Picture a silent hero within you—a dynamic, muscular tunnel that delivers every bite and sip to your stomach. This is your esophagus, the unsung workhorse of digestion. But when cancer strikes this vital conduit, it often begins as a stealthy invader, masking its presence until crucial treatment windows narrow. By the time symptoms like agonizing swallows or unexplained weight loss sound the alarm, the battle becomes urgent. Early detection isn’t just advantageous—it can be transformative, shifting outcomes from dire to hopeful.
This guide pulls back the curtain on esophageal cancer, exposing its elusive early warnings, demystifying its progression through critical stages (0 to IV), and mapping the route to elite specialists armed with cutting-edge therapies. Whether you’re navigating a new diagnosis or advocating for a loved one, consider this your compass to specialized care—where expertise meets urgency, and knowledge becomes your greatest ally.
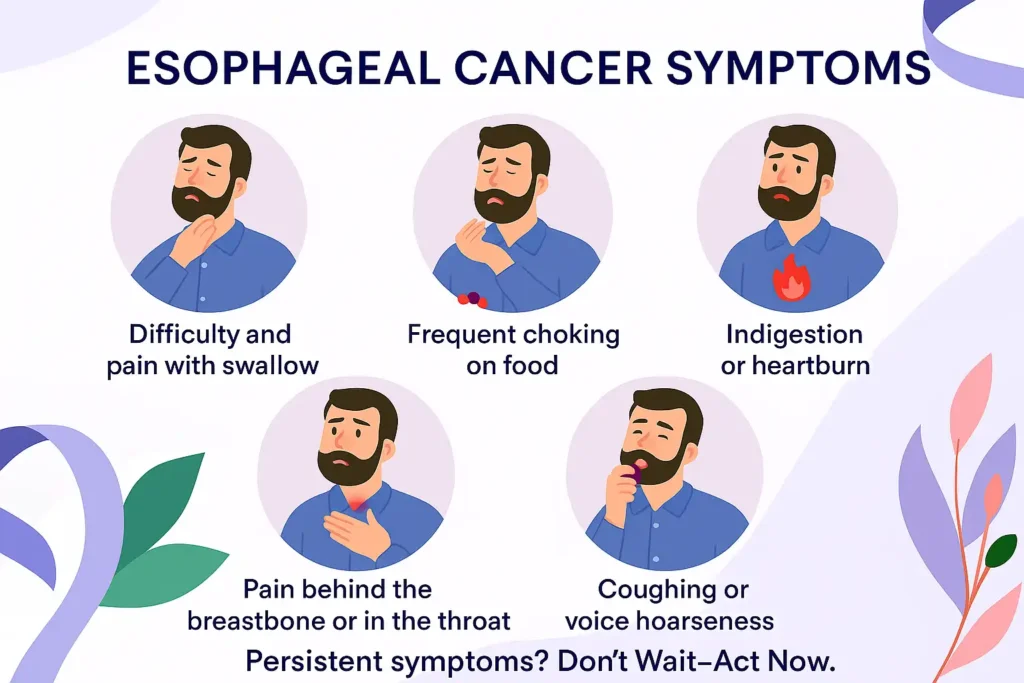
Recognizing Esophageal Cancer Symptoms
EsopThe Silent Onset: Why Early Symptoms Go Unnoticed
Esophageal cancer is a master of disguise in its initial phases. Unlike other cancers that trigger immediate alarms, it often lurks undetected because the esophagus—a flexible, muscular tube—can stretch and adapt, masking early abnormalities. Here’s how symptoms evolve:
Early Warning Signs (Often Overlooked)
- “Silent Phase”: No obvious red flags.
- Persistent Indigestion: Recurring heartburn or mild chest discomfort, easily mistaken for GERD or stress.
- Subtle Fatigue: Mild anemia caused by slow, unnoticed bleeding in the esophagus.
Why it’s missed: These mimic common gastrointestinal issues. High-risk individuals (smokers, chronic GERD patients) often dismiss them.
Advanced Symptoms: When the Body Sounds the Alarm
As tumors grow or spread, the esophagus narrows, and systemic effects emerge:
- Dysphagia (Difficulty Swallowing):
- Solids feel “stuck” (like a pill lodged in the throat).
