all breakouts are created equal. While bacteria and clogged pores play a role in all acne, Hormonal Chin Acne has a distinct “personality” that sets it apart. If your go-to acne products aren’t making a dent, it’s a strong clue that your hormones are the primary drivers.
Ask yourself these key questions to see if your skin is sending you hormonal signals:
1. Location, Location, Location: The “Hormonal Mask”
If your breakouts consistently target your lower face—specifically your chin, jawline, and the upper neck—you’re likely dealing with hormonal issues. This area is rich in hormone-sensitive oil glands. In contrast, T-zone breakouts (forehead and nose) are more often linked to surface-level issues like excess oil and bacteria.
2. Type of Blemishes: The Deep, Painful Cysts
This is one of the most telling signs. Hormonal Chin Acne typically manifests as:
- Papules and Nodules: These are the deep, tender, red bumps that feel hard to the touch. They linger under the skin’s surface without a visible head.
- Cysts: The most severe form, these are soft, painful, fluid-filled lumps deep within the skin. They are the most likely to cause post-acne scarring.
Unlike the blackheads and whiteheads of comedonal acne or the pus-filled pustules of bacterial acne, these hormonal blemishes are like underground rebels—difficult to reach and treat with topical products alone.
3. Timing is Everything: The Flare-Up Forecast
For women, your menstrual cycle is a major clue. Do breakouts predictably erupt 7 to 10 days before your period starts and then begin to calm down once it arrives? This pattern is a near-certain indicator of hormonal involvement. Other key hormonal life stages that can trigger it include pregnancy, perimenopause, and the months after starting or stopping birth control pills.

4. Adult Onset: The “Second Puberty” Surprise
Hormonal Chin Acne frequently appears or worsens in your 20s, 30s, 40s, and beyond. Many women who had clear skin as teenagers are baffled when they develop persistent chin acne as adults. This adult-onset pattern is a hallmark of the condition.
5. Stubborn and Slow to Heal: The Lingering Aftermath
These blemishes are notoriously resistant to standard over-the-counter benzoyl peroxide or salicylic acid washes. Even when the painful swelling subsides, they leave a lasting mark—literally. Post-inflammatory hyperpigmentation (PIH), the dark or red spots that remain long after the pimple is gone, is very common with hormonal acne because of the significant inflammation involved.
If you’re nodding along to most of these signs, you can be confident that you’re dealing with Hormonal Chin Acne—and the treatment approach needs to match the cause.
The Root Causes: Uncovering Your Personal Triggers
Understanding that your chin acne is hormonal is the first step; the next, crucial step is pinpointing your unique triggers. Hormonal Chin Acne rarely has a single cause. It’s often a perfect storm of several internal and external factors. By identifying the specific contributors in your life, you can create a targeted and effective action plan.
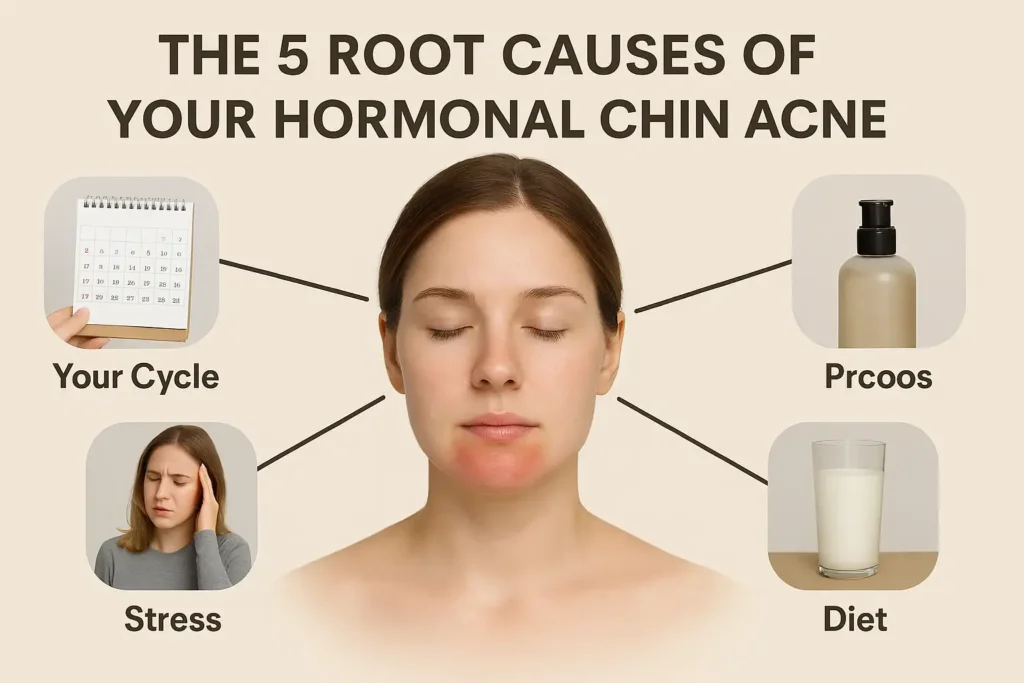
The Menstrual Cycle Rollercoaster
This is the most common trigger for people with cyclical periods. It’s not just about one hormone, but a delicate dance between several:
- The Shift: In the week before your period, estrogen and progesterone levels, which were high, plummet dramatically.
