Cervical cancer, which targets the cervix (the resilient gateway between the vagina and uterus), stands apart in the world of oncology: it’s one of the few cancers we can nearly eradicate. Yet, despite medical advances, over 4,000 women in the U.S. still lose their lives to this disease each year—a tragedy compounded by the fact that 93% of cases are preventable through vaccination and screening.
The American Cancer Society reports roughly 13,170 new diagnoses annually, but behind this statistic lies a powerful truth: when caught early (Stage 0–1), cervical cancer has a 93% survival rate. Its progression—from HPV infection to precancerous cells to invasive cancer—unfolds over 10–15 years, offering a critical window for intervention.
Understanding cervical cancer’s stages isn’t just about medical terminology; it’s about grasping the life-altering difference between a routine Pap smear and a Stage 4 diagnosis. Staging dictates whether treatment means a 30-minute outpatient procedure or a years-long battle with chemotherapy. For caregivers and patients alike, this knowledge transforms fear into agency—because cervical cancer’s greatest weakness is timing.
Why this matters now:
- The HPV vaccine, introduced in 2006, has already slashed cervical cancer rates by 65% in young women (CDC).
- Yet, 51% of women remain under-screened, often due to gaps in healthcare access or awareness.
This guide isn’t just about cancer—it’s about rewriting futures. By demystifying stages, symptoms, and survival data, we empower individuals to seize control through prevention, advocate for their health, and challenge a disease that thrives on silence.
“Cervical cancer is a mirror reflecting healthcare inequities—but also our power to shatter them.” — World Health Organization
Symptoms & Early Detection
Cervical cancer is often called a “silent” disease in its earliest phases, as most women experience no symptoms until the cancer advances. This makes proactive screening critical. Below, we break down what to watch for—and how early detection can be lifesaving.

Recognizing the Warning Signs
As cervical cancer progresses, symptoms may include:
- Abnormal Vaginal Bleeding
- Bleeding between periods, after sexual intercourse, or after menopause.
- Heavier or longer menstrual cycles than usual.
- Pelvic Pain or Discomfort
- Persistent pain in the pelvis or lower back.
- Pain during intercourse (dyspareunia), which may feel sharp or deep.
- Unusual Vaginal Discharge
- Foul-smelling discharge that may appear watery, pink, or streaked with blood.
- A sudden change in discharge consistency or odor.
Important: These symptoms can mimic less serious conditions (e.g., infections, fibroids). Never dismiss persistent changes—consult a healthcare provider for evaluation.
Why Early Detection Matters
Cervical cancer is one of the most preventable cancers, but timing is everything. Here’s how to catch it early:
1. Pap Smear (Pap Test)
- What it does: Screens for precancerous cell changes in the cervix.
- Why it’s vital: Detects abnormalities years before they turn cancerous.
- Guidelines: The American Cancer Society (ACS) recommends:
- Start Pap tests at age 25.
- If results are normal, repeat every 3–5 years (combined with HPV testing).
2. HPV DNA Testing
- What it does: Identifies high-risk HPV strains (e.g., HPV 16, 18) linked to 95% of cervical cancers (WHO).
- Why it’s vital: HPV often clears on its own, but persistent infection can trigger cancer.
- Guidelines:
- Women aged 25–65 should get an HPV test every 5 years (preferred method: co-testing with a Pap).
- Over 65? Screening may stop if prior results are normal.
The Lifesaving Power of Screening
- Regular Pap + HPV testing can prevent up to 80% of cervical cancers.
- Women who skip screenings are 6x more likely to be diagnosed with advanced-stage cancer.
Real-life impact: A 2023 study found that 93% of Stage 0–1 cervical cancer cases are cured with early treatment.
Key Takeaway
Trust your body, trust the science:
- If you notice any symptoms, act immediately—don’t “wait and see.”
- Even if you feel healthy, stick to screening schedules. Early-stage cervical cancer often has no warning signs.
*”A 10-minute Pap test could save decades of your life.”*
Cervical Cancer Stages (0–4)
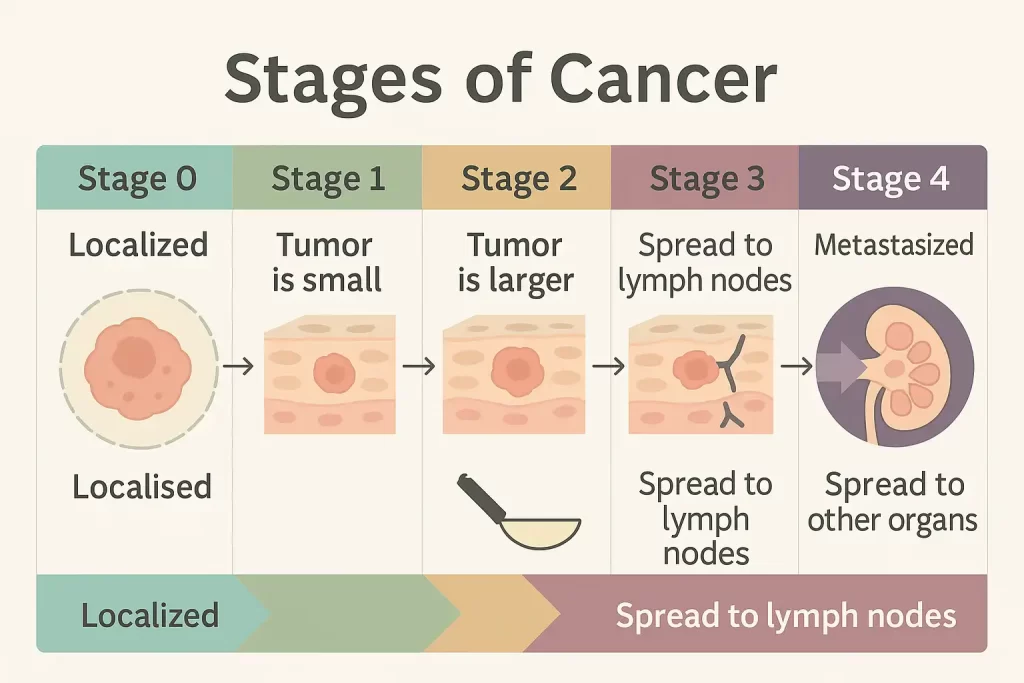
Staging cervical cancer is critical for determining treatment plans and predicting outcomes. The FIGO system (International Federation of Gynecology and Obstetrics) categorizes cervical cancer into five stages (0–4), reflecting tumor size, spread, and impact on nearby organs. Below, we break down each stage with clinical details and survival data:
Cervical Cancer Staging Table
| Stage | Key Characteristics | 5-Year Survival Rate | Common Treatment Options |
|---|---|---|---|
| Stage 0 | Carcinoma in situ: Abnormal cells only on the cervix’s surface (precancerous). | Nearly 100%* | – LEEP (Loop Electrosurgical Excision) – Cone biopsy – Cryotherapy |
| Stage 1 | Cancer is confined to the cervix. – 1A: Microscopic invasion (<3–5 mm deep). – 1B: Visible tumor (up to 4 cm). | 93% (1A) 80% (1B) | – Radical hysterectomy – Radiation + Chemotherapy |
| Stage 2 | Spread to upper vagina/uterus but not pelvic wall. – 2A: No parametrial invasion. – 2B: Invades parametrial tissue. | 63% (2A) 58% (2B) | – Chemoradiation – Surgery (select cases) |
| Stage 3 | Extends to pelvic wall/lower vagina or causes kidney issues (hydronephrosis). – 3A: Lower vagina affected. – 3B: Pelvic wall/kidney involvement. | 35% (3A) 32% (3B) | – Aggressive chemoradiation – Palliative surgery |
| Stage 4 | Metastasized to distant organs (bladder, rectum, lungs, liver). – 4A: Invades bladder/rectum. – 4B: Distant organ spread. | 15–16% | – Palliative care – Targeted therapy – Immunotherapy (clinical trials) |
Source: American Cancer Society (2023 data)
Note: Survival rates are averages; individual outcomes depend on age, health, and treatment access.
Key Takeaways
- Stage 0–1: Highly treatable with surgery or localized therapy. Survival exceeds 80% with early intervention.
- Stage 2–3: Requires combination therapies (chemoradiation) to target regional spread.
- Stage 4: Focus shifts to quality of life and symptom management, though emerging therapies offer hope.
Why Staging Matters
- Guides Treatment: Early stages (0–1) often avoid chemotherapy, while advanced stages (3–4) prioritize systemic therapies.
- Predicts Outcomes: Survival rates highlight the life-saving power of early detection.
- Informs Clinical Trials: Advanced stages may benefit from experimental treatments.
Source: American Cancer Society
How Is Cervical Cancer Diagnosed?
Diagnosing cervical cancer involves a combination of screenings, imaging, and lab tests to detect abnormalities, confirm cancer, and determine its spread. Below, we break down the 5 essential diagnostic methods, their purpose, and what to expect:
1. Pap Smear (Pap Test)
What it does:
- Screens for precancerous or abnormal cells on the cervix.
- Identifies cell changes caused by HPV before they turn cancerous.
How it works:
- A speculum is inserted into the vagina to access the cervix.
- Cells are gently scraped from the cervix and analyzed under a microscope.
Why it matters:
- Reduces cervical cancer deaths by 80% through early detection (ACS).
- Recommended every 3–5 years for women aged 25–65 (with HPV co-testing).
2. HPV DNA Test
What it does:
- Detects high-risk HPV strains (e.g., HPV 16, 18) linked to 95% of cervical cancers.
How it works:
- Uses the same cell sample from a Pap smear.
- Tests for HPV genetic material to assess cancer risk.
Why it matters:
- Identifies persistent HPV infections needing closer monitoring.
- The CDC recommends HPV testing every 5 years starting at age 25.
3. Colposcopy
What it does:
- A magnified exam of the cervix to pinpoint abnormal areas.
How it works:
- A vinegar-like solution is applied to the cervix, highlighting irregularities.
- A colposcope (lighted magnifying device) examines the cervix for lesions.
Next steps:
- If suspicious areas are found, a biopsy is taken during the procedure.
Why it matters:
- Guides targeted biopsies, reducing guesswork and improving accuracy.
4. Biopsy
Types of biopsies:
- Punch biopsy: Removes a small tissue sample from abnormal areas.
- Cone biopsy (LEEP/Conization): Removes a cone-shaped tissue section for deeper analysis.
How it works:
- Tissue is sent to a lab to confirm cancer presence, type (e.g., squamous cell carcinoma), and grade.
Why it matters:
- The only definitive way to diagnose cervical cancer.
5. Imaging Scans (MRI, CT, PET)
What they do:
- MRI: Detailed images of cervix, pelvis, and lymph nodes to assess tumor size/spread.
- CT/PET scans: Detect metastasis to distant organs (lungs, liver).
When used:
- After a cancer diagnosis to determine stage (e.g., Stage 3 vs. 4).
Why it matters:
- Critical for creating a tailored treatment plan (surgery vs. radiation).
Diagnostic Pathway Flowchart
- Abnormal Pap/HPV test → 2. Colposcopy → 3. Biopsy → 4. Imaging → 5. Final Diagnosis & Staging
Key Takeaway
Early diagnosis hinges on routine screenings (Pap + HPV tests). If abnormalities are found, advanced tests like colposcopy and imaging ensure precise staging and treatment. “Don’t skip your Pap smear—it’s the first line of defense against cervical cancer.”
Survival Rates & Prognosis
Cervical cancer survival rates provide a statistical snapshot of outcomes, but every patient’s journey is unique. Prognosis hinges on the stage at diagnosis, treatment accessibility, and individual health factors. Below, we break down survival data, contextualize the numbers, and highlight advances in care.
5-Year Survival Rates by Stage
The 5-year survival rate reflects the percentage of patients alive five years post-diagnosis. These averages, sourced from the American Cancer Society (2023), are benchmarks—not definitive predictions:
| Stage | Key Details | 5-Year Survival Rate |
|---|---|---|
| Stage 0 | Precancerous cells (carcinoma in situ). | Nearly 100% |
| Stage 1 | Cancer confined to the cervix. | 80–93% |
| Stage 2 | Spread to upper vagina/uterus. | 58–63% |
| Stage 3 | Reaches pelvic wall/lower vagina; may block kidneys. | 32–35% |
| Stage 4 | Metastasized to distant organs (e.g., lungs, liver). | 15–16% |
What Influences Survival Rates?
While staging is critical, these factors also shape outcomes:
- Age & Overall Health: Younger patients with strong immune systems often tolerate aggressive treatments better.
- HPV Status: HPV-positive cancers may respond better to therapies than HPV-negative ones.
- Access to Care: Timely surgery, radiation, and targeted therapies improve survival.
- Tumor Biology: Aggressive subtypes (e.g., small cell carcinoma) have poorer prognoses.
- Treatment Response: Some tumors shrink rapidly with chemoradiation; others resist therapy.
Stage-Specific Insights
- Stage 0–1: Highly curable. Surgery (cone biopsy/hysterectomy) or radiation often leads to remission.
- Stage 2–3: Treatable but challenging. Chemoradiation combined with surgery can extend survival, but recurrence risks rise.
- Stage 4: Focus shifts to quality of life. Palliative care manages pain, while immunotherapy trials (e.g., pembrolizumab) offer hope for some.
Beyond the Numbers: Reasons for Hope
- Immunotherapy: Drugs like Keytruda (pembrolizumab) target advanced cervical cancer with PD-L1 markers, doubling survival in some trials.
- HPV Vaccination: Widespread vaccination could reduce cervical cancer cases by 90% in decades (WHO).
- Personalized Medicine: Genetic testing identifies mutations (e.g., PI3K) for tailored therapies.
Key Takeaway
Survival statistics are a starting point—not a verdict. Advances in early detection (e.g., HPV self-tests) and treatment are steadily improving outcomes. For those facing advanced stages, palliative care and clinical trials can extend life and ease symptoms.
“Your diagnosis is a chapter, not the whole story. Advocate for screenings, explore all options, and lean on support networks.”
Prevention: Your Best Defense
Cervical cancer is not a fate—it’s a preventable outcome. With the right tools, you can slash your risk by over 90%. Below, we dismantle the three pillars of prevention, backed by science and steeped in actionable steps.
1. HPV Vaccination: Armor Against the Invisible Threat
What it does:
- The HPV vaccine blocks 9 high-risk strains of human papillomavirus (HPV 16, 18, 31, 33, 45, 52, 58, and others), which cause 90% of cervical cancers (CDC).
- It also prevents genital warts and cancers of the throat, anus, and vulva.
Who needs it:
- Ages 9–26: Ideal time for vaccination (pre-sexual activity).
- Ages 27–45: The CDC now recommends catch-up doses for unvaccinated adults.
Why it’s revolutionary:
- Since its 2006 debut, the vaccine has reduced HPV-related cancers by 65% in teens and young adults.
- Myth-buster: “I’m already sexually active—is it too late?” No. The vaccine still protects against strains you haven’t encountered.
Key stat: Countries with 90% HPV vaccination rates (e.g., Australia) are on track to eliminate cervical cancer by 2035.
2. Routine Screenings: Catching Cancer Before It Starts
The 1-2 Punch:
- Pap Smear: Detects precancerous cell changes.
- HPV Test: Identifies high-risk HPV strains.
Guidelines:
- 25–65 years: Co-testing (Pap + HPV) every 5 years is gold standard.
- Post-65: Stop if prior results are normal (but discuss with your doctor).
Why it’s non-negotiable:
- Precancerous cells take 10–15 years to turn invasive. Screenings intercept this process early, when treatment is simplest.
- Tragic irony: 50% of cervical cancer deaths occur in women who’ve never been screened.
3. Lifestyle Choices: Your Daily Defense Strategy
| Risk Factor | Action | Impact |
|---|---|---|
| Smoking | Quit today. | Smoking doubles risk by weakening cervical immunity and fueling DNA damage. |
| Sexual Health | Use condoms; limit partners. | Reduces HPV exposure. 6+ lifetime partners? Risk triples. |
| Diet/Immunity | Eat antioxidant-rich foods. | A strong immune system clears 90% of HPV infections naturally. |
The silent accelerator:
- Birth control pills: Long-term use (>5 years) may slightly raise risk. Balance benefits with screenings.
- Poverty & Access: Lack of healthcare doubles mortality. Advocate for free clinics and telehealth options.
Prevention at a Glance
| Tool | Best For | When to Act | Efficacy |
|---|---|---|---|
| HPV Vaccine | Stopping cancer before HPV | Ages 9–45 | 90% cancer prevention |
| Pap + HPV Tests | Catching precancer | Every 5 years (25–65) | 80% mortality reduction |
| Smoking Cessation | Halting cell damage | Immediately | 50% risk drop post-quitting |
Your Call to Action
- Today: Book your child’s HPV vaccine or your own catch-up dose.
- This Month: Schedule a Pap/HPV test if overdue.
- This Year: Swap one habit (e.g., vaping → walking) to boost immunity.
Remember: Cervical cancer preys on delay. Every year, 4,000+ women die from a disease we can outsmart. Will you be the generation that ends it?
FAQs
Q1: Can cervical cancer be cured if caught early?
A: Yes—early-stage cervical cancer is highly treatable, often curable.
- Stage 0 (precancer): Nearly 100% cure rate with minimally invasive procedures like LEEP or cryotherapy.
- Stage 1: Surgery (hysterectomy) or radiation achieves a 93% survival rate (American Cancer Society).
Why early action matters: Precancerous cells take 10–15 years to become invasive cancer. Regular screenings intercept this process, preventing progression.
Key Takeaway: “Cervical cancer is one of the few cancers we can stop before it starts. Don’t skip your Pap test.”
Q2: Do I need a Pap test if I’ve had the HPV vaccine?
A: Absolutely. Here’s why:
- The HPV vaccine protects against 9 high-risk strains, including HPV 16/18 (linked to 70% of cervical cancers).
- However, 30% of cervical cancers are caused by other HPV strains not covered by the vaccine.
- The vaccine is most effective when given before HPV exposure (ideally ages 9–12).
Guidelines:
- Vaccinated women: Start Pap + HPV co-testing at 25, per ACS.
- Unvaccinated women: Same screening schedule—plus ask about catch-up vaccines (available up to age 45).
Key Takeaway: Think of the HPV vaccine as a seatbelt and screenings as airbags—both save lives.
Q3: How often should I get screened if I’ve had abnormal results before?
A: It depends on your history:
- Minor cell changes: Repeat Pap/HPV test in 6–12 months.
- High-grade precancer (CIN2/3): Requires treatment (e.g., LEEP) followed by every 3–6 month screenings for 2 years.
- Post-treatment: Most women return to normal screening after 3 years of clear results.
Q4: Can I still get cervical cancer after a hysterectomy?
A: Risk is extremely low but not zero if:
- Your hysterectomy was for non-cancerous reasons (e.g., fibroids) and the cervix was removed.
- Exception: If surgery was for cervical precancer/cancer, ongoing vaginal vault screenings may be needed.
Q5: Are cervical cancer survivors at higher risk for other cancers?
A: Not directly, but:
Smoking history raises risks for lung/bladder cancers.
HPV can cause vaginal, vulvar, or anal cancers—regular pelvic exams are crucial.
Conclusion
Imagine holding a shield forged from knowledge—a shield that deflects fear and empowers you to rewrite the narrative of your health. Cervical cancer, a disease once shrouded in inevitability, now bows to the twin swords of prevention and early action. Here’s how you wield them:
- The HPV Vaccine: A 15-second injection that blocks 90% of cervical cancers (CDC). It’s not just a shot; it’s a legacy of health for future generations.
- Screenings: A 10-minute Pap test can mean the difference between a 93% survival rate (Stage 1) and a 16% survival rate (Stage 4). These numbers aren’t abstract—they represent birthdays celebrated, milestones reached, and lives uninterrupted.
- Symptom Vigilance: That “odd” discharge or unexplained bleeding? Your body whispers warnings long before it screams. Listen.
Yes, barriers exist—time, fear, or access to care. But consider this: 51% of cervical cancer deaths occur in underserved communities. By demanding equitable healthcare, advocating for free clinics, or simply texting a friend to book their screening, you become part of a revolution.
Today, right now, ask yourself: “When did I last prioritize my well-being?” If the answer unsettles you, let it ignite action. Call your doctor. Share this article. Challenge the stigma.
The World Health Organization envisions a world free of cervical cancer by 2030. That future starts in your calendar, in your choices, in your courage to act.
“The greatest tragedy of cervical cancer isn’t its existence—it’s that we have the tools to end it, yet hesitate to use them.”
“Cervical cancer is preventable. Let’s end it together.”