- Progresses to trouble swallowing liquids.
- Unexplained Weight Loss:
- Rapid loss of 10+ pounds without dieting.
- Linked to reduced appetite and metabolic changes.
- Hoarseness & Chronic Cough:
- Tumors press on the laryngeal nerve or irritate the airway.
- Coughing worsens at night or after eating.
- Chest Pain or Burning:
- Persistent discomfort behind the breastbone, unrelated to heartburn.
- Hematemesis (Blood in Vomit):
- Bright red or coffee-ground-like vomit signals bleeding tumors.
When to Act:
*”Don’t wait for all symptoms to align. If you experience two or more of these signs for 2+ weeks—especially with risk factors like smoking, heavy alcohol use, or GERD—seek urgent evaluation. Early imaging or endoscopy can be lifesaving.”*
– National Cancer Institute Guidelines
Section-Specific Image Prompt:
Visual Concept:
*”A split-screen infographic contrasting early vs. advanced esophageal cancer symptoms. Left side: A calm, blue-toned esophagus with subtle icons (small heartburn flame, faint fatigue shadow). Right side: A red-alert esophagus with visible tumors, a person clutching their throat, a downward-tipping scale, and crossed-out cigarettes/alcohol. Bottom: A diverse doctor holding a ‘2+ Weeks’ calendar, urging action.”*
Style & Elements:
Call-to-Action: Doctor pointing to a calendar with “2+ Weeks” highlighted.
Color Palette: Early stage (cool blues/greys), advanced stage (urgent reds/oranges).
Icons:
Early: Faint flame (heartburn), shadow figure (fatigue).
Advanced: Tumors blocking the esophagus, blood droplets, weight scale.
Risk Factors: Cigarette, wine bottle, acid reflux graphic.
Staging Esophageal Cancer: From 0 to IV
Decoding the Stages: How Far Has the Cancer Spread?
Staging is the roadmap oncologists use to predict outcomes, tailor therapies, and gauge urgency. The TNM system—developed by the American Joint Committee on Cancer (AJCC)—classifies tumors based on three pillars:
- T (Tumor): Size and depth of the primary tumor.
- N (Nodes): Spread to nearby lymph nodes.
- M (Metastasis): Presence of distant organ involvement.
Here’s a breakdown of esophageal cancer stages, their clinical implications, and survival insights:
| Stage | Description |
|---|---|
| Stage 0 | Abnormal cells (pre-cancer) in the inner lining. |
| Stage I | Small tumor within the esophagus wall. |
| Stage II | Spread to deeper layers or nearby lymph nodes. |
| Stage III | Invasion into adjacent organs (e.g., trachea) or multiple lymph nodes. |
| Stage IV | Metastasis to distant organs (liver, lungs). |
Diagnostic Tools: Mapping the Cancer’s Footprint
- Endoscopy:
- What it shows: Direct visualization of tumors, ulcers, or strictures.
- Patient experience: Sedation is used; a thin tube with a camera is inserted through the mouth.
- Biopsy:
- Purpose: Confirms cancer type (adenocarcinoma vs. squamous cell carcinoma).
- Key insight: Genetic testing on biopsy samples can reveal targets for immunotherapy (e.g., PD-L1 expression).
- Imaging:
- CT/PET Scans: Detect lymph node involvement and distant metastases.
- Barium Swallow: Highlights structural abnormalities via X-ray after swallowing contrast dye.
How to Find Specialized Care for Esophageal Cancer
Navigating the Maze: Building Your Expert Care Network
Esophageal cancer demands a precision-driven approach, and the quality of your care team can profoundly impact outcomes. Here’s how to assemble a multidisciplinary squad and access cutting-edge resources:
1. Assemble a Multidisciplinary Dream Team
Esophageal cancer treatment requires seamless collaboration. Prioritize these specialists:
- Surgical Oncologists: Seek those trained in minimally invasive esophagectomy (MIE), which reduces recovery time vs. open surgery.
- Key credential: Fellowship in thoracic or gastrointestinal surgery.
- Medical Oncologists: Look for expertise in immunotherapy (e.g., pembrolizumab) and targeted therapies (HER2 inhibitors for adenocarcinoma).
