Let’s be honest: when you’re in your 20s or 30s, breast cancer probably isn’t at the top of your mind. You’re building a career, maybe starting a family, or just living your life. It’s easy to feel invincible, to think, “That’s something I’ll worry about later.”
But here’s the truth we need to talk about: breast cancer doesn’t care how old you are. While it’s more common in older women, thousands of women under 40 are diagnosed each year. For young women, the disease can be trickier to detect and often diagnosed at a later stage, making awareness absolutely critical.
This guide isn’t meant to scare you. It’s meant to empower you. Knowledge is power, and knowing what to look for is your first and best line of defense.
Why Breast Cancer is Different for Young Women
BWhen we think of breast cancer, we often picture it in the context of older women. But for women under 40, the reality of a diagnosis comes with a unique set of challenges that can make detection and treatment more complex. Understanding these differences is the first step to becoming your own best advocate.
1. The Challenge of Denser Breast Tissue
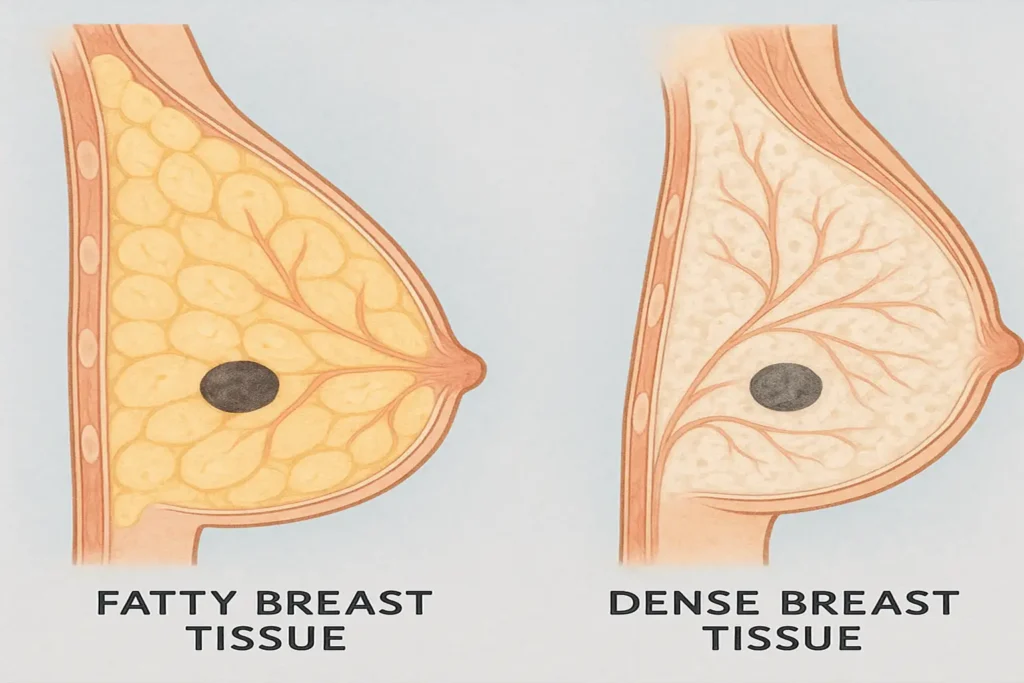
Younger women typically have denser breast tissue, which contains more glandular and fibrous tissue than fatty tissue. While this is completely normal, it creates a significant hurdle for detection.
- On a Mammogram: Dense tissue appears as a solid white area, and unfortunately, tumors also appear white. This is like trying to find a snowball in a snowstorm—it becomes incredibly difficult for radiologists to distinguish a potential tumor from the surrounding dense tissue. This is why mammograms can have a higher rate of “false negatives” in younger women, meaning the test misses a cancer that is actually present.
- During Self-Exams: This density can also make it harder to feel a distinct lump. Rather than a clearly defined pebble, a lump might feel more like a general thickening or area of firmness within the already dense landscape of the breast.
2. The Screening Gap
Because the overall risk is lower and dense tissue makes mammograms less effective, most major health organizations do not recommend routine screening mammograms for average-risk women under 40. This creates a critical “screening gap.” Without regular imaging, the responsibility for early detection falls heavily on you. This makes Breast Self-Awareness—knowing the normal look and feel of your own breasts—not just a recommendation, but an essential practice. It means that when you do notice a change, you must be your own champion and seek medical evaluation, even without a routine screening schedule.
3. Often More Aggressive Biologies
Perhaps the most sobering difference is the biology of breast cancers in younger women. They are more likely to be diagnosed with faster-growing and more aggressive sub-types, such as:
- Triple-Negative Breast Cancer (TNBC): This type lacks the three most common receptors (Estrogen, Progesterone, HER2) that many treatments target, making it more challenging to treat.
- HER2-Positive Breast Cancer: This type involves an overexpression of the HER2 protein, which can promote the growth of cancer cells. While treatments exist, it was historically considered a very aggressive cancer.
This is precisely why early detection is not just a buzzword; it’s a critical factor in improving outcomes. Finding and diagnosing the cancer at an earlier stage can significantly influence treatment success.
The Bottom Line: You Are the Expert on Your Own Body
In the face of these challenges, your most powerful tool is self-knowledge. You are the only person who lives in your body every single day. You are the first line of defense. This isn’t meant to be a burden, but a source of empowerment. By being aware of these unique factors and committing to knowing what is normal for you, you take control and become an active participant in your own health.
The 8 Early Signs You Should NEVER Ignore
Move beyond the single idea of a lump. Breast cancer can reveal itself in several ways. If you notice any of the following changes that are new and persistent (lasting for two weeks or more), it’s time to see a doctor.
1. A New Lump or Thickening
This is the most well-known sign, but it’s important to know the details. It may feel like a hard, painless knot with distinct edges. However, it can also be tender, soft, or rounded. The key is that it’s a new change. Check in the breast tissue and around the armpit area.
2. Change in Breast Size or Shape
Look for unexplained swelling or shrinkage, especially if it’s only on one side. A sudden difference in the size or contour of your breasts is a significant red flag.
3. Nipple Changes
Pay attention to your nipples. Be concerned if one nipple suddenly turns inward (inversion), retracts, or changes its position or direction. Any spontaneous change should be checked.

4. Nipple Discharge
While discharge can be related to hormonal shifts or medications, be wary of discharge that occurs without squeezing, is bloody, or comes from only one nipple.
5. Skin Changes on the Breast
This is a sign people often miss. Look for:
- Dimpling: Skin that looks pitted or dimpled, like an orange peel (called peau d’orange).
- Redness or Rash: Unexplained redness, warmth, or a rash that doesn’t go away.
- Scaling or Thickening: Skin on the breast or nipple that becomes scaly, red, or swollen.
6. Breast or Nipple Pain
While breast pain is extremely common and usually linked to your menstrual cycle, persistent pain in one specific spot that isn’t related to your cycle warrants a conversation with your doctor.
7. Itching or Rash on the Nipple
Persistent, intense itching or a rash on or around the nipple can be a symptom of a rare form of breast cancer called Paget’s disease.
8. Swelling or a Lump in the Armpit
Breast tissue extends into the armpit. A lump or swelling under your arm could be an enlarged lymph node, which can be an early sign that the body is fighting something, including breast cancer.
What’s Normal? Contextualizing the Signs
Reading a list of potential cancer symptoms can be understandably alarming. It’s crucial to pause and remember this fundamental truth: The vast majority of breast changes are not cancer. Your body is dynamic, and your breasts naturally change throughout your menstrual cycle and life.
Many of the signs we’ve discussed can be caused by completely benign (non-cancerous) conditions. Let’s break down what else might be happening:
- That “Lump” Could Be: A fluid-filled cyst (often smooth and movable) or a solid, benign fibroadenoma (a rubbery lump common in young women). Both are harmless and often easily managed.
- Pain and Tenderness: This is most often linked to your hormonal fluctuations during your menstrual cycle. This “cyclical” pain typically comes and goes with your period.
- Nipple Discharge: Discharge that appears only when the nipple is squeezed, is milky, or occurs from both breasts is frequently related to hormones, medications, or thyroid issues.
- Skin Redness and Swelling: This can often be a sign of a breast infection (mastitis), especially in women who are breastfeeding, or another skin condition like eczema.

The Key Takeaway: Don’t Panic, But Do Take Action
The goal of this information is not to make you live in fear of every twinge or change. The goal is to move you from a place of “I’m sure it’s nothing” to a place of “I should get this checked to be sure.”
Think of it this way: You wouldn’t ignore a persistent, unexplained check-engine light in your car. You’d take it to a mechanic to diagnose the problem, which could be anything from a serious issue to a simple, loose gas cap.
Your body is giving you a signal. Your doctor’s job is to be the mechanic—to run the tests and figure out the cause. It is always better to be safe and get a professional opinion. Making that appointment is an act of self-care and empowerment, not panic.
Beyond the Lumps: Lesser-Known Symptoms
SWhen we think of breast cancer, we focus on the breast. However, it’s vital to understand that cancer can sometimes announce itself through more general, “whole-body” symptoms. These are often the easiest to dismiss as stress, a busy lifestyle, or a different minor ailment. Paying attention to these systemic signals is a critical part of awareness, especially when they are persistent and unexplained.
Here’s a closer look at what these lesser-known symptoms might involve and why they occur:
- Unexplained, Persistent Fatigue: This isn’t the typical tiredness you feel after a long day or a poor night’s sleep. This is a deep, unshakable exhaustion that doesn’t improve with rest. The body uses a tremendous amount of energy to fight cancer, and cancer cells can also release substances that directly cause fatigue. If you’re consistently drained for no clear reason, it’s your body asking for a check-in.
- Unexplained Weight Loss: Losing a significant amount of weight (e.g., 10 pounds or more) without changes to your diet or exercise routine can be a red flag. Cancer can change the way your body uses energy from food, leading to unintended weight loss.
- Persistent Back or Bone Pain: While back pain is incredibly common, pain that is new, constant, and localized to one area—especially in the upper or middle back—can be a symptom of cancer that has spread (metastasized) to the bones. This type of pain may be dull and aching or sharp and stabbing, and it often doesn’t improve with typical remedies like stretching or pain relievers. It may also feel worse at night.
The Crucial Takeaway
It is essential to state that these symptoms are most often caused by conditions far less serious than cancer, such as thyroid issues, stress, or routine musculoskeletal problems.
However, when these general symptoms appear in conjunction with a specific breast change, or when they are persistent and have no other explanation, they are a powerful signal from your body to seek medical advice. You know your body’s normal baseline better than anyone. If something feels profoundly and persistently “off,” it is always a valid reason to consult your doctor.
Know Your Breasts: The Power of Self-Exams
Think of your monthly self-check not as a scary test, but as a familiar conversation with your own body. You are not looking for something wrong; you are learning what is normal for you. This practice, often called Breast Self-Awareness (BSA), is your most accessible and powerful tool for early detection. You don’t need to be a medical expert—you just need to be you.
How to Perform a Breast Self-Exam: A Step-by-Step Guide
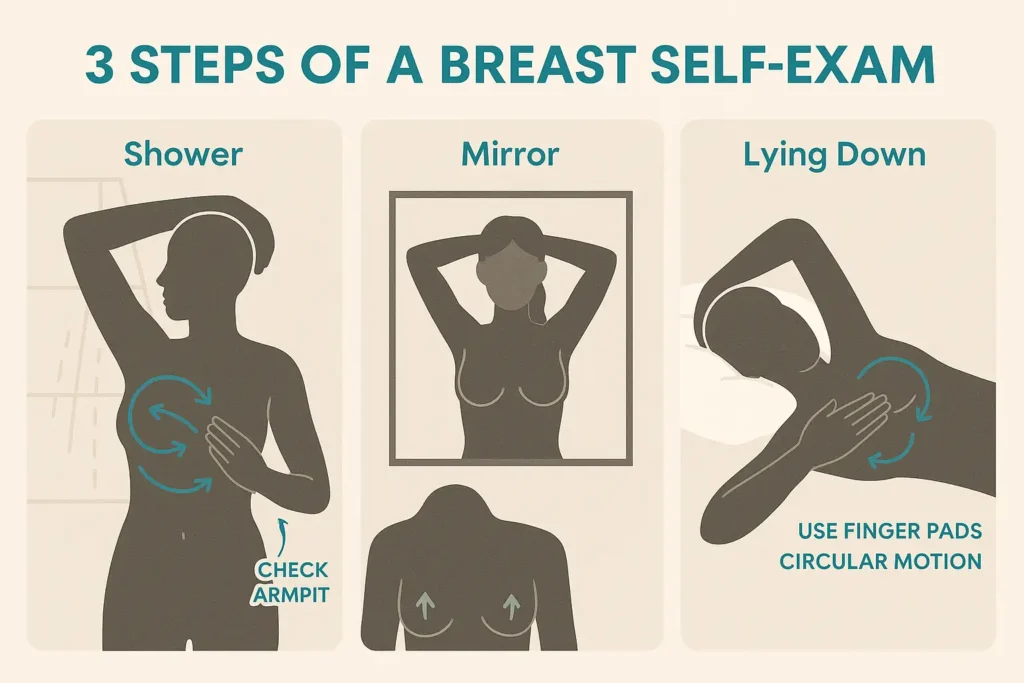
A thorough self-exam involves three key positions. The best time to do this is about 3-5 days after your period ends, when your breasts are least likely to be swollen or tender. If you no longer have a period, choose a consistent day each month, like the first day of the month.
Step 1: In the Shower
(Using water and soap helps your fingers glide smoothly over the skin.)
- Raise your right arm and place your hand behind your head.
- Using the pads of the three middle fingers on your left hand (not your fingertips), feel for any lumps or thickening in your right breast.
- Press with a firm, smooth touch in a circular pattern, about the size of a quarter. You can choose to move:
- In lines from your collarbone to the top of your abdomen, and from your armpit to your cleavage.
- In circles from the outside of your breast toward the nipple, covering the entire breast.
- Vary the pressure—use light pressure to feel the tissue close to the skin, medium pressure for deeper tissue, and firm pressure to feel the tissue closest to your chest and ribs.
- Repeat these steps on your left breast, using your right hand.
Step 2: In Front of a Mirror
(This is for a visual inspection to spot changes in appearance.)
- Stand undressed from the waist up in front of a well-lit mirror with your arms relaxed at your sides.
- Look closely at your breasts for any changes in:
- Size, shape, or contour.
- Skin: Dimpling, puckering, redness, rash, or bulging.
- Nipples: Any change in position, inversion (pulling inward), or redness.
- Now, place your hands on your hips and press firmly to flex your chest muscles. Turn from side to side to look for the same changes. (Note: It’s normal for breasts to not be perfectly symmetrical).
- Finally, raise your arms high overhead and look for the same changes again, as well as any swelling or dimpling of the skin.
Step 3: Lying Down
(When you lie down, your breast tissue spreads out evenly and thinly, making it easier to feel.)
- Lie down on your back and place a small pillow or folded towel under your right shoulder. Place your right hand behind your head.
- Using your left hand, use the same circular motion with finger pads and varying pressure levels as you did in the shower to examine your entire right breast and armpit area.
- Repeat these steps on your left breast with the pillow under your left shoulder.
What’s Next?
If you feel a lump or notice any of the changes we’ve discussed, don’t panic. Remember that most changes are benign. Simply note what you’ve found and schedule an appointment with your doctor to have it checked. You are taking control of your health, and that is always the right thing to do.
Risk Factors for Women Under 40
Understanding your personal risk profile is a key part of being proactive about your breast health. It allows you to have a more informed and productive conversation with your doctor about a personalized screening or prevention plan. While having a risk factor does not mean you will get cancer, it’s important to be aware of them.
Here is a deeper look at the key risk factors for young women:
- Family History: This is one of the strongest known risk factors. Having one or more first-degree relatives (a mother, sister, or daughter) diagnosed with breast cancer, especially if they were premenopausal, or a family history of ovarian cancer, significantly increases your risk. Knowing your family’s health history on both your mother’s and father’s side is crucial.
- Inherited Genetic Mutations: About 5-10% of breast cancers are linked to inherited gene mutations. The most well-known are the BRCA1 and BRCA2 genes. These genes normally help suppress tumors, but specific mutations can dramatically increase the lifetime risk of both breast and ovarian cancer. Other genes, like PALB2, TP53, and CHEK2, also play a role. Genetic counseling and testing may be recommended if you have a strong family history.
- Personal Health History: Your own medical history matters. A woman who has had cancer in one breast has a higher risk of developing a new cancer in the other breast or in another part of the same breast. Additionally, certain non-cancerous breast conditions, like atypical hyperplasia (an overgrowth of abnormal cells), can increase your risk.
- Dense Breast Tissue: Having dense breasts (more glandular and fibrous tissue than fatty tissue) is a common risk factor for young women. Not only does it increase your relative risk of developing breast cancer, but as discussed earlier, it also makes cancer harder to detect on a mammogram.
- Previous Chest Radiation: If you received radiation therapy to the chest for another cancer (such as Hodgkin or non-Hodgkin lymphoma) as a child or young adult, your risk of breast cancer is significantly increased. This is why survivors of childhood cancers require specialized, early screening.
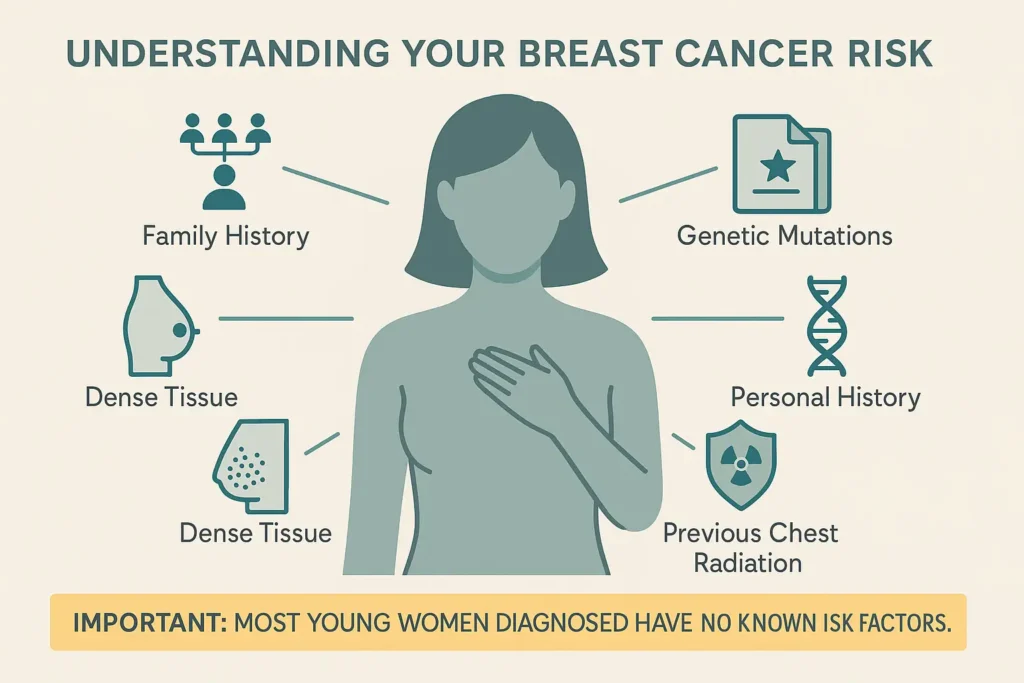
The Most Critical Takeaway
Despite this list, it is essential to internalize this fact: Approximately 80% of young women diagnosed with breast cancer have no known family history and no identifiable risk factors beyond their age and gender.
This is not a reason to dismiss these risk factors, but rather a powerful reminder that breast cancer can happen to anyone. This is precisely why universal awareness—knowing your body, recognizing the signs, and advocating for yourself—is so vital for every woman, regardless of her family history or perceived risk.
You’ve noticed a change. That initial moment of discovery can be filled with a flood of emotions—fear, confusion, denial. The most important step you can take right now is to channel that energy into action. Your health is worth it.
When to Make the Appointment: The 2-Week Rule
If you notice any of the signs we’ve discussed—a lump, skin change, nipple inversion, or anything else that is new and unusual for you—and it persists for two weeks or more, it is time to schedule an appointment. This timeframe is long enough to rule out temporary hormonal fluctuations but short enough to ensure timely follow-up.
Even more importantly, trust your intuition. If something just feels profoundly or persistently “wrong” or “off” in your body, even if you can’t pinpoint a specific symptom from a list, that is a valid reason to see a doctor. You know your body better than anyone.
Your Script for Empowerment:
When you call or during your appointment, be direct. You can say:
- “I’ve found a persistent lump in my breast/armpit, and I’d like to have it checked.”
- “I’ve noticed a new and lasting change in the skin on my breast, and I’m concerned.”
- “I know my body, and something doesn’t feel right. I need a clinical breast exam.”
Remember:
- You are not wasting anyone’s time. This is precisely what doctors are for.
- Do not let fear talk you out of it. The anxiety of not knowing is almost always worse than the process of finding out.
- You are being your own best health advocate. This is a sign of strength, not hypochondria.
What to Expect at the Doctor’s Office: Demystifying the Process
Knowing what might happen can significantly reduce anxiety. The goal of these appointments is to find an explanation for your symptoms. Here is a typical roadmap:
1. The Clinical Breast Exam (CBE)
Your doctor will perform a physical examination similar to the self-check you did at home, but with a trained, clinical touch. They will systematically feel your breast tissue, chest wall, and lymph nodes in your armpits and around your collarbone, assessing the size, texture, and mobility of any lump you’ve found.
2. Diagnostic Imaging: A Closer Look
If the CBE finds anything of concern, or if your symptom is clear (like spontaneous nipple discharge), the next step is imaging.
- Breast Ultrasound: This is often the first imaging test for women under 40. It uses sound waves to create a picture of the inside of your breast. It’s excellent for distinguishing between a solid mass (which needs further investigation) and a fluid-filled cyst (which is usually harmless). It’s also ideal for looking at dense breast tissue.
- Diagnostic Mammogram: This is a more detailed X-ray than a screening mammogram. It takes multiple images of the breast, focusing on the specific area of concern. The technologist may place a small marker on the spot you’re worried about.
3. The Biopsy: The Only Way to Be Sure
If the imaging reveals a suspicious area, a biopsy is the next and only definitive step. A biopsy is the only way to diagnose breast cancer.
- What it is: A doctor uses a needle to remove small samples of tissue from the area in question. This is typically done using local anesthesia to numb the area, and image-guidance (like an ultrasound) to ensure accuracy.
- It sounds scarier than it is. Most breast biopsies are minimally invasive procedures. You will be awake but numb, and it usually leaves only a tiny mark, similar to a blood draw.
- The tissue samples are then sent to a pathologist, who examines them under a microscope to determine if cancer cells are present. This process usually takes a few days.
This diagnostic journey is a process of gathering information. Each step is designed to get a clearer picture and guide the next step. By taking action, you are taking control.
Debunking Common Myths About Breast Cancer and Age
Misinformation can be one of the biggest barriers to early detection. When it comes to breast cancer and young women, certain persistent myths can create a false sense of security, leading to delayed diagnosis. Let’s shatter these dangerous misconceptions with facts.
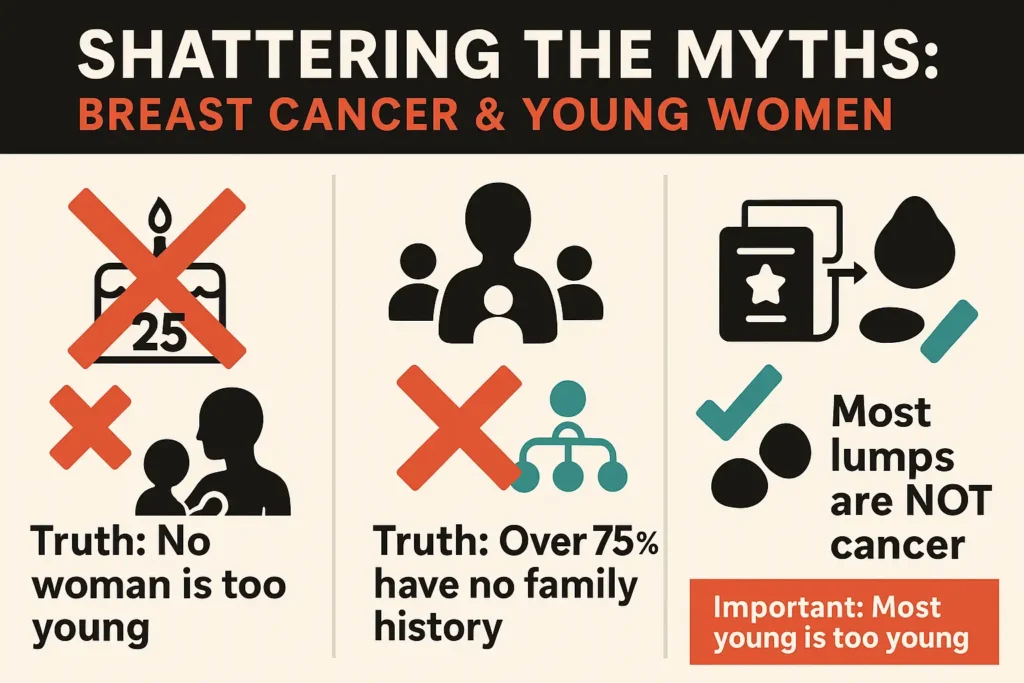
Myth 1: “I’m Too Young to Get Breast Cancer.”
- The Dangerous Belief: Breast cancer is exclusively an “older woman’s disease,” and women in their 20s and 30s are immune.
- The Truth: While it’s true that your risk increases with age, no woman is “too young.” Breast cancer is the most common cancer in women of all ages. Thousands of women under 40 are diagnosed each year. Age alone is not a shield, which is why awareness at every stage of life is non-negotiable.
Myth 2: “I Don’t Have a Family History, So I’m Safe.”
- The Dangerous Belief: Breast cancer only runs in families. If your mother, grandmother, or aunts never had it, you have nothing to worry about.
- The Truth: This is one of the most critical myths to correct. The reality is that only about 10-15% of women diagnosed with breast cancer have a known family history. The vast majority—over 75%—have no family history at all. Breast cancer is often a sporadic event, meaning it can happen to anyone, regardless of their family tree. Your greatest risk factor is simply being a woman.
Myth 3: “If I Find a Lump, It Means I Have Cancer.”
- The Dangerous Belief: Every lump equals a cancer diagnosis, which can cause such intense fear that it prevents women from getting a lump checked.
- The Truth: The good news is that the overwhelming majority of breast lumps are benign (non-cancerous). Common causes include cysts (fluid-filled sacs) and fibroadenomas (solid, benign tumors). However—and this is crucial—while most lumps are harmless, it is impossible to know without a professional medical evaluation. This is why the message is not “don’t worry,” but “get it checked.” A doctor’s visit brings clarity and peace of mind.
Why This Matters:
Believing these myths can be a form of self-sabotage. They talk you out of making that doctor’s appointment. They convince you to wait and see. By replacing myth with fact, you empower yourself to take action, advocate for your health, and respond to changes in your body with knowledge, not fear.
Conclusion: Your Health is in Your Hands
The truth about breast cancer in women under 40 is that it’s a real possibility, but one you can face with knowledge and confidence. You don’t need to live in fear. Instead, live in awareness.
Know your body. Trust your instincts. Advocate for your health.
Schedule that self-check today. Share this information with your friends, sisters, and colleagues. By spreading awareness, we empower a generation of women to take control of their health, catch warning signs early, and ultimately, save lives.
Ressources
- American Cancer Society (ACS)
A comprehensive resource for information on all types of cancer, including prevention, detection, and support. Their guide to breast cancer is particularly helpful. - National Cancer Institute (NCI)
As part of the U.S. National Institutes of Health, the NCI provides in-depth, research-based information on breast cancer.- Website: www.cancer.gov/types/breast
- Breastcancer.org
A patient-focused organization dedicated to providing reliable, up-to-date information on all aspects of breast cancer.- Website: www.breastcancer.org
- Young Survival Coalition (YSC)
This one is crucial for your audience. YSC is the premier organization dedicated to the unique concerns of young women diagnosed with breast cancer. They offer resources, support networks, and community.- Website: www.youngsurvival.org
- FORCE: Facing Our Risk of Cancer Empowered
An invaluable resource for women concerned about genetic risks and hereditary breast and ovarian cancer.- Website: www.facingourrisk.org