- The Androgen Effect: This sudden drop unmasks the effect of androgens (like testosterone), which remain relatively stable. With the calming influence of estrogen gone, these androgens have a more potent effect on your oil glands.
- The Result: This hormonal shift is a direct signal for your sebaceous glands to go into overdrive, leading to the classic pre-menstrual flare-up of deep, painful cysts along the jawline and chin.
PCOS and Other Underlying Conditions
For some, persistent Hormonal Chin Acne is a symptom of a broader metabolic condition.
- Polycystic Ovary Syndrome (PCOS): This condition is characterized by insulin resistance and elevated levels of androgens. The high androgens directly stimulate excess oil production, leading to stubborn, often treatment-resistant acne that is concentrated on the lower face. Key signs that may point to PCOS include irregular periods, excess facial or body hair (hirsutism), and hair thinning on the scalp.
- Other Imbalances: Issues with adrenal glands or other endocrine disorders can also cause similar hormonal fluctuations and skin manifestations.
Stress and Cortisol
Your skin is a direct reflection of your internal stress levels.
- The Cascade: When you’re stressed (physically or emotionally), your body releases the hormone cortisol.
- Inflammation and Oil: Elevated cortisol levels directly increase inflammation throughout the body, worsening the redness and swelling of acne. It can also signal your oil glands to produce more sebum, creating a fertile ground for new breakouts. This is why high-stress periods often lead to major flare-ups.
Diet and Dairy Connection
The saying “you are what you eat” holds significant truth for hormonal acne.
- High-Glycemic Foods: Foods like white bread, sugar, pasta, and pastries cause a rapid spike in your blood sugar and insulin levels. High insulin can boost androgen activity and may influence oil production, creating a cascade that ends in a breakout.
- Dairy: The connection is strongest with skim milk. Dairy from pregnant cows contains growth hormones and growth factors that can interact with our own human hormones, particularly insulin-like growth factor 1 (IGF-1), which can stimulate oil glands and worsen acne for some individuals.
Certain Hair and Skin Products
Sometimes, the culprit is right in your bathroom cabinet. This is known as acne cosmetica or “pomade acne.”
The Solution: The skin on your chin and jawline is particularly vulnerable to this, as products from your hair and face easily migrate there. Always look for labels that say “non-comedogenic,” “oil-free,” or “won’t clog pores.”
The Problem: Heavy, occlusive ingredients in products can create a physical barrier that traps oil, dead skin cells, and bacteria inside your pores. Common offenders include thick facial creams, oil-based hair serums, pomades, and even some silicone-heavy primers.
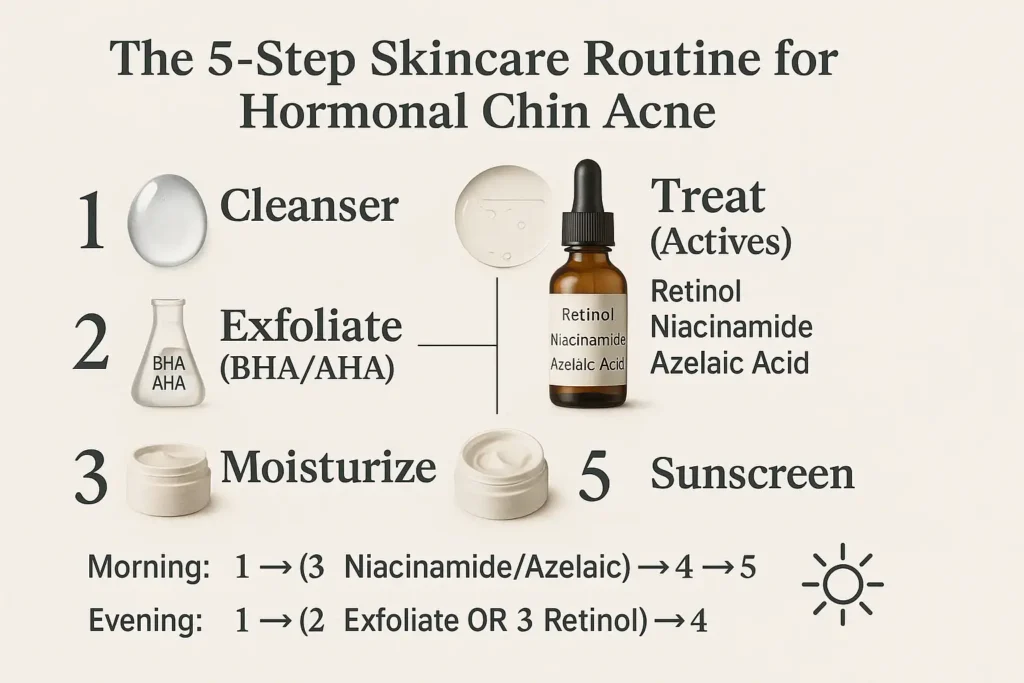
Your At-Home Skincare Arsenal: Building the Right Routine
CoConsistency is your greatest weapon against Hormonal Chin Acne. While internal factors drive the breakout, the right topical routine is essential for managing inflammation, unclogging pores, preventing new cysts from forming, and healing the skin’s barrier. This isn’t about aggressive stripping; it’s about strategic, gentle, and targeted care.
Here is your step-by-step blueprint for a routine that works with your skin, not against it.
Step 1: Gentle Cleansing (Without Stripping)
The Goal: To remove impurities, excess oil, and makeup without compromising your skin’s protective barrier.
Why it Matters: Harsh, sulfate-based cleansers strip your skin of all its natural oils. This might feel “squeaky clean,” but it actually signals your oil glands to produce even more oil to compensate, worsening the problem. It also damages your skin barrier, leading to more irritation and sensitivity.
How to Do It Right:
- Look For: A gentle, pH-balanced (around 5.5), sulfate-free, and fragrance-free cleanser.
- Key Ingredients: Cream or gel formulas with hydrating agents like glycerin, ceramides, or hyaluronic acid.
- Frequency: Morning and night. In the PM, consider double-cleansing if you wear makeup or sunscreen: first with an oil-based cleanser to break down products, then with your water-based gentle cleanser.
Step 2: Exfoliation is Key (AHAs vs. BHAs)
The Goal: To dissolve the clogs deep within pores and sweep away dead skin cells that contribute to blockages.
Why it Matters: This is non-negotiable for fighting the deep-seated clogs of hormonal acne. Chemical exfoliants are far more effective and gentle than abrasive physical scrubs for this skin concern.
How to Choose & Use:
- BHAs (Beta Hydroxy Acids/Salicylic Acid): YOUR MVP.
- Why: Salicylic acid is oil-soluble. This unique property allows it to penetrate into the pore lining, dissolving the mixture of sebum and dead skin cells that form painful cysts and blackheads. It’s anti-inflammatory and truly gets to the root of the clog.
- How to Use: Apply 2-3 times per week in a leave-on formula (serum or toner) after cleansing and before moisturizing.
