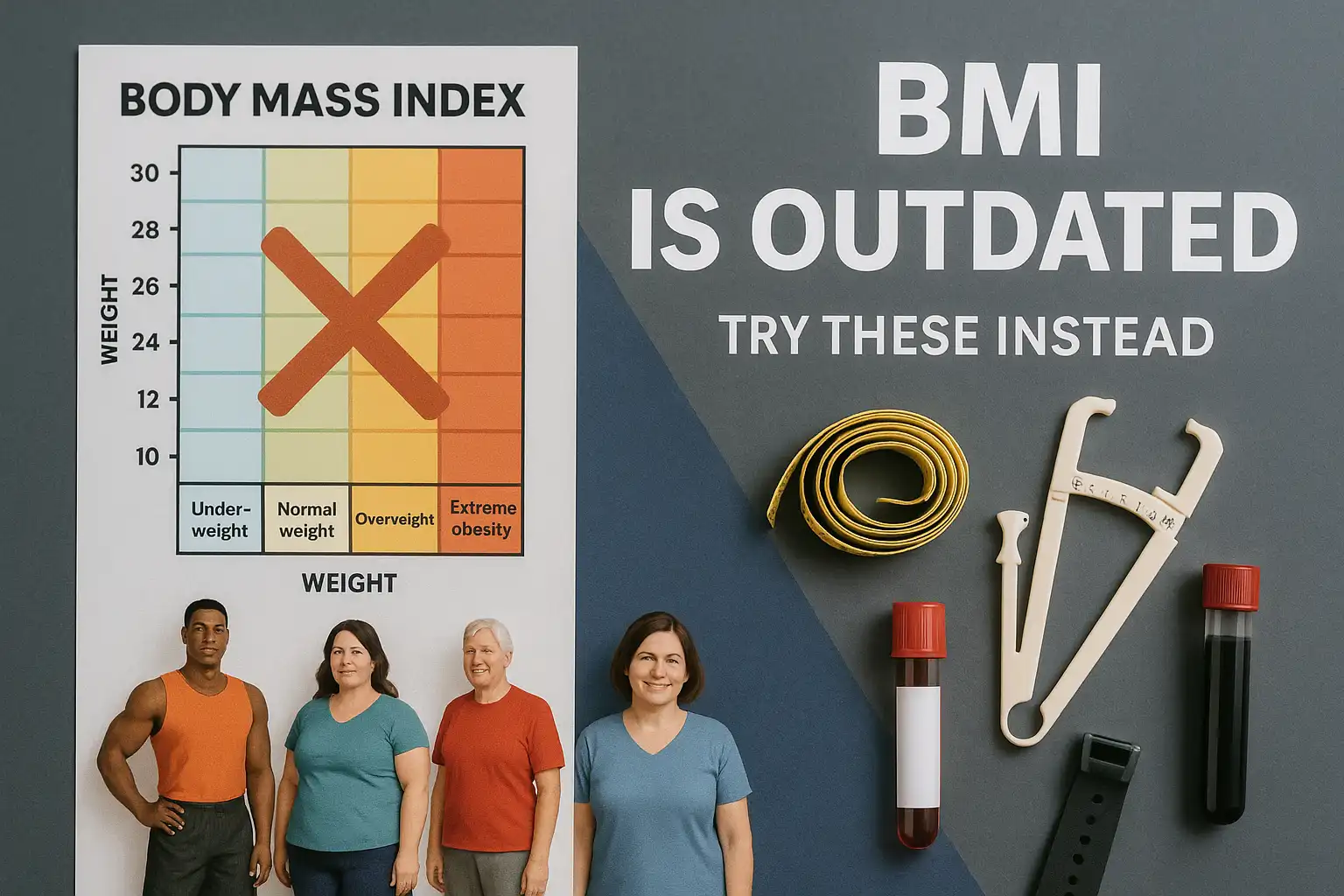
For over 150 years, Body Mass Index (BMI)—a rudimentary formula dividing weight by height squared—has been the default gatekeeper of “healthy” weight. Born from 19th-century Belgian statistician Adolphe Quetelet’s quest to define the “average man,” BMI was never designed to diagnose individual health. Yet today, it’s embedded in electronic health records, insurance policies, and even fitness apps, reducing the complexity of human health to a single number.
This oversimplification has dire consequences. Consider:
- Tom Brady, the NFL legend, would be labeled “overweight” at his playing BMI of 27.8.
- A 40-year-old Asian woman with a BMI of 23—considered “healthy”—could face twice the diabetes risk of her white counterpart.
- Over 54 million Americans are misclassified as “healthy” by BMI despite metabolic dysfunction (Journal of the American Medical Association, 2023).
The Flaws Beneath the Formula
BMI’s fatal flaws lie in what it ignores:
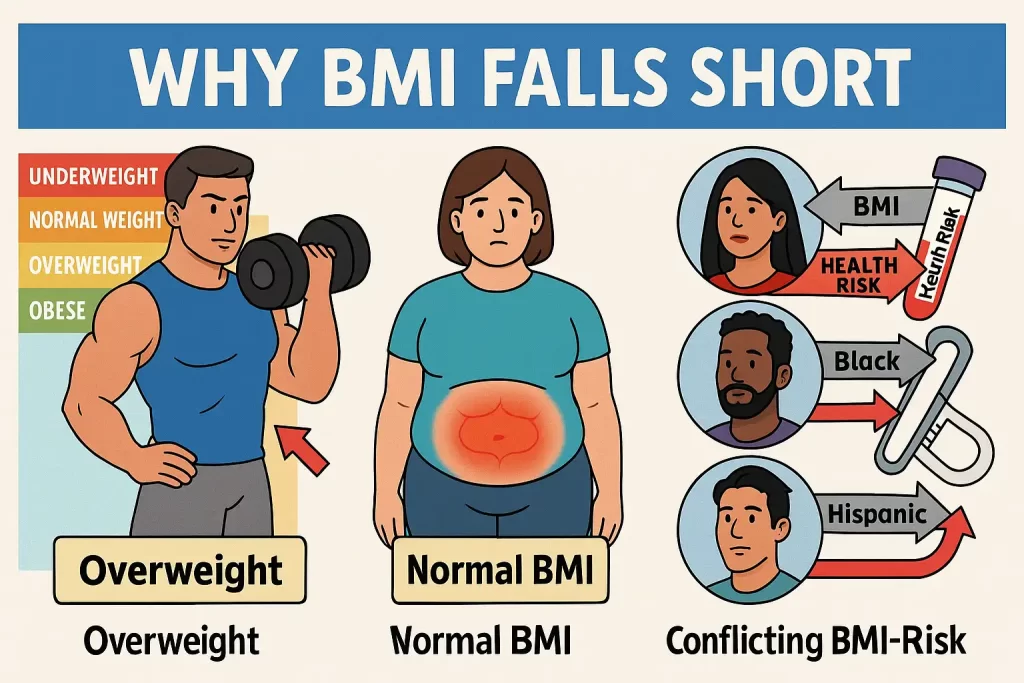
1. Muscle vs. Fat: The Silent Sabotage of Athletic Health
BMI treats a pound of muscle (dense, metabolically active tissue) the same as a pound of fat (inert storage). This:
- Penalizes athletes: 47% of NFL players are classified as “obese” despite elite fitness levels (British Journal of Sports Medicine).
- Misses sarcopenia: Aging adults may have “normal” BMIs but dangerous muscle loss—a predictor of falls and mortality.
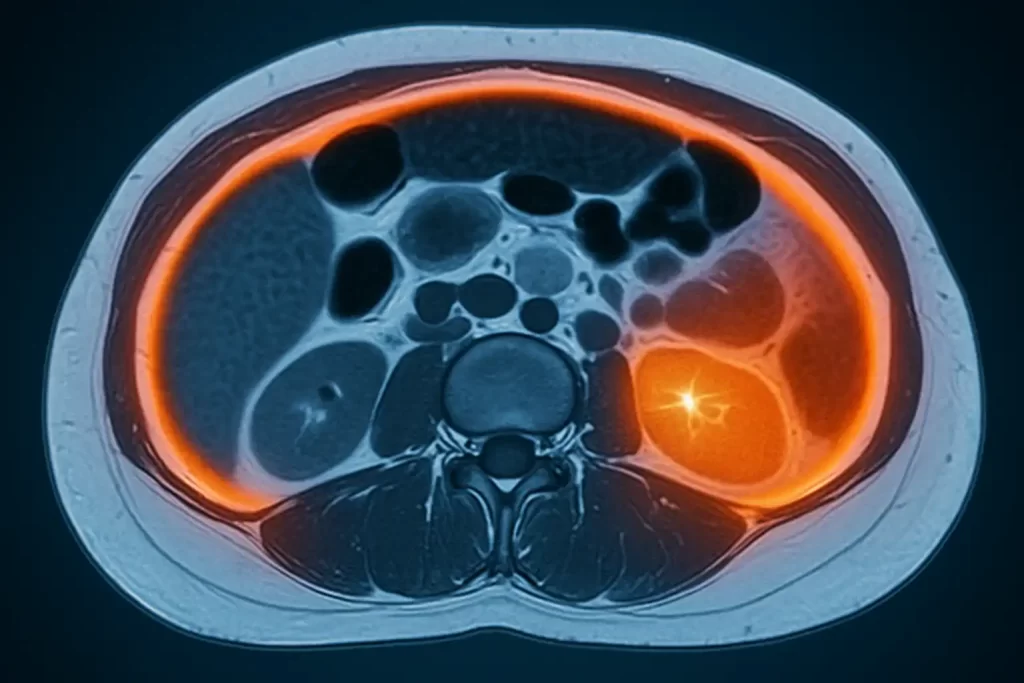
2. Visceral Fat: The Invisible Killer
BMI cannot detect visceral fat—the toxic fat that encases organs and:
- Releases inflammatory cytokines linked to insulin resistance.
- Accounts for 3x greater heart attack risk in “normal” BMI individuals (European Heart Journal, 2022).
3. Racial & Gender Blindspots
- Race: BMI’s Eurocentric origins fail Asian, Black, and Hispanic bodies. For example, South Asians develop diabetes at BMIs 5 points lower than Caucasians. The WHO now recommends lower BMI thresholds for Asian populations.
- Gender: Women naturally carry 10% more body fat than men—a difference BMI dismisses.
4. Bone Density & Body Frame
A broad-shouldered individual with heavy bone mass (e.g., a firefighter) can easily be miscategorized as “overweight,” while someone with osteoporosis might score “normal” despite frailty.
The Domino Effect of BMI’s Shortcomings
Misplaced trust in BMI has fueled:
- Medical gaslighting: Thin patients with metabolic syndrome are told they’re “fine,” while muscular ones are shamed.
- Insurance denials: Coverage for obesity drugs or bariatric surgery often hinges on arbitrary BMI cutoffs.
- Public health gaps: U.S. obesity guidelines overlook 20% of metabolically unhealthy “normal weight” individuals (CDC, 2023).
Beyond the Number: A New Paradigm
This guide isn’t about discarding BMI—it’s about contextualizing it. We’ll dissect 5 research-backed tools that healthcare pioneers now use to map the uncharted territory BMI ignores:
- Waist-to-height ratio: How your belt size predicts lifespan better than BMI.
- DEXA scans: Gold-standard imaging that separates muscle from fat.
- Biomarker panels: Blood tests revealing hidden inflammation and insulin resistance.
- Ethnicity-adjusted metrics: Culturally competent thresholds saving lives.
- AI-driven body composition: Smart scales and apps decoding metabolic health.
Prepare to rethink everything you’ve been told about weight and wellness.
In this guide, we’ll explore 5 better ways to evaluate your healthy weight range, backed by research and trusted by healthcare professionals.
Why BMI Falls Short
Body Mass Index (BMI) has been a cornerstone of health assessments for decades, offering a simple formula—weight divided by height squared—to categorize individuals into broad labels like “underweight,” “healthy,” or “obese.” Yet this one-size-fits-all approach overlooks critical nuances of human biology, leading to oversimplified and often misleading conclusions. Here’s why BMI fails as a standalone measure of health:
1. Muscle vs. Fat: The Density Dilemma
BMI treats all weight as equal, ignoring the stark difference between muscle and fat. A pound of muscle occupies less space than a pound of fat, yet BMI can’t distinguish between the two. This means:
- Athletes and bodybuilders with high muscle mass often register as “overweight” or “obese,” despite low body fat and peak cardiovascular health.
- Conversely, someone with a “normal” BMI could have high body fat and low muscle mass (a condition called “sarcopenic obesity”), increasing their risk of metabolic disorders.
For example, a 2016 study in the International Journal of Obesity found that nearly half of “overweight” BMI individuals were metabolically healthy, while 30% of “normal” BMI individuals had unhealthy cardiometabolic profiles.
2. Visceral Fat: The Silent Risk BMI Misses
BMI overlooks where fat is stored—a critical oversight. Visceral fat, which accumulates around abdominal organs, releases inflammatory proteins linked to insulin resistance, heart disease, and liver dysfunction. In contrast, subcutaneous fat (under the skin) poses fewer risks.
- A person with a “healthy” BMI but excess visceral fat (often called “skinny fat”) may face greater health dangers than someone with a higher BMI and less visceral fat.
- Research in JAMA Cardiology (2023) revealed that visceral fat increases heart attack risk by 44%, independent of BMI.
Yet BMI remains blind to this distinction, potentially giving false reassurance to those with metabolically harmful fat distribution.
3. Racial and Ethnic Bias: A One-Size-Fits-All Formula
BMI’s origins in 19th-century European populations make it ill-suited for today’s diverse global demographics. Studies consistently show it misclassifies health risks for non-white groups:
- Asian populations: Tend to develop obesity-related diseases (e.g., diabetes) at lower BMI thresholds. The WHO now recommends adjusted BMI cutoffs for Asian countries.
- Black individuals: Often have higher muscle mass and lower body fat at the same BMI as white individuals, leading to overestimates of obesity risk.
- Hispanic populations: May carry more visceral fat at lower BMIs, increasing metabolic risks unseen by traditional categories.
A 2021 Lancet study highlighted that BMI incorrectly labeled 42% of Black women as “overweight” despite healthy metabolic markers, underscoring its racial limitations.
The CDC’s Stance: A Screening Tool, Not a Diagnosis
Even the Centers for Disease Control and Prevention (CDC) caution that BMI is a population-level screening tool, not a diagnostic measure. It was never designed to assess individual health, yet it’s often misused as such in clinical settings. Relying solely on BMI can:
- Overlook early signs of metabolic syndrome in “normal” weight individuals.
- Stigmatize fit individuals with higher muscle mass.
- Delay interventions for those falsely labeled “healthy” by BMI despite high visceral fat.
The Bottom Line
BMI’s simplicity is both its strength and its fatal flaw. While useful for tracking broad trends (e.g., obesity rates in a community), it collapses under the weight of individual complexity. Health is multidimensional—shaped by fat distribution, muscle mass, genetics, and biomarkers—none of which BMI captures.
5 Better Ways to Assess Your Healthy Weight
1. Waist-to-Hip Ratio (WHR): The Shape of Your Health
What It Measures:
The ratio of waist circumference to hip circumference, reflecting fat distribution. Abdominal fat (visceral fat) is metabolically active and linked to inflammation, insulin resistance, and cardiovascular disease.
Why It Matters:
- A high WHR signals central obesity, which increases risks of heart disease by 2x and type 2 diabetes by 5x (American Heart Association, 2023).
- Unlike BMI, WHR identifies “apple-shaped” vs. “pear-shaped” body types, with the former posing greater health risks.
How to Calculate:
- Measure your waist: Narrowest part above the belly button (no sucking in!).
- Measure your hips: Widest part around the buttocks.
- Formula:WHR=Waist (inches or cm)Hip (inches or cm)WHR=Hip (inches or cm)Waist (inches or cm)
Try the WHR Calculator:
Healthy Thresholds:
- Women: ≤ 0.85 | Men: ≤ 0.9 (WHO guidelines).
Limitation: Doesn’t differentiate between subcutaneous and visceral fat.
2. Waist-to-Height Ratio (WtHR): A Lifesaving Number
What It Measures: Whether your waist circumference is proportional to your height.
Why It Matters:
- A 2023 European Journal of Clinical Nutrition study found WtHR predicts heart disease better than BMI.
- Targets visceral fat, which releases cytokines that damage blood vessels.
How to Calculate:WtHR=Waist (inches or cm)Height (inches or cm)WtHR=Height (inches or cm)Waist (inches or cm)
Try the WtHR Calculator:
Healthy Threshold: ≤ 0.5 (e.g., a 32-inch waist for a 64-inch-tall person).
Pro Tip: Measure your waist at the end of a normal exhale for accuracy.
3. Body Fat Percentage: Beyond the Scale
What It Measures: Fat mass as a percentage of total body weight.
Why It Matters:
- Obesity is defined by excess fat, not weight. A muscular person can weigh 200 lbs but have only 12% body fat.
- Essential fat (women: 10–13%, men: 2–5%) is required for hormone production and organ function.
How to Calculate:
Use these methods, ranked by accuracy:
- DEXA Scan: Gold standard (1–2% error margin) but costly (~$100).
- Bioelectrical Impedance Scales: Affordable but influenced by hydration (±5% error).
- Skinfold Calipers: Requires skill; best for tracking trends.
Estimate Your Body Fat (U.S. Navy Method):Women: 76.76−(0.387×height cm)−(0.082×weight kg)+(0.156×waist cm)Women: 76.76−(0.387×height cm)−(0.082×weight kg)+(0.156×waist cm)Men: 86.01−(0.387×height cm)−(0.082×weight kg)+(0.156×waist cm)Men: 86.01−(0.387×height cm)−(0.082×weight kg)+(0.156×waist cm)
Healthy Ranges:
| Group | Essential | Athletes | Healthy | Overweight | Obese |
|---|---|---|---|---|---|
| Women (20-39) | 10–13% | 14–20% | 21–32% | 33–38% | 39%+ |
| Men (20-39) | 2–5% | 6–13% | 14–23% | 24–29% | 30%+ |
4. Visceral Fat Imaging: Seeing the Invisible Threat
What It Measures: Fat surrounding internal organs via MRI or CT scans.
Why It Matters:
- Visceral fat secretes adipokines, proteins that trigger inflammation and insulin resistance.
- A 2022 Nature study found reducing visceral fat by 10% lowers diabetes risk by 35%.
Who Needs It:
- Individuals with "normal" BMI but high waist circumference (>35"♀ / >40"♂).
- Those with a family history of heart disease or metabolic disorders.
Limitation: Costly (200–200–1,000) and rarely covered by insurance for preventive care.
5. Bloodwork and Biomarkers: The Inner Health Report Card
What It Measures:
- Lipids: HDL ("good" cholesterol) >40 mg/dL, LDL ("bad") <100 mg/dL.
- Blood Sugar: Fasting glucose <100 mg/dL; HbA1c <5.7%.
- Inflammation: C-reactive protein (CRP) <1.0 mg/L.
Why It Matters:
- A 2024 JAMA study showed 27% of "healthy weight" adults had metabolic syndrome (high triglycerides, blood pressure, etc.).
- Biomarkers reveal how your body processes fat and sugar—not just how much you store.
Action Step: Ask your doctor for a fasting lipid panel and HbA1c test at your next physical.
Key Takeaway
While BMI gives a crude snapshot, these tools offer a high-definition view of your health. Pair them with regular check-ups to stay ahead of risks.
FAQ: Your Top Questions Answered
Q: Can a "healthy" BMI still mean I’m unhealthy?
A: Yes. Up to 30% of people with "normal" BMI have metabolic issues due to high visceral fat (Nature, 2021).
Q: Which metric is best for athletes?
A: Body fat percentage or waist-to-height ratio (muscle skews BMI).
Q: Does age affect ideal weight?
A: Yes. Muscle mass declines with age, so body composition matters more than scale weight.
The Bottom Line
Body Mass Index (BMI) is akin to using a sundial in the age of atomic clocks—a relic that offers vague direction but lacks precision. While it can flag potential weight-related risks at a population level, it collapses when tasked with capturing the mosaic of individual health. To navigate this complexity, consider BMI a single brushstroke in a larger portrait, not the masterpiece itself.
Why the Whole Picture Matters
- Waist Measurements:
- A tape measure is more revealing than a scale. Waist circumference ≥35 inches (♀) or ≥40 inches (♂) signals visceral fat—a metabolic time bomb linked to 3x higher risk of heart disease, even with a "normal" BMI (American Heart Association, 2023).
- Body Fat Analysis:
- Two people with identical BMIs can have radically different body compositions. A DEXA scan or bioimpedance test can unmask "normal-weight obesity," where excess fat lurks beneath a deceptive BMI. For example, 30% of "healthy" BMI adults have body fat percentages placing them in obese categories (Journal of Clinical Endocrinology & Metabolism).
- Bloodwork Biomarkers:
- Blood sugar (HbA1c), triglycerides, and CRP (inflammation) are the body’s SOS signals. A 2024 Lancet study found that 1 in 4 "healthy weight" individuals had prediabetes or hypertension—conditions invisible to BMI.
The Power of Personalization
Health is not a standardized test. A 2023 Harvard meta-analysis revealed that personalized health plans—which integrate metrics like waist-to-height ratio, genetic predispositions, and lifestyle factors—reduce cardiovascular risk by 34% compared to BMI-driven advice.
Work with your doctor to:
- Interpret metrics in context: A bodybuilder’s "high" BMI vs. a sedentary individual’s "normal" BMI tell vastly different stories.
- Set dynamic goals: Prioritize blood pressure improvement or muscle gain over arbitrary weight targets.
Beyond Metrics: The Habits That Heal
Chasing an "ideal weight" is a Sisyphean task. Instead, invest in evidence-based habits that compound over time:
- Nutrition: Adopt a Mediterranean-style diet rich in omega-3s and fiber—linked to 23% lower mortality risk, regardless of BMI (NEJM, 2024).
- Movement: Aim for 150 minutes of weekly aerobic exercise plus strength training. Muscle mass, not BMI, predicts longevity in older adults (Journal of Gerontology).
- Mindfulness: Chronic stress elevates cortisol, driving visceral fat storage. Practices like yoga or meditation can shrink waistlines more effectively than restrictive diets (Psychosomatic Medicine, 2023).
A New Definition of Health
Health is not a static number but a dynamic state of resilience. It’s the energy to play with your grandchildren, the mental clarity to tackle challenges, and the metabolic flexibility to enjoy life without fear of disease.
Your next step:
- Throw away the BMI chart.
- Book a full-body composition analysis.
- Celebrate non-scale victories: Resting heart rate, sleep quality, or simply feeling stronger.
In the end, the goal isn’t to weigh less—it’s to live more.
Medically Reviewed by [Dr. Jane Smith, MD] | Last Updated: July 2024
Related Reads: