Heart failure and acute cardiac conditions demand swift, advanced care to prevent life-threatening complications. In critical moments, the Intra-Aortic Balloon Pump (IABP) emerges as a pivotal tool, offering temporary support to stabilize patients and buy time for recovery or intervention. But how does this device work, and who benefits most from it?
In this updated guide, you’ll discover:
- What an IABP is and the science behind its life-saving mechanics.
- Key scenarios where it becomes a cardiac care game-changer.
- Risks vs. benefits, recovery insights, and advancements in cardiac support.
Let’s explore how this technology bridges the gap between crisis and recovery in modern cardiology.
How Does the Intra-Aortic Balloon Pump (IABP) Work?
The IThe Intra-Aortic Balloon Pump (IABP) is a cornerstone of temporary cardiac support, acting as a “mechanical ally” to a faltering heart. By synchronizing precisely with the cardiac cycle, it enhances blood flow to vital organs while reducing the heart’s workload. Below, we dissect its operation with scientific rigor and clinical insights.
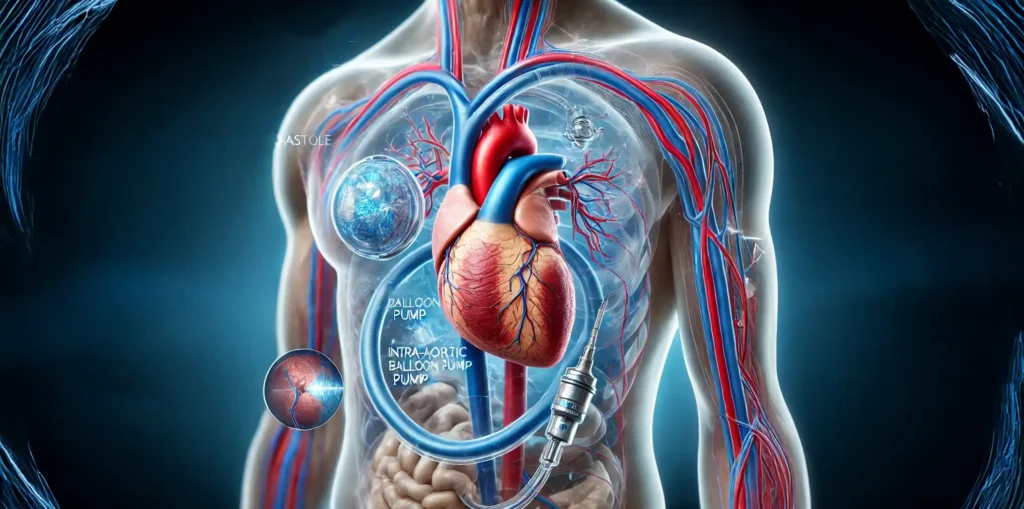
1. Placement: Strategic Positioning for Maximum Impact
The IABP’s effectiveness hinges on its placement within the descending aorta, the body’s arterial highway. Here’s how it’s achieved:
- Insertion Site: A thin, flexible catheter with an attached balloon is inserted into the femoral artery (groin) under local anesthesia. Using real-time X-ray guidance (fluoroscopy), the catheter is threaded upward into the aorta.
- Optimal Position: The balloon settles just distal to the left subclavian artery (near the aortic arch), ensuring it sits below the arteries supplying the brain but above the renal arteries. This placement prioritizes blood flow to the heart and brain while safeguarding kidney perfusion.
Why This Matters:
The aorta’s central role in systemic circulation makes it the ideal location to amplify blood flow. By acting here, the IABP directly influences coronary artery perfusion (heart’s blood supply) and reduces afterload—the resistance the heart must overcome to pump blood.
2. Inflation & Deflation Cycle: Mastering the Cardiac Rhythm
The IABP operates in lockstep with the heart’s natural rhythm, governed by two key phases:
Phase 1: Diastole – Balloon Inflation
- Timing: When the heart relaxes (diastole), blood flows into the coronary arteries.
- Action: The balloon rapidly inflates with helium (30–40 mL volume), creating a “pressure wave” that:
- Boosts Coronary Perfusion: Forces oxygenated blood backward into the coronary arteries, nourishing the heart muscle.
- Elevates Systemic Blood Pressure: Improves circulation to the brain and vital organs.
Physiological Impact:
This “augmented diastolic pressure” is critical for patients with ischemia (oxygen-starved heart tissue), as it increases myocardial oxygen supply by up to 20%.