- AHAs (Alpha Hydroxy Acids like Glycolic & Lactic Acid):
- Why: These are water-soluble and work on the skin’s surface. They are excellent for smoothing skin texture, fading post-acne dark spots (hyperpigmentation), and boosting radiance.
- How to Use: Use 1-2 times per week, often alternating with your BHA. Do not overuse, as this can lead to irritation.
Step 3: Treat with Targeted Actives
The Goal: To directly address oil production, inflammation, and bacteria with concentrated ingredients.
Why it Matters: This is where you deploy your specialized troops to tackle the specific mechanisms of hormonal acne.
Your Power Players:
- Retinoids (Start with OTC Retinol):
- The Gold Standard: They accelerate skin cell turnover, preventing dead cells from clogging pores. They are also powerfully anti-inflammatory and stimulate collagen, which helps heal scars.
- How to Use: Start with an over-the-counter retinol 2-3 nights a week on dry skin, after cleansing but before moisturizing. CRUCIAL: Always use sunscreen the next day, as retinoids increase sun sensitivity.
- Niacinamide (Vitamin B3):
- The Multi-Tasking Hero: This ingredient is a game-changer. It helps regulate sebum production, calms redness, strengthens the skin barrier, and fades discoloration. It’s gentle enough for daily use.
- How to Use: A 5-10% concentration serum can be used morning and/or night after cleansing.
- Azelaic Acid:
- The Underrated Powerhouse: Brilliant for reducing the inflammation and redness of active cysts. It also kills acne-causing bacteria and is exceptionally effective at fading the post-acne marks that hormonal acne leaves behind.
- How to Use: Can be used daily or on alternate days, often in the morning. It pairs very well with retinoids at night (applied after the retinol).
Step 4: Moisturize to Repair Your Barrier
The Goal: To hydrate, soothe, and fortify your skin’s natural barrier.
Why it Matters: A damaged skin barrier is more vulnerable to irritation, bacteria, and transepidermal water loss. Keeping it healthy makes your skin more resilient, less reactive, and better able to heal. Even oily, acne-prone skin needs hydration.
How to Do It Right:
- Look For: A lightweight, oil-free, and non-comedogenic (won’t clog pores) formula.
- Key Ingredients: Seek out ceramides, niacinamide, panthenol, and hyaluronic acid to hydrate and repair without heaviness.
Step 5: Don’t Forget Sunscreen!
The Goal: To protect your skin from UV-induced inflammation and prevent dark spots from worsening.
Why it Matters: Sun exposure is a major source of inflammation, which can worsen active breakouts. Furthermore, the dark spots (post-inflammatory hyperpigmentation) left by hormonal acne become significantly darker and more permanent when exposed to UV rays. Many acne treatments also increase photosensitivity.
How to Do It Right:
Frequency: Apply it as the final step of your morning routine, every single day, rain or shine.
Look For: A broad-spectrum, lightweight, oil-free, non-comedogenic sunscreen with at least SPF 30.
Lifestyle and Diet Changes: Supporting Your Skin from the Inside Out
While a targeted skincare routine manages the symptoms on the surface, achieving long-term clarity from Hormonal Chin Acne requires addressing the internal factors that fuel it. Think of your body as a complex ecosystem; what you feed it and how you treat it directly influences your hormone balance and inflammatory response. This holistic approach is what ultimately breaks the cycle for good.
Foods to Embrace: Building an Anti-Inflammatory Foundation
Focus on incorporating nutrient-dense, whole foods that actively fight inflammation and support stable blood sugar.
- Omega-3 Fatty Acids: Your Natural Anti-Inflammatories
- Why: These essential fats are powerful inflammation-lowering agents. By countering the inflammatory response that creates painful, red cysts, they help calm your skin from the inside.
- Sources: Fatty fish like salmon, mackerel, and sardines; plant-based options like walnuts, chia seeds, and flaxseeds.
- Antioxidant-Rich Foods: Combatting Cellular Stress
- Why: Oxidative stress can worsen inflammation and skin damage. Antioxidants neutralize these free radicals, promoting healing and protecting your skin cells.
- Sources: “Eat the rainbow.” Focus on berries (blueberries, raspberries), dark leafy greens (spinach, kale), bright vegetables (bell peppers, carrots), and green tea.
- Zinc: The Regulating Mineral
- Why: Zinc plays a role in wound healing, reducing inflammation, and may even help regulate oil production. Studies have shown it can be effective in reducing acne severity.
- Sources: Pumpkin seeds, lentils, chickpeas, cashews, and quinoa.
Foods to Consider Limiting: Identifying Your Personal Triggers
Pay close attention to how your skin reacts to these common dietary culprits. You don’t need to eliminate them forever, but a 4-6 week elimination trial can reveal powerful insights.
- High-Glycemic Foods: The Blood Sugar Rollercoaster
- Why: Foods that spike your blood sugar (white bread, pasta, pastries, candy, sugary drinks) cause a corresponding spike in insulin. Elevated insulin levels can increase androgen activity and boost oil production, directly fueling the hormonal acne cycle.
- Action: Swap refined carbs for complex ones like oats, sweet potatoes, and whole grains to maintain stable blood sugar.
- Dairy: A Complex Trigger
- Why: The link is strongest with skim milk. Dairy contains growth hormones and milk proteins (like whey and casein) that may stimulate insulin and IGF-1 production, which in turn can influence oil glands and clog pores. This effect is highly individual.
- Action: Try eliminating all dairy (especially milk, yogurt, and whey protein) for a month. Observe if your skin calms down. If you reintroduce it, note any changes.
Stress Management Techniques: Calming Your Cortisol
Chronic stress is a direct trigger for Hormonal Chin Acne. Managing it is not a luxury; it’s a critical part of your treatment plan.
- Prioritize Sleep (Aim for 7-9 hours):
- Why: During deep sleep, your body repairs itself and regulates key hormones, including cortisol. Skimping on sleep keeps cortisol elevated, leading to more oil and more inflammation.
- Tip: Create a relaxing bedtime routine and keep your room dark and cool.
- Move Your Body (Regularly but Not Excessively):
- Why: Exercise is a powerful tool for balancing hormones and reducing stress. It improves insulin sensitivity and boosts endorphins. However, intense, prolonged exercise can sometimes increase cortisol, so balance is key.
- Tip: Find joyful movement you enjoy, like brisk walking, yoga, dancing, or cycling.
- Practice Mindfulness (Even 10 Minutes a Day):
- Why: Activities like meditation, deep breathing exercises, or journaling actively lower cortisol levels. They signal to your nervous system that it’s safe to relax, dialing down the inflammatory response that worsens acne.
- Tip: Use a meditation app or simply focus on taking 10 slow, deep breaths when you feel stressed.
When to See a Dermatologist: Professional Treatments That Work
If your at-home efforts aren’t enough after a few months, it’s time to call in the pros. A dermatologist can provide powerful solutions that target the hormonal source.
Topical Prescriptions
- Prescription-Strength Retinoids: Like Tretinoin or Adapalene gel, which are far more potent than OTC retinol.
- Topical Antibiotics: Like Clindamycin, to reduce bacteria.
Oral Medications
- Oral Contraceptives: Certain birth control pills (like Yaz, Ortho Tri-Cyclen) that contain both estrogen and progestin can effectively balance hormones and clear acne.
- Spironolactone: This is a game-changer for many women. It’s a medication that blocks androgen receptors, directly reducing oil production. It is not suitable for men or pregnant women.
- Oral Antibiotics: Used short-term to quickly bring severe inflammation under control.
In-Office Procedures
- Cortisone Injections: A dermatologist can inject a diluted steroid directly into a large, painful cyst, shrinking it dramatically within 24-48 hours.
- Chemical Peels: Professional peels with high concentrations of salicylic or glycolic acid can deeply exfoliate and clear pores.
What NOT to Do: Common Mistakes That Make Chin Acne Worse
- Over-washing or Scrubbing Harshly: This irritates your skin, damages your barrier, and can make acne worse.
- Picking or Popping Cysts: This pushes bacteria deeper, increases inflammation, and significantly raises the risk of scarring and dark spots.
- Using Comedogenic Products: Avoid heavy oils, butters, and occlusive ingredients on your chin.
- Neglecting Your Phone Screen and Pillowcases: These are breeding grounds for bacteria and oil. Clean them regularly!
FAQ: Your Top Questions About Hormonal Chin Acne, Answered
How long does it take to see results?
Patience is vital. With a consistent routine, you may see some improvement in 6-8 weeks. It can take 3 months or more to see significant, lasting results, especially with hormonal treatments like birth control or Spironolactone.
Can men get hormonal acne on the chin?
Absolutely. While the triggers may differ (often related to genetics and natural androgen fluctuations), men are just as susceptible to hormonal acne on the chin and jawline.
What is the difference between hormonal acne and fungal acne?
Hormonal acne presents as inflamed, often painful cysts. Fungal acne (malassezia folliculitis) typically appears as uniform, itchy, small red bumps. They require completely different treatments, so a correct diagnosis is key.
Are there any natural remedies that work?
While not a substitute for a proven routine, some natural options may help support skin health. Spearmint tea has anti-androgen properties, and zinc supplements can reduce inflammation. Always consult with a doctor before starting any new supplements.
Conclusion: Your Path to Clearer Skin Starts Now
Getting rid of stubborn hormonal chin acne is a journey that requires a multi-faceted approach. There is no single magic bullet, but by combining a targeted skincare routine, mindful lifestyle changes, and professional help when needed, you can break the cycle.
Your skin doesn’t have to be a source of frustration. Be patient with your body, consistent with your routine, and remember that you have the power to take control. Your journey to clearer, calmer skin starts today.
Ressources
- American Academy of Dermatology (AAD) – Acne Resource Center
- Link: https://www.aad.org/public/diseases/acne
- Why it’s helpful: The gold standard for patient-friendly, dermatologist-reviewed information on acne causes, treatments, and skin care.
- British Association of Dermatologists – Acne Patient Information Leaflet
- Link: https://www.bad.org.uk/pils/acne/
- Why it’s helpful: Provides a comprehensive and clear overview of acne, including different types and treatment options, from a leading UK dermatological body.
- Journal of the American Academy of Dermatology (JAAD)
- Link: https://www.jaad.org/
- Why it’s helpful: For those interested in the deep science, this is a premier peer-reviewed journal where many clinical studies on acne treatments are published. (Note: Some articles may be behind a paywall).
Clinical Studies & Evidence-Based Research
- The Role of Diet in Acne and Rosacea (Journal of the American Academy of Dermatology)
- Link: https://www.jaad.org/article/S0190-9622(17)32270-9/fulltext
- Why it’s helpful: A review of the current evidence on diet (including dairy and high-glycemic foods) and its impact on acne.
- Spironolactone for the Treatment of Acne in Women: A Retrospective Study (The Journal of Clinical and Aesthetic Dermatology)
- Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2923944/
- Why it’s helpful: A key study highlighting the effectiveness and safety of Spironolactone for adult female acne.
- National Institutes of Health (NIH) – Polycystic Ovary Syndrome (PCOS)
- Link: https://www.nichd.nih.gov/health/topics/pcos
- Why it’s helpful: A reliable resource to learn more about PCOS, a common underlying cause of hormonal acne.
Skincare Ingredient & Product Education
- Paula’s Choice Ingredient Dictionary
- Link: https://www.paulaschoice.com/ingredient-dictionary
- Why it’s helpful: An unbiased, research-backed database that explains how common skincare ingredients (like BHAs, Niacinamide, and Retinoids) work.
- Lab Muffin Beauty Science
- Link: https://labmuffin.com/
- Why it’s helpful: A blog and YouTube channel run by a PhD in Chemistry, offering clear, science-based explanations of skincare myths and ingredients.
Mental Health & Support
- Mind – How to Cope with the Mental Health Impact of Skin Conditions
- Link: https://www.mind.org.uk/information-support/types-of-mental-health-problems/skin-conditions-and-mental-health/
- Why it’s helpful: Acne can significantly impact self-esteem and mental well-being. This resource offers valuable support and coping strategies.
- Anxiety and Depression Association of America (ADAA)
- Link: https://adaa.org/
- Why it’s helpful: Provides resources for managing stress and anxiety, which are known triggers for hormonal acne.