- Radiation Oncologists: Prioritize those using intensity-modulated radiation therapy (IMRT) to spare healthy tissue.
Where to Find Them:
- NCI-Designated Cancer Centers: These NIH-recognized hubs (e.g., MD Anderson, Dana-Farber) offer:
- Access to clinical trials for refractory cases.
- Tumor boards where specialists collaborate on complex cases.
- Volume Matters: Choose hospitals performing 50+ esophagectomies/year; high-volume centers have lower mortality rates (Annals of Surgery, 2023).
2. Master the Consultation: 10 Critical Questions to Ask
Turn appointments into actionable intel with this strategic checklist:
Diagnosis & Staging:
- “What is my cancer’s histologic subtype (squamous cell vs. adenocarcinoma), and how does that affect treatment?”
- “Has my tumor been tested for biomarkers like PD-L1, HER2, or MSI status?”
Treatment Strategy:
3. “Is neoadjuvant therapy (pre-surgery chemo/radiation) recommended to shrink my tumor?”
4. “What are the long-term survival rates for my stage with this approach?”
Surgical Details:
5. “Will my surgery be robot-assisted or open? What’s your complication rate?”
6. “How will we manage post-op nutrition (e.g., feeding tubes)?”
Support & Survivorship:
7. “Can I meet with a dysphagia specialist to address swallowing issues?”
8. “Do you partner with palliative care teams for pain management?”
Second Opinions:
9. “Can you refer me to a NCI center for a second opinion?”
10. “What clinical trials am I eligible for?”
3. Tap Into Authoritative Resources: Beyond Google
For Treatment Guidelines
- National Cancer Institute (NIH):
- Esophageal Cancer Treatment PDQ – Updated, evidence-based protocols.
- Also in Spanish: Instituto Nacional del Cáncer.
For Emotional & Practical Support
- American Cancer Society (ACS):
- 24/7 Helpline: Connects you to local support groups and financial aid.
- “Living as an Esophagus Cancer Survivor” – Diet, exercise, and mental health guides.
For Cutting-Edge Science
- ClinicalTrials.gov:
- Search terms: “Esophageal squamous cell carcinoma immunotherapy” or “metastatic adenocarcinoma targeted therapy.”
- Filter by phase (I-III), location, and biomarker eligibility.
En Español:
- Sociedad Americana Contra El Cáncer:
- Cáncer de esófago – Guías de tratamiento y videos educativos.
Prevention and Risk Reduction
Defending Your Esophagus: Science-Backed Strategies to Slash Your Risk
While esophageal cancer can’t always be prevented, research reveals that proactive lifestyle changes and vigilant management of pre-cancerous conditions can dramatically reduce risk. Here’s how to fortify your defenses:
1. Quit Smoking: Break Free from a Leading Carcinogen
- The Hard Truth: Smokers face 2-5x higher risk of squamous cell carcinoma (the most common esophageal cancer type worldwide). Toxins in cigarette smoke, like nitrosamines, directly damage esophageal DNA.
- Action Plan:
- Nicotine Replacement Therapy (NRT): Patches or lozenges double quit rates (CDC, 2023).
- Behavioral Support: Apps like QuitGenius or free counseling (1-800-QUIT-NOW).
- Did You Know?: Risk declines by 50% within 5 years of quitting (Journal of the National Cancer Institute).
2. Limit Alcohol: Protect Your Mucosal Lining
- The Science: Alcohol metabolizes into acetaldehyde, a DNA-mutating compound. Heavy drinkers (3+ drinks/day) have 3-8x higher risk of squamous cell carcinoma.
- Smart Swaps:
- Cap Intake: ≤1 drink/day for women, ≤2 for men (1 drink = 5 oz wine).
- Hydrate Strategically: Alternate alcohol with water to reduce esophageal exposure.
- Avoid “Double Threats”: Smoking + drinking multiplies risk synergistically (up to 100x in some studies).
3. Tame Acid Reflux: Stop GERD Before It Becomes Barrett’s Esophagus
Why It Matters: Chronic GERD inflames the esophagus, triggering cellular changes (Barrett’s esophagus) that raise adenocarcinoma risk by 30-125x.
Proactive Management:
- Dietary Shifts:
- Avoid: Spicy foods, caffeine, chocolate (relax the lower esophageal sphincter).
- Embrace: Alkaline foods like bananas, melons, and oatmeal to neutralize acid.
- Medication:
- PPIs (e.g., omeprazole): Reduce acid production but use the lowest effective dose long-term.
- H2 Blockers (e.g., famotidine): For nighttime breakthrough symptoms.
- Monitor Barrett’s: If diagnosed, undergo bi-annual surveillance endoscopies to catch dysplasia early.
4. Eat to Outsmart Cancer: Build a Bioactive Shield
Anti-Cancer Plate Formula:
- 50% Cruciferous Veggies: Broccoli, kale, and Brussels sprouts contain sulforaphane, which inhibits tumor growth (Cancer Prevention Research, 2022).
- 25% Whole Grains: High-fiber diets reduce esophageal inflammation; aim for 30g/day.
- 25% Lean Protein: Choose fish (omega-3s combat inflammation) over processed meats (nitrites linked to adenocarcinoma).
Ditch These Risks:
- Scalding Hot Drinks: >149°F (65°C) liquids increase squamous cell risk (International Journal of Cancer).
- Processed Meats: Bacon, sausages, and deli meats are Group 1 carcinogens (WHO).
5. Weight Management: The GERD-Obesity Link
- Excess belly fat pressures the stomach, forcing acid into the esophagus. Losing 5-10% body weight can halve reflux episodes.
- Exercise Smart: Opt for low-impact activities (yoga, swimming) over heavy lifting, which can worsen reflux.
Key Takeaways:
- Quit smoking with NRT + counseling—your esophagus heals faster than you think.
- GERD is not “just heartburn”—untreated, it’s a gateway to pre-cancer.
- Fill your plate like a pharmacologist—every bite can be chemo-preventive.
Free Resource:
- NCI Diet Guide: What to Eat During Cancer Treatment.
- En Español: Guía de alimentación del Instituto Nacional del Cáncer.
Frequently Asked Questions
QQ1: Can Esophageal Cancer Be Detected Early?
A: Early detection remains a formidable challenge due to the esophagus’s resilient structure and vague initial symptoms. However, strategic surveillance can alter outcomes for high-risk groups:
- High-Risk Populations:
- Barrett’s Esophagus Patients: Annual or bi-annual surveillance endoscopies with biopsy to detect dysplasia (pre-cancer).
- Chronic GERD Sufferers: Those with >5 years of weekly reflux symptoms.
- Lynch Syndrome Carriers: Genetic predisposition increases adenocarcinoma risk.
- Emerging Tools:
- Cytosponge: A swallowable sponge that collects esophageal cells for TP53 mutation testing (90% sensitivity in trials).
- Biomarker Panels: Blood tests detecting CFDNA (circulating tumor DNA) are under study.
Bottom Line: While routine screening isn’t advised for the general population, high-risk individuals should insist on endoscopic monitoring—*early-stage detection boosts 5-year survival to 47% vs. 5% for metastatic disease*.
Q2: What’s the Survival Rate for Esophageal Cancer?
A: Survival hinges on stage, histology, and treatment access. Here’s the breakdown (SEER Database, 2023):
| Stage | 5-Year Survival | Key Influencing Factors |
|---|---|---|
| Localized (I) | 47% | – Tumor depth – No lymph node involvement |
| Regional (II-III) | 25% | – Response to neoadjuvant therapy – Surgical margins |
| Metastatic (IV) | 5% | – Metastasis sites (liver vs. bone) – Biomarker-driven therapies (e.g., HER2+) |
Critical Notes:
- Histology Matters: Adenocarcinoma (common in the West) has slightly better prognosis than squamous cell carcinoma (linked to smoking/alcohol).
- Innovation Impact: Immunotherapy (e.g., nivolumab) has doubled 1-year survival in Stage IV trials (NEJM, 2022).
Q3: Is Esophageal Cancer Linked to Diet?
A: Absolutely. Diet acts as both sword and shield in esophageal cancer risk:
Risk Amplifiers:
- Processed/Red Meats: Nitrosamines in bacon and sausages directly damage esophageal DNA. Daily consumption raises adenocarcinoma risk by 20% (WHO IARC).
- Scalding Beverages: Drinking tea/coffee >65°C (149°F) increases squamous cell carcinoma risk 8-fold (International Journal of Cancer).
- Low-Fiber Diets: Linked to chronic inflammation and GERD.
Protective Foods:
- Cruciferous Vegetables: Sulforaphane in broccoli induces cancer cell apoptosis.
- Berries: Anthocyanins inhibit tumor angiogenesis.
- Whole Grains: Fiber reduces bile acid reflux, a GERD trigger.
Global Case Study:
The “Asian Esophageal Cancer Corridor” (Iran to China) highlights diet’s role: populations consuming pickled vegetables (high in Fusarium fungi carcinogens) have 10x higher squamous cell rates.
Q4: How Does GERD Progress to Cancer?
A: The GERD → Barrett’s Esophagus → Adenocarcinoma sequence unfolds over decades:
- Chronic Acid Exposure: Stomach acid erodes the squamous epithelium.
- Metaplasia: Damaged cells transform into acid-resistant columnar cells (Barrett’s).
- Dysplasia: Genetic hits (e.g., TP53 mutations) turn Barrett’s into high-grade dysplasia.
- Adenocarcinoma: Invasive cancer develops in 0.5-1% of Barrett’s patients yearly.
Intervention Window:
- Radiofrequency Ablation (RFA): Eradicates Barrett’s with 90% efficacy if caught early.
Q5: Are New Treatments Improving Survival?
A: Precision oncology is rewriting the rulebook:
- Immunotherapy: Pembrolizumab (Keytruda) boosts survival in PD-L1+ tumors.
- Targeted Therapies: Trastuzumab (HER2 inhibitor) for HER2+ adenocarcinoma.
- MINAR Trial (2023): Minimally invasive surgery + neoadjuvant chemo reduced recurrence by 40%.
Clinical Trial Access:
Search ClinicalTrials.gov for “esophageal cancer CAR-T” or “KRAS inhibitor” trials.
Key Takeaway: Esophageal cancer is no longer a death sentence—knowledge, early action, and cutting-edge care are shifting survival curves.
Need Clarification?
ACS Nutrition Guide: Diet Tips During Treatment.
NIH Genetic Counseling: Esophageal Cancer Risk Assessment.
Key Takeaways
Your Action Plan Against Esophageal Cancer: Knowledge, Expertise, and Hope
Esophageal cancer is a stealthy adversary, but arming yourself with awareness and decisive action can tilt the odds in your favor. Let this be your battle blueprint:
- Heed Your Body’s Alarms:
- Persistent swallowing struggles or unexplained hoarseness are not mere inconveniences—they’re red flags demanding swift medical scrutiny. Think of your esophagus as a vital highway; blockages (tumors) only grow costlier with delay.
- Stage Dictates Strategy:
- Cancer staging isn’t just a label—it’s a roadmap to survival. Seek care at NCI-Designated Cancer Centers, where multidisciplinary teams deploy precision tools like immunotherapy and minimally invasive surgery. Remember: Where you’re treated is as critical as how.
- Prevention is Power:
- Slash your risk by extinguishing cigarettes, taming acid reflux (GERD), and embracing a plant-forward diet. Barrett’s esophagus? Treat it as a code-red prelude—regular endoscopies can intercept cancer’s march.
- Survival is a Team Sport:
- From clinical trials exploring CAR-T cell therapy to dysphagia specialists restoring swallow function, your care squad should be as specialized as your cancer.
Urgent Support at Your Fingertips:
- 🚨 American Cancer Society Hotline: *1-800-227-2345* – 24/7 guidance for emotional support, clinical trial matching, and financial aid navigation.
- 🔍 Find a GI Expert: Tap the ASGE Doctor Finder – vetted specialists skilled in cutting-edge diagnostics and therapies.
Final Thought:
While esophageal cancer’s 5-year survival rates remain sobering, modern oncology is rewriting endings. Every early endoscopy, lifestyle shift, and second opinion inches us closer to turning the tide. Your next move could save a life—possibly your own.


1 thought on “Esophagus Cancer 101: Symptoms, Stages, and How to Find Specialized Care”