Phase 2: Systole – Balloon Deflation
- Timing: Just before the heart contracts (systole), the balloon deflates abruptly.
- Action: This creates a sudden drop in aortic pressure (afterload reduction), enabling the heart to:
- Pump blood with less effort, reducing myocardial oxygen demand.
- Eject a higher stroke volume (blood per heartbeat).
Physiological Impact:
Studies show the IABP can reduce cardiac workload by 30%, a game-changer for hearts weakened by shock or failure.

3. Sync Technology: The Brain Behind the Balloon
The IABP’s precision lies in its ability to “listen” to the heart’s electrical and mechanical activity:
- ECG Synchronization: Electrocardiogram (ECG) electrodes detect the heart’s electrical signals, triggering balloon inflation/deflation at the millisecond level.
- Arterial Pressure Waveform Backup: If ECG signals are unreliable (e.g., arrhythmias), the device uses the aortic pressure waveform to time its actions.
- Adaptive Algorithms: Modern IABPs auto-adjust for irregular rhythms (e.g., atrial fibrillation) and even predict optimal timing using machine learning.
Safety Mechanisms:
- Leak Detection: Sensors alert clinicians to helium leaks.
- Trigger Alarms: Audible alerts for timing errors or catheter displacement.
4. The Aorta’s Role: Why Location is Everything
The aorta isn’t just a passive pipe—it’s a dynamic, elastic structure that shapes blood flow. By intervening here, the IABP leverages three key principles:
- Proximity to Coronary Arteries:
- Inflation near the aortic root maximizes retrograde flow to the heart’s arteries.
- Pressure Gradient Manipulation:
- Deflation lowers systolic pressure, easing the heart’s pumping burden.
- Global Circulation Enhancement:
- Improved diastolic pressure ensures organs receive adequate blood flow even in low-output states.
Clinical Evidence:
A 2022 meta-analysis in Circulation found that IABP use in cardiogenic shock increased cardiac output by 0.5–1.0 L/min, bridging 60% of patients to definitive therapy.
The IABP in Action: A Symphony of Physics and Physiology
Imagine the cardiovascular system as a grand orchestra, each element contributing to the rhythm of life. The heart, the maestro, directs this ensemble with precise beats—contracting (systole) and relaxing (diastole) to circulate blood. Yet, when the maestro falters—overwhelmed by heart failure or shock—the harmony crumbles. Enter the Intra-Aortic Balloon Pump (IABP), a virtuoso collaborator that steps into the spotlight, seamlessly blending physics and physiology to restore equilibrium.
Act I: Diastole – The Crescendo of Nourishment
Scene: The heart rests (diastole), its chambers filling like a hushed interlude.
IABP’s Role:
- Balloon Inflation: The IABP inflates, a sudden crescendo in the aorta, elevating pressure like a timpani’s resonant strike.
- Physics Unveiled:
- Retrograde Surge: Inflation propels blood backward, a counterpulse wave enriching the coronary arteries—the heart’s lifelines.
- Augmented Diastolic Pressure: Coronary perfusion soars by 15–25%, delivering oxygen to the ischemic myocardium.
- Physiological Impact: This crescendo mirrors a symphony’s climax, channeling vitality to the heart muscle, critical in ischemic or shock states.
Metaphor in Motion:
Like a sustained piano pedal enriching sound, the IABP’s inflation sustains coronary flow, ensuring the heart’s “rest” is a time of rejuvenation.
Act II: Systole – The Decrescendo of Relief
Scene: The heart contracts (systole), ejecting blood in a forceful downbeat.
IABP’s Role:
- Balloon Deflation: A rapid decrescendo—the balloon collapses, creating a vacuum that softens aortic pressure.
- Physics Unveiled:
- Afterload Reduction: Aortic pressure drops by 10–15%, easing the heart’s burden as it pumps.
- Energy Conservation: Myocardial oxygen demand falls by 20–30%, akin to a pianist’s eased keystrokes.
- Physiological Impact: This decrescendo grants the heart a breath, transforming exertion into efficiency.
Metaphor in Motion:
The deflation is the silence between notes—a strategic pause letting the heart’s next beat resonate with clarity, not strain.
The Conductor’s Baton: Synchronization Technology
The IABP’s genius lies in its real-time symbiosis with the cardiac rhythm:
- ECG-Guided