Mental disorders are health conditions marked by significant disruptions in a person’s thinking, emotional regulation, or behavior, often causing distress and impairing their ability to function socially, professionally, or personally. According to the National Institute of Mental Health (NIMH), 1 in 5 U.S. adults grappled with a mental disorder in 2021, with anxiety and depressive disorders ranking as the most common. Clinicians rely on the *Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5)*—the gold standard for classification—to accurately diagnose these conditions and guide treatment plans. This guide delves into the types, symptoms, and evidence-based therapies for mental disorders, equipping readers with actionable insights to pursue timely, effective care.
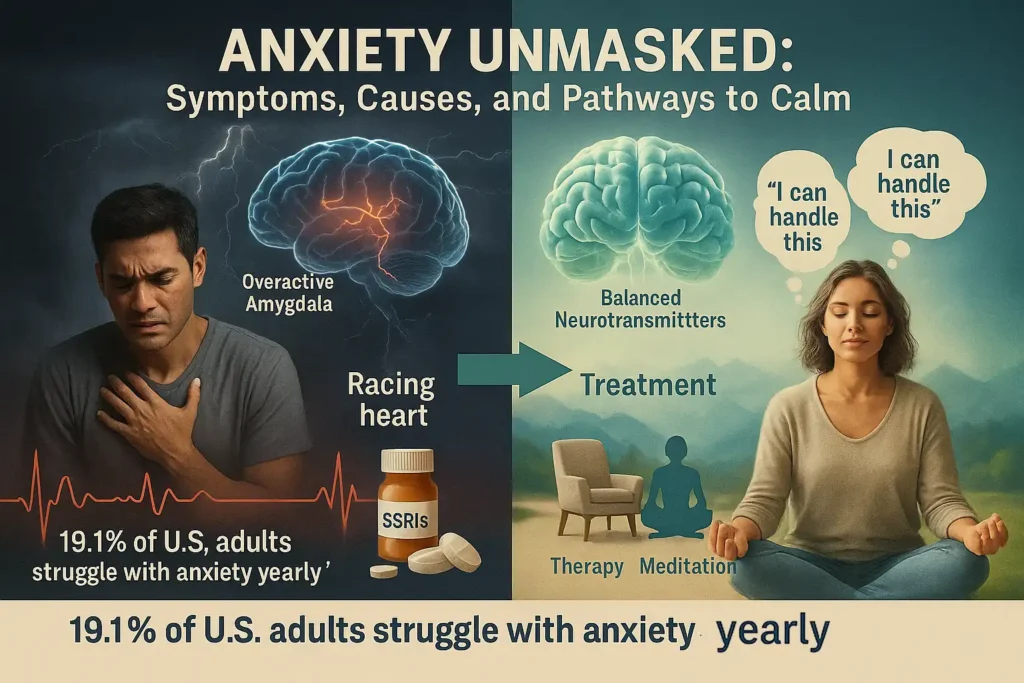
1. Anxiety Disorders
Anxiety disorders are a cluster of mental health conditions characterized by persistent, excessive fear or anxiety that severely disrupts daily life. Unlike temporary stress, these disorders involve symptoms that linger for months or years, often escalating without treatment.
Mechanism: Anxiety arises from hyperactivity in the brain’s amygdala (the “fear center”) and imbalances in neurotransmitters like serotonin and norepinephrine. This triggers a heightened “fight-or-flight” response, even in non-threatening situations.
Symptoms:
- Psychological: Intrusive worries, irrational fears, anticipatory anxiety.
- Physical: Sweating, trembling, chest tightness, gastrointestinal distress.
- Behavioral: Avoidance of triggers (e.g., skipping social events), compulsive rituals (e.g., excessive handwashing).
Examples:
- Generalized Anxiety Disorder (GAD):
- Chronic worry about everyday issues (health, finances) for ≥6 months.
- Prevalence: 3.1% of U.S. adults.
- Panic Disorder:
- Sudden panic attacks with symptoms mimicking heart attacks (e.g., palpitations, derealization).
- Prevalence: 2.7% of U.S. adults.
- Social Anxiety Disorder:
- Crippling fear of embarrassment, leading to avoidance of public speaking or social gatherings.
- Prevalence: 7.1% of U.S. adults.
DSM-5 Criteria:
- Symptoms must persist ≥6 months, cause significant distress, and impair work/social functioning.
- Rule out substance-induced anxiety (e.g., caffeine, medications).
Treatment:
- First-line: Cognitive Behavioral Therapy (CBT) to reframe negative thoughts.
- Medications: SSRIs (e.g., sertraline), SNRIs (e.g., venlafaxine).
- Lifestyle: Mindfulness meditation, diaphragmatic breathing.
Expert Insight:
“Anxiety isn’t a choice—it’s a misfiring of the brain’s alarm system. Early intervention with CBT can rewire neural pathways.” — Dr. Emily Carter, Clinical Psychologist
2. Bipolar and Related Disorders
Bipolar and related disorders are complex mental health conditions defined by extreme, cyclical shifts in mood, energy, and cognition, oscillating between manic highs and depressive lows. These fluctuations are not mere mood swings but severe disruptions rooted in dysregulation of neurotransmitters like dopamine and serotonin, often requiring lifelong management.
Mechanism: During manic phases, the brain’s prefrontal cortex (responsible for decision-making) becomes underactive, while the limbic system (emotional center) hyperactivates. Conversely, depressive episodes involve reduced activity in reward pathways and elevated stress hormones like cortisol.
Symptoms:
- Manic Episodes:
- Psychological: Grandiosity, racing thoughts, impulsivity (e.g., reckless spending).
- Physical: Reduced need for sleep (≤3 hours/night), hyperactivity.
- Behavioral: Risky decisions (substance abuse, hypersexuality).
- Depressive Episodes:
- Psychological: Hopelessness, suicidal ideation, anhedonia (loss of pleasure).
- Physical: Fatigue, weight changes, psychomotor retardation.
- Behavioral: Social withdrawal, neglect of responsibilities.
Examples:
- Bipolar I Disorder:
- Manic episodes lasting ≥7 days, often requiring hospitalization.
- Prevalence: 1% of U.S. adults.
- *DSM-5 Criteria*: Mania + major depressive episodes (in 90% of cases).
- Bipolar II Disorder:
- Hypomania (less severe mania) + recurrent depressive episodes.
- Prevalence: 1.4% of U.S. adults.
- *DSM-5 Criteria*: No full manic episodes; hypomania lasts ≥4 days.
Prevalence: Affects 2.8% of U.S. adults, with 83% classified as severe (NIMH, 2021).
Treatment:
- Medications: Mood stabilizers (e.g., Lithium), antipsychotics (e.g., Abilify).
- Therapy: Interpersonal and Social Rhythm Therapy (IPSRT) to stabilize daily routines.
- Lifestyle: Sleep hygiene, avoiding stimulants (caffeine, alcohol).

Expert Insight:
“Bipolar disorder isn’t a life sentence—it’s a manageable condition. Early diagnosis and mood tracking apps can prevent episodes from derailing lives.” — Dr. Sarah Lin, Psychiatrist
3. Depressive Disorders
Depressive disorders are debilitating mental health conditions marked by persistent sadness, anhedonia (loss of pleasure), and cognitive impairments that corrode a person’s ability to function. Rooted in dysregulation of serotonin, norepinephrine, and dopamine systems, these disorders are more than “feeling down”—they alter brain structure, reducing hippocampal volume and prefrontal cortex activity over time.
Mechanism: Chronic stress and genetic vulnerability disrupt the hypothalamic-pituitary-adrenal (HPA) axis, leading to elevated cortisol levels. This impairs neuroplasticity, perpetuating cycles of despair and cognitive fog.
Symptoms:
- Psychological: Guilt, worthlessness, suicidal ideation.
- Physical: Psychomotor agitation or retardation, unexplained aches.
- Behavioral: Social withdrawal, neglect of self-care, reduced productivity.
Examples:
- Major Depressive Disorder (MDD):
- ≥5 symptoms (e.g., sleep changes, fatigue) lasting ≥2 weeks.
- Prevalence: 8.4% of U.S. adults (21 million people).
- Persistent Depressive Disorder (Dysthymia):
- Chronic low mood + 2+ symptoms for ≥2 years.
- Prevalence: 1.5% of U.S. adults.
- Seasonal Affective Disorder (SAD):
- Depression recurring annually, linked to reduced sunlight.
- Prevalence: 5% of U.S. adults.
DSM-5 Criteria:
- ≥5 symptoms (including depressed mood or anhedonia) present daily for ≥2 weeks.
- Rule out medical causes (e.g., hypothyroidism, Parkinson’s).
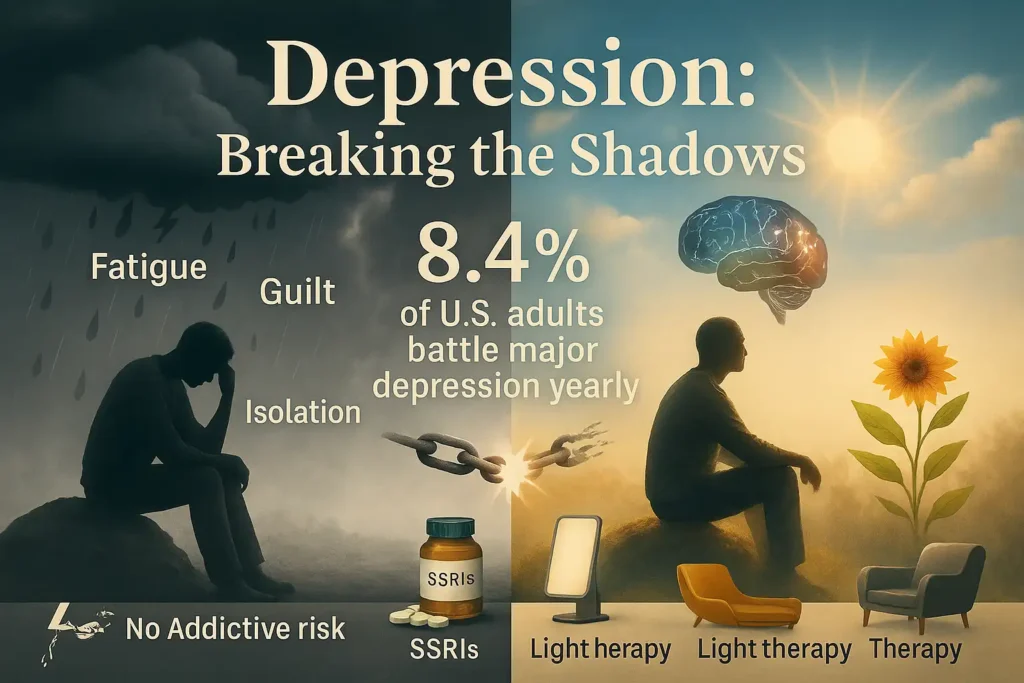
Treatment:
- First-line: SSRIs (e.g., escitalopram) + Cognitive Behavioral Therapy (CBT).
- Advanced: Transcranial Magnetic Stimulation (TMS) for treatment-resistant cases.
- Lifestyle: Light therapy (for SAD), aerobic exercise (boosts BDNF).
Expert Insight:
“Depression is a thief—it steals joy, energy, and hope. But with the right treatment, the brain can heal. Never underestimate the power of early intervention.” — Dr. Rachel Nguyen, Neuropsychiatrist
4. Dissociative Disorders
Dissociative disorders are profound disruptions in consciousness, identity, memory, or perception, often arising as a psychological survival mechanism to cope with overwhelming trauma. These conditions fragment a person’s sense of self, creating barriers between thoughts, emotions, and memories. Rooted in severe stress or abuse (often during childhood), dissociation serves as the brain’s “circuit breaker” to escape unbearable realities.
Mechanism: Trauma hyperactivates the amygdala while suppressing the prefrontal cortex, impairing memory integration. The hippocampus—critical for memory consolidation—shrinks, leading to gaps in autobiographical recall. Neurotransmitter imbalances (e.g., low serotonin) further destabilize emotional regulation.
Symptoms:
- Psychological: Identity confusion, “out-of-body” experiences (depersonalization), emotional numbness.
- Cognitive: Amnesia for traumatic events, time loss (e.g., “losing” hours or days).
- Behavioral: Sudden shifts in speech/mannerisms, finding unfamiliar items in possession.
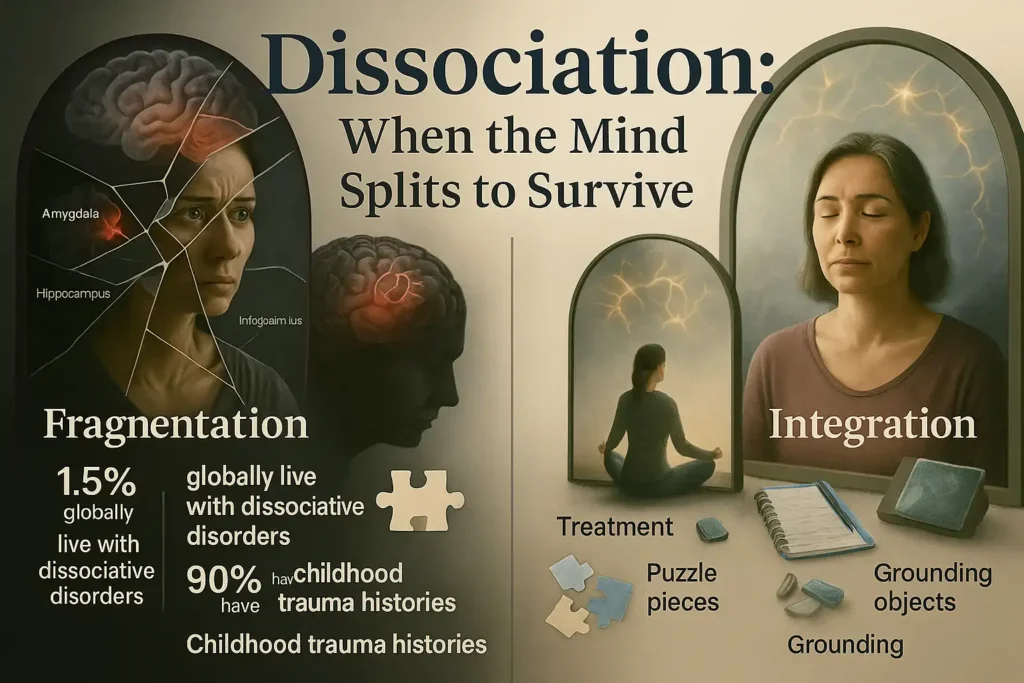
Examples:
- Dissociative Identity Disorder (DID):
- Formerly “multiple personality disorder,” DID involves ≥2 distinct identity states with unique memories, behaviors, and emotional patterns.
- Prevalence: 1–1.5% globally; often misdiagnosed for 7–10 years.
- *DSM-5 Criteria*: Disruption of identity + recurrent amnesia, not attributable to substances.
- Dissociative Amnesia:
- Inability to recall personal information, often surrounding trauma (e.g., abuse, combat).
- Subtypes: Localized (specific events), selective (parts of events), generalized (whole identity).
Treatment:
- Phase-Oriented Therapy: Stabilization (safety), trauma processing (EMDR), reintegration.
- Medications: Off-label use of SSRIs for comorbid depression/anxiety.
- Grounding Techniques: Sensory exercises (e.g., holding ice, naming objects) to anchor in the present.
Expert Insight:
“Dissociation isn’t ‘faking’—it’s the mind’s desperate attempt to protect itself. Recovery requires rebuilding trust, often over years.” — Dr. Elena Martinez, Trauma Specialist
5. Feeding and Eating Disorders
Feeding and eating disorders are severe mental health conditions characterized by extreme, obsessive behaviors around food, weight, and body image, often driven by a distorted self-perception and intense fear of gaining weight. These disorders are not lifestyle choices but biologically influenced illnesses, rooted in genetic, neurochemical, and psychosocial factors. They disrupt physical health, social functioning, and emotional stability, with mortality rates among the highest of any mental illness.
Mechanism: Dysregulation in the hypothalamus (appetite control) and serotonin/dopamine pathways skew reward processing, while societal pressures and trauma exacerbate perfectionism and control-seeking behaviors. For example, anorexia nervosa is linked to overactivity in the brain’s insula, which heightens interoceptive awareness (hyperfocus on body signals).
Symptoms:
- Psychological: Preoccupation with calories, “good vs. bad” food fixation, guilt after eating.
- Physical: Electrolyte imbalances, amenorrhea, gastrointestinal damage (from purging).
- Behavioral: Secretive eating, ritualistic habits (e.g., cutting food into tiny pieces), excessive exercise.
Examples:
- Anorexia Nervosa:
- Restrictive subtype: Severe calorie restriction, BMI ≤17.5.
- Binge-purge subtype: Alternating restriction with purging behaviors.
- Prevalence: 0.3–0.6% of the population; 10% mortality rate within 10 years.
- Bulimia Nervosa:
- Recurrent binge-eating followed by compensatory behaviors (vomiting, laxatives).
- Prevalence: 1–1.5% of the population; often comorbid with anxiety/depression.
- Binge-Eating Disorder (BED):
- Consuming large quantities rapidly without purging, accompanied by shame.
- Prevalence: 2.8% of U.S. adults; most common eating disorder.

DSM-5 Criteria:
- Anorexia: Restriction leading to significantly low weight + intense fear of weight gain.
- Bulimia: Recurrent bingeing/purging ≥1x/week for 3 months.
- BED: Bingeing ≥1x/week for 3 months without compensatory behaviors.
Treatment:
- Medical Stabilization: Address malnutrition, cardiac risks.
- Therapy: CBT-E (Enhanced Cognitive Behavioral Therapy), Family-Based Therapy (FBT).
- Medications: SSRIs (e.g., fluoxetine) for bulimia/BED.
- Nutritional Counseling: Meal planning to restore metabolic balance.
Expert Insight:
“Eating disorders thrive in secrecy. Recovery begins when we replace shame with compassion and challenge the myth that thinness equals worth.” — Dr. Laura Hill, Eating Disorder Specialist
6. Gender Dysphoria
Gender dysphoria is a clinically significant distress arising from the incongruence between a person’s gender identity and their sex assigned at birth, often accompanied by a profound desire to align physical characteristics, social roles, and/or legal identity with their true gender. This condition is not a mental illness itself but a recognized medical diagnosis that validates the emotional and psychological toll of societal stigma and body mismatch. Rooted in neurobiological and psychosocial factors, gender dysphoria can emerge in childhood, adolescence, or adulthood, necessitating individualized, affirming care.
Mechanism: Research suggests that gender identity may be influenced by prenatal hormone exposure and brain structure differences (e.g., in the BSTc region). Societal rejection and lack of access to affirming care exacerbate distress, increasing risks of anxiety (52% prevalence) and depression (48% prevalence) among transgender individuals.
Symptoms:
- Psychological: Intense discomfort with gendered body parts (e.g., chest, genitalia), rejection of birth name/pronouns, social withdrawal.
- Behavioral: Seeking gender-affirming interventions (hormones, surgery), adopting clothing/hairstyles aligning with gender identity.
- Social: Distress in gendered spaces (e.g., bathrooms, locker rooms), avoidance of mirrors/photos.

DSM-5 Criteria:
- Duration: Distress or impairment lasting ≥6 months.
- Exclusions: Not better explained by other mental disorders (e.g., body dysmorphia).
- Subtypes: With/without a disorder of sex development (e.g., intersex conditions).
Prevalence:
- Transgender Adults: ~1.6 million in the U.S. (0.6% of adults), with 35–50% experiencing clinical gender dysphoria.
- Youth: 1.8% of high school students identify as transgender, many reporting dysphoria pre-puberty.
Treatment:
- Medical: Hormone replacement therapy (HRT), surgeries (e.g., top surgery, vaginoplasty).
- Social: Legal name/gender marker changes, pronoun affirmation.
- Psychological: Gender-affirming therapy, support groups (e.g., Trans Lifeline).
Expert Insight:
“Gender dysphoria isn’t about ‘changing’ who you are—it’s about becoming who you’ve always been. Affirmation saves lives, reducing suicide risk by 73%.” — Dr. Jamie Feldman, Transgender Health Specialist
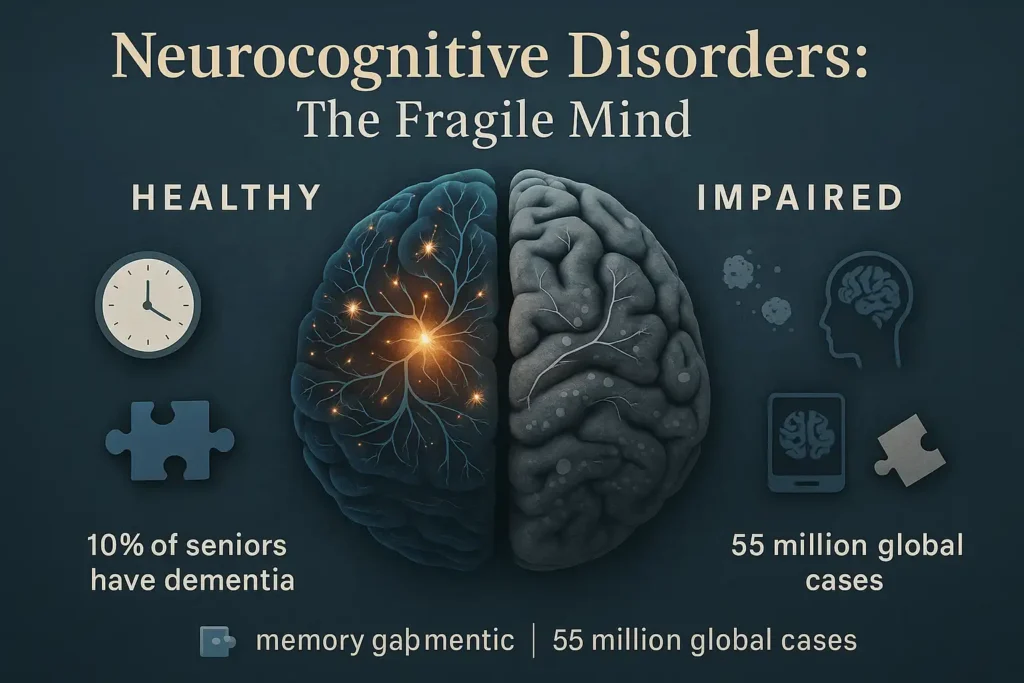
7. Neurocognitive Disorders
Neurocognitive Disorders (NCDs) are conditions marked by significant cognitive decline in domains such as memory, reasoning, or language, impacting daily functioning. These disorders arise from brain damage or disease, with severity ranging from mild (subtle deficits) to major (severe impairment).
Examples & Mechanisms:
- Alzheimer’s Disease: Characterized by beta-amyloid plaques and tau tangles, causing progressive memory loss. Accounts for 60-80% of dementia cases.
- Traumatic Brain Injury (TBI): Results from external force (e.g., concussion), leading to attention deficits, memory issues, or executive dysfunction.
- Vascular Dementia: Caused by cerebrovascular damage (e.g., stroke), impairing decision-making and processing speed.
Symptoms:
- Memory lapses (e.g., forgetting recent conversations)
- Difficulty planning tasks or solving problems
- Language struggles (e.g., word-finding issues)
- Personality changes (e.g., apathy, agitation)
Prevalence:
- ~10% of U.S. adults aged 65+ have dementia; 22% of TBI survivors experience long-term cognitive deficits.
- Global dementia cases: 55 million, projected to triple by 2050 (WHO).
DSM-5 Criteria:
- Major NCD: Significant decline interfering with independence (e.g., needing help with finances).
- Mild NCD: Modest decline without functional impairment.
- Diagnosis requires clinical assessment (e.g., Montreal Cognitive Assessment) and neuroimaging (MRI, PET).
Treatment:
- Pharmacological: Cholinesterase inhibitors (donepezil) for Alzheimer’s; symptom management for TBI.
- Non-Pharmacological: Cognitive rehabilitation, caregiver education, lifestyle modifications (diet, exercise).
Expert Insight:
“Early detection of NCDs can slow progression. Cognitive decline isn’t inevitable aging—it’s a medical issue requiring intervention.” — Dr. Maria Lopez, Neurologist
8. Neurodevelopmental Disorders
Neurodevelopmental disorders are lifelong conditions originating in early brain development, marked by impairments in cognitive, social, or motor functioning that impact learning, behavior, and independence. Rooted in genetic, epigenetic, and environmental factors (e.g., prenatal exposure to toxins), these disorders reflect atypical neural connectivity and neurotransmitter imbalances (e.g., dopamine in ADHD). Early diagnosis and intervention are critical to maximizing potential and improving quality of life.
Examples & Mechanisms:
- Autism Spectrum Disorder (ASD):
- Characterized by differences in social communication (e.g., eye contact, reciprocity) and restricted/repetitive behaviors (e.g., stimming, rigid routines).
- Linked to overconnectivity in local brain networks (e.g., default mode network) and underconnectivity between distant regions.
- Subtypes: Level 1 (requiring support) to Level 3 (requiring very substantial support).
- ADHD (Attention-Deficit/Hyperactivity Disorder):
- Involves dysregulation of dopamine and norepinephrine pathways, impairing attention, impulse control, and executive functioning.
- Subtypes: Predominantly inattentive, hyperactive-impulsive, or combined.
Symptoms:
- ASD: Sensory sensitivities, delayed speech, difficulty understanding social cues.
- ADHD: Forgetfulness, fidgeting, poor time management.
- Common Comorbidities: Anxiety (50% of ASD cases), learning disabilities (30% of ADHD cases).
Prevalence:
- ASD: 1 in 36 U.S. children (CDC, 2023), with a 4:1 male-to-female ratio.
- ADHD: 9.8% of U.S. children (6 million), 60% of whom experience symptoms into adulthood.
DSM-5 Criteria:
- ADHD: Symptoms (e.g., inattention, hyperactivity) must emerge before age 12 and persist ≥6 months across multiple settings (home, school).
- ASD: Symptoms must be present in early childhood, even if masked until social demands exceed capacity.

Treatment:
- Behavioral: Applied Behavior Analysis (ABA) for ASD; Parent-Child Interaction Therapy (PCIT) for ADHD.
- Pharmacological: Stimulants (e.g., methylphenidate) for ADHD; SSRIs for comorbid anxiety in ASD.
- Supportive: Individualized Education Programs (IEPs), occupational therapy.
Expert Insight:
“Neurodiversity isn’t a defect—it’s a different wiring. Our goal isn’t to ‘fix’ but to empower individuals with tools to thrive.” — Dr. Temple Grandin, Autism Advocate
9. Obsessive-Compulsive and Related Disorders
Obsessive-Compulsive and Related Disorders (OCRDs) are mental health conditions defined by persistent, intrusive thoughts (obsessions) and ritualistic behaviors (compulsions) performed to neutralize anxiety. These disorders stem from dysfunctional brain circuits, particularly in the cortico-striato-thalamo-cortical (CSTC) loop, which governs decision-making and threat detection. Sufferers often recognize their thoughts/behaviors as irrational but feel powerless to stop them, leading to significant time loss and distress.
Mechanism
- Neurobiology: Hyperactivity in the orbitofrontal cortex (obsessions) and basal ganglia (compulsions) creates a loop of anxiety and relief. Low serotonin levels exacerbate symptoms.
- Genetic Factors: 25–40% heritability, with first-degree relatives at higher risk.
Symptoms
- Obsessions: Fear of harm, contamination, or moral guilt.
- Compulsions: Repetitive handwashing, checking locks, mental rituals (e.g., counting).
- Avoidance: Evading triggers (e.g., public restrooms, sharp objects).
Examples
- Obsessive-Compulsive Disorder (OCD):
- Subtypes: Contamination, harm, symmetry, taboo thoughts (e.g., sexual/religious obsessions).
- Prevalence: 1.2% of U.S. adults; 50% onset before age 18.
- Hoarding Disorder:
- Persistent difficulty discarding items, leading to unsafe clutter.
- Prevalence: 2–6% of adults; often comorbid with ADHD.
- Body Dysmorphic Disorder (BDD):
- Preoccupation with perceived flaws (e.g., facial features), leading to excessive grooming or surgeries.
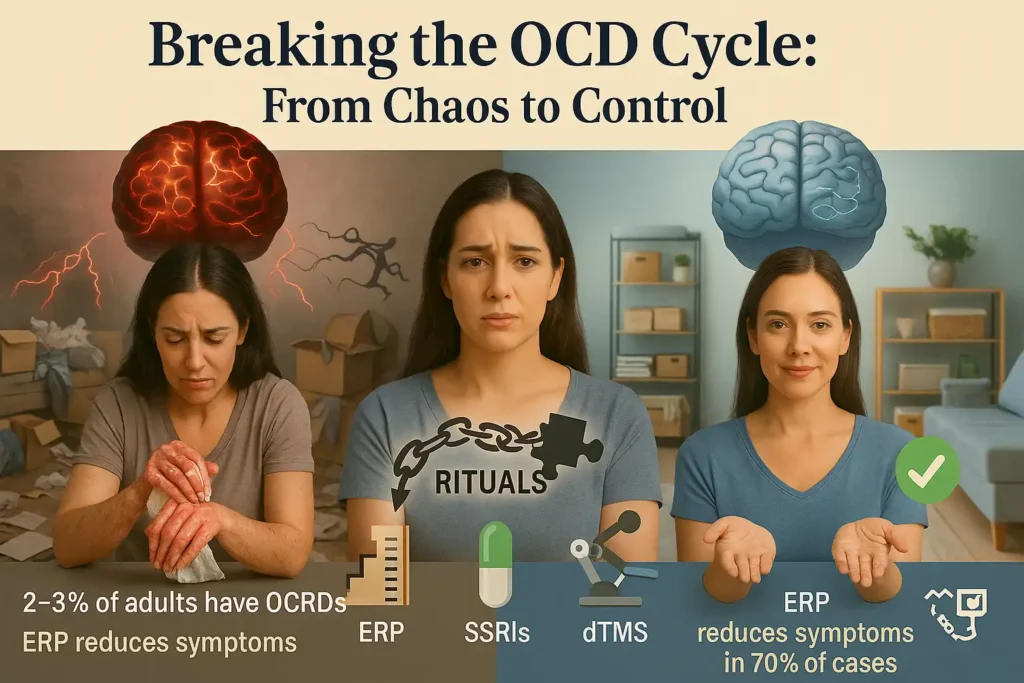
DSM-5 Criteria
- Obsessions/compulsions consume ≥1 hour/day and impair functioning.
- Hoarding disorder requires distress or danger from clutter.
Treatment
- First-Line: Exposure and Response Prevention (ERP) therapy to break the anxiety-compulsion cycle.
- Medications: SSRIs (e.g., fluoxetine) at higher doses than for depression.
- Innovative: Deep Transcranial Magnetic Stimulation (dTMS) for refractory cases.
Expert Insight:
“OCD is a ‘doubting disease.’ ERP teaches patients to tolerate uncertainty without rituals—it’s grueling but life-changing.” — Dr. Jonathan Abramowitz, OCD Researcher
10. Personality Disorders
Personality disorders are enduring, inflexible patterns of thinking, feeling, and behaving that deviate sharply from cultural norms, causing distress and impairing relationships. These disorders stem from maladaptive coping mechanisms developed in response to childhood trauma, neglect, or invalidating environments. Unlike episodic mental illnesses, personality disorders are deeply ingrained, emerging in adolescence/early adulthood and persisting lifelong without intervention.
Mechanism
- Neurobiology: Dysregulation in the amygdala (emotional processing) and prefrontal cortex (impulse control) underpins traits like impulsivity (BPD) or lack of empathy (NPD).
- Attachment Theory: Insecure attachment styles (e.g., fearful-avoidant in BPD) perpetuate unstable relationships.
- Genetic Factors: Heritability estimates range from 40–60% for Cluster B disorders.
Symptoms
- Cognitive: Black-and-white thinking (BPD), grandiose fantasies (NPD).
- Emotional: Intense mood swings (BPD), shallow affect (ASPD).
- Behavioral: Self-harm (BPD), exploitation of others (NPD).
Examples
- Borderline Personality Disorder (BPD):
- Core Traits: Fear of abandonment, identity disturbance, chronic emptiness.
- Prevalence: 1.6% of U.S. adults; 75% are female.
- *DSM-5*: ≥5 of 9 criteria (e.g., suicidal gestures, unstable relationships).
- Narcissistic Personality Disorder (NPD):
- Core Traits: Grandiosity, need for admiration, lack of empathy.
- Prevalence: 0.5–5% of adults; often comorbid with substance abuse.
- Antisocial Personality Disorder (ASPD):
- Core Traits: Disregard for others’ rights, deceitfulness, lack of remorse.
- Prevalence: 1–4% of adults; 3:1 male-to-female ratio.

DSM-5 Criteria
- General Criteria:
- Onset by early adulthood.
- Pervasive across personal/social contexts.
- Not attributable to other mental or medical conditions.
- Cluster System:
- Cluster A (Odd/Eccentric): Paranoid, schizoid, schizotypal.
- Cluster B (Dramatic/Erratic): BPD, NPD, ASPD, histrionic.
- Cluster C (Anxious/Fearful): Avoidant, dependent, obsessive-compulsive.
Treatment
- Dialectical Behavior Therapy (DBT): Gold standard for BPD (reduces self-harm by 50%).
- Mentalization-Based Therapy (MBT): Enhances ability to understand self/others.
- Medications: Mood stabilizers (BPD), SSRIs (comorbid depression).
Expert Insight:
“Personality disorders are survival strategies gone awry. Healing requires rebuilding trust—in oneself and others.” — Dr. Marsha Linehan, Creator of DBT
11. Schizophrenia Spectrum and Psychotic Disorders
Schizophrenia spectrum and psychotic disorders are severe mental health conditions marked by a profound detachment from reality, including hallucinations, delusions, and disorganized thinking. These disorders arise from complex interactions between genetic vulnerability (e.g., mutations in the COMT gene), neurodevelopmental abnormalities (e.g., enlarged ventricles), and environmental triggers (e.g., childhood trauma, cannabis use). Symptoms typically emerge in late adolescence/early adulthood, disrupting education, relationships, and independence.
Mechanism
- Dopamine Hypothesis: Hyperactivity in mesolimbic dopamine pathways drives positive symptoms (hallucinations), while hypoactivity in mesocortical pathways contributes to negative symptoms (apathy).
- Brain Structure: Reduced gray matter in the prefrontal cortex (executive dysfunction) and hippocampus (memory deficits).
- Neuroinflammation: Elevated cytokines (e.g., IL-6) may worsen cognitive decline.
Symptoms
- Positive Symptoms:
- Hallucinations: Auditory (e.g., commanding voices), visual, or tactile.
- Delusions: Persecutory (e.g., “The FBI is tracking me”), grandiose, or referential (e.g., believing TV messages are personal).
- Disorganized Speech: Tangentiality, word salad.
- Negative Symptoms:
- Avolition: Lack of motivation.
- Blunted Affect: Reduced emotional expression.
- Alogia: Poverty of speech.
- Cognitive Symptoms: Impaired working memory, attention deficits.
Examples
- Schizophrenia:
- Requires ≥2 symptoms (e.g., delusions + disorganized speech) for ≥6 months.
- Subtypes: Paranoid (persecutory delusions), catatonic (motor immobility).
- Prevalence: 0.3–0.7% of the U.S. population.
- Schizoaffective Disorder:
- Combines psychotic symptoms with mood episodes (mania/depression).
- Prevalence: 0.3% of adults.
- Brief Psychotic Disorder:
- Sudden psychosis lasting 1 day–1 month, often triggered by stress.

DSM-5 Criteria
- Schizophrenia:
- Active-phase symptoms (delusions, hallucinations, disorganized speech) ≥1 month.
- Continuous signs ≥6 months with functional decline.
- Exclusion of substance/medical causes.
- Schizophreniform Disorder: Meets schizophrenia criteria but lasts 1–6 months.
Treatment
- Antipsychotics:
- First-Generation: Haloperidol (risk of tardive dyskinesia).
- Second-Generation: Aripiprazole, clozapine (for treatment-resistant cases).
- Psychosocial Interventions:
- Cognitive Behavioral Therapy for Psychosis (CBTp): Challenges delusional beliefs.
- Supported Employment/Education: Rebuilds life skills.
- Early Intervention: Reduces relapse risk by 50% with coordinated specialty care.
Expert Insight:
“Psychosis is a brain condition, not a life sentence. With the right support, many achieve recovery—working, loving, and thriving.” — Dr. Patrick McGorry, Early Psychosis Researcher
12. Sleep-Wake Disorders
Sleep-wake disorders are disruptions in the quality, timing, or duration of sleep, leading to daytime impairment and reduced quality of life. These disorders arise from dysregulation of the circadian rhythm, neurotransmitter imbalances (e.g., hypocretin deficiency in narcolepsy), or maladaptive behaviors (e.g., excessive screen time). Chronic sleep disturbances are linked to cardiovascular disease, depression, and cognitive decline, making early diagnosis critical.
Mechanism
- Circadian Rhythm: Governed by the suprachiasmatic nucleus, disruptions (e.g., shift work, jet lag) misalign sleep-wake cycles with environmental cues.
- Neurotransmitters: Low GABA (insomnia) or hypocretin (narcolepsy) destabilize sleep architecture.
- Behavioral Factors: Poor sleep hygiene (e.g., irregular bedtime, caffeine use) perpetuates dysfunction.
Symptoms
- Insomnia: Difficulty falling/staying asleep, non-restorative sleep.
- Narcolepsy: Sudden sleep attacks, cataplexy (muscle weakness triggered by emotions).
- Restless Legs Syndrome (RLS): Urge to move legs, worsening at night.
Examples
- Insomnia Disorder:
- Acute: Lasts <3 months (e.g., stress-induced).
- Chronic: ≥3 nights/week for ≥3 months.
- Prevalence: 30% of adults globally; 10% meet chronic criteria.
- Narcolepsy Type 1:
- Hypocretin deficiency + cataplexy.
- Prevalence: 1 in 2,000 people.
- Obstructive Sleep Apnea (OSA):
- Repeated breathing pauses during sleep.
- Prevalence: 25% of men, 10% of women.

DSM-5 Criteria
- Insomnia: Dissatisfaction with sleep quantity/quality + daytime impairment for ≥3 months.
- Narcolepsy: Daily irrepressible sleep attacks + hypocretin deficiency (Type 1) or abnormal MSLT (Multiple Sleep Latency Test).
Treatment
- Behavioral:
- CBT-I (Cognitive Behavioral Therapy for Insomnia): Reduces sleep latency by 50%.
- Sleep restriction therapy (limit time in bed to consolidate sleep).
- Medical:
- Melatonin agonists (e.g., ramelteon) for circadian rhythm disorders.
- Sodium oxybate (Xyrem) for narcolepsy.
- Lifestyle: Light therapy (for shift workers), weighted blankets (RLS).
Expert Insight:
“Sleep is the foundation of mental health. Treating insomnia isn’t just about pills—it’s about rewiring habits.” — Dr. Matthew Walker, Sleep Scientist
13. Substance-Related and Addictive Disorders
Substance-related and addictive disorders are chronic, relapsing conditions characterized by compulsive substance use despite severe physical, psychological, and social consequences. These disorders hijack the brain’s reward system, with substances like alcohol, opioids, or stimulants flooding neural pathways with dopamine, reinforcing addictive behaviors. Genetic predisposition (50–60% heritability), trauma, and social determinants (e.g., poverty, lack of access to care) drive vulnerability.
Mechanism
- Neurobiology: Repeated substance use dysregulates the mesolimbic dopamine pathway, blunting natural rewards (e.g., food, relationships). Glutamate imbalances impair prefrontal cortex function, reducing impulse control.
- Tolerance/Withdrawal: Chronic use downregulates neurotransmitter receptors (e.g., GABA in alcohol dependence), necessitating higher doses to avoid withdrawal (e.g., tremors, seizures).
- Epigenetics: Trauma alters gene expression (e.g., FKBP5), increasing stress-related relapse risk.
Symptoms
- Behavioral: Failed attempts to quit, neglecting responsibilities, risky use (e.g., driving under influence).
- Physical: Cravings, withdrawal symptoms (e.g., nausea, sweating), tolerance.
- Psychological: Preoccupation with obtaining/using substances, denial of severity.
Examples
- Alcohol Use Disorder (AUD):
- Subtypes: Chronic (daily drinking), binge (≥5 drinks/occasion).
- Prevalence: 14.5 million U.S. adults (NIAAA, 2021).
- *DSM-5*: ≥2 symptoms (e.g., cravings, withdrawal) in 12 months.
- Opioid Use Disorder (OUD):
- Includes prescription painkillers (e.g., oxycodone) and heroin.
- Prevalence: 2.7 million U.S. adults; 130+ daily overdose deaths (CDC).
- Stimulant Use Disorder:
- Cocaine, methamphetamine; linked to cardiovascular damage and psychosis.

DSM-5 Criteria
- Mild: 2–3 symptoms.
- Moderate: 4–5 symptoms.
- Severe: ≥6 symptoms.
- Key Symptoms: Tolerance, withdrawal, time spent obtaining/using, continued use despite harm.
Treatment
- Medications:
- OUD: Buprenorphine, methadone (reduce cravings/withdrawal).
- AUD: Naltrexone, acamprosate.
- Behavioral:
- Motivational Interviewing (MI): Enhances readiness to change.
- Contingency Management: Rewards drug-free urine tests.
- Harm Reduction:
- Needle exchanges, naloxone distribution.
Expert Insight:
“Addiction isn’t a moral failing—it’s a treatable brain disease. Recovery requires addressing both biology and trauma.” — Dr. Nora Volkow, Director of NIDA
14. Trauma- and Stressor-Related Disorders
Trauma- and stressor-related disorders are mental health conditions triggered by exposure to overwhelmingly distressing events, such as violence, abuse, accidents, or significant life changes. These disorders reflect the brain’s struggle to process and adapt to extreme stress, often disrupting emotional regulation, memory integration, and interpersonal relationships.
Mechanism
- Neurobiology: Trauma dysregulates the hypothalamic-pituitary-adrenal (HPA) axis, leading to chronic cortisol elevation. This impairs the prefrontal cortex (decision-making) and hyperactivates the amygdala (fear response), trapping individuals in a survival state.
- Memory Fragmentation: Traumatic memories often remain unprocessed in the brain’s right hemisphere, manifesting as flashbacks or nightmares.
Examples
- Post-Traumatic Stress Disorder (PTSD):
- Symptoms: Intrusive memories, avoidance of triggers, hypervigilance, negative mood changes.
- Prevalence: 7% of U.S. adults; 20% of combat veterans.
- *DSM-5 Criteria*: Symptoms persist >1 month with functional impairment.
- Adjustment Disorder:
- Symptoms: Emotional/behavioral reactions (e.g., anxiety, reckless behavior) within 3 months of a stressor (e.g., divorce, job loss).
- Prevalence: 5–20% in clinical settings; often resolves within 6 months post-stressor.
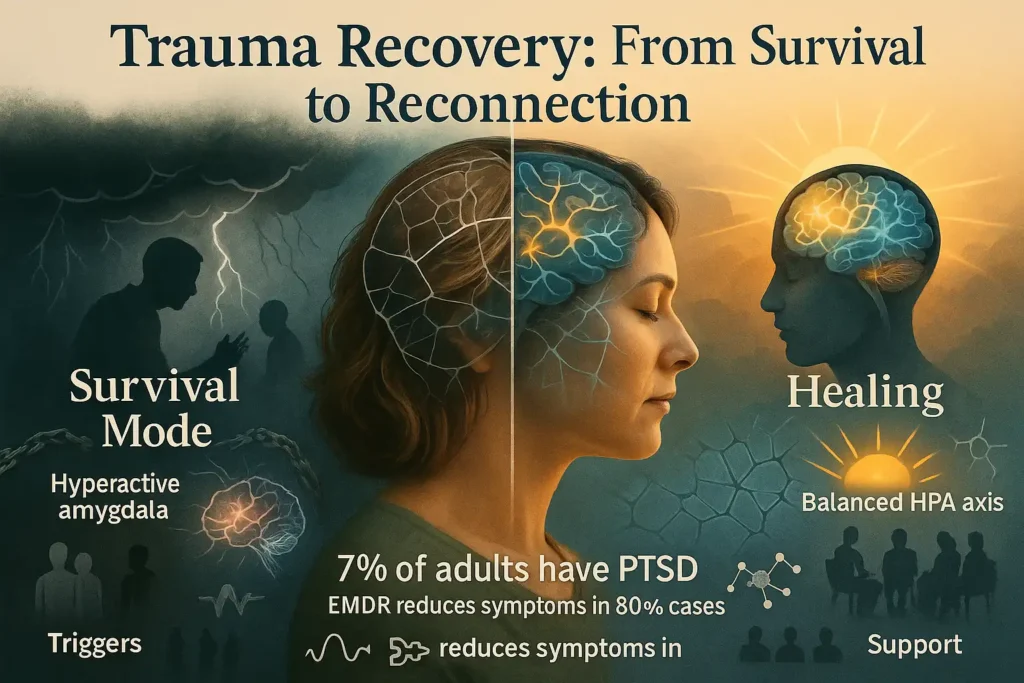
Risk Factors
- Cumulative trauma (e.g., childhood adversity + adult trauma).
- Lack of social support or coping skills.
Treatment
- Trauma-Focused Therapies:
- EMDR (Eye Movement Desensitization and Reprocessing): Helps reprocess traumatic memories.
- CPT (Cognitive Processing Therapy): Challenges distorted beliefs (e.g., self-blame).
- Medications: SSRIs (e.g., sertraline) for PTSD.
- Mindfulness: Reduces hyperarousal through grounding techniques.
Expert Insight:
“Trauma isn’t what happens to you—it’s what happens inside you. Healing requires rebuilding safety in the body and mind.” — Dr. Bessel van der Kolk, Trauma Expert
Diagnosis and Comorbidity
The DSM-5 provides standardized criteria to diagnose mental illnesses. For example, diagnosing major depressive disorder requires ≥5 symptoms (e.g., low mood, sleep changes) lasting ≥2 weeks.
Comorbidity:
- Dual Diagnosis: 50% of individuals with mental illness have a co-occurring substance use disorder.
- Example: A person with borderline personality disorder may also struggle with major depression and alcohol misuse.
Treatment Options
Psychotherapy
- Cognitive Behavioral Therapy (CBT): Challenges negative thought patterns.
- Dialectical Behavior Therapy (DBT): Teaches emotional regulation.
Medications
| Class | Examples | Used For |
|---|---|---|
| SSRIs | Prozac, Zoloft | Depression, anxiety |
| Antipsychotics | Risperdal, Abilify | Schizophrenia, bipolar |
| Mood Stabilizers | Lithium | Bipolar disorder |
Procedures
- Electroconvulsive Therapy (ECT): Effective for treatment-resistant depression.
Lifestyle Adjustments
- Exercise: 30 minutes/day reduces anxiety and depression.
- Mindfulness: Meditation apps like Headspace improve emotional resilience.
Conclusion
Mental illnesses are diverse but treatable. Early diagnosis using DSM-5 criteria and evidence-based treatments like CBT or SSRIs can significantly improve quality of life. If you or a loved one are struggling, contact the 988 Suicide & Crisis Lifeline for immediate support.
Key Takeaways:
- Mental illnesses affect 1 in 5 adults.
- Treatment combines therapy, medication, and lifestyle changes.
- Comorbidity is common; integrated care is essential.
Sources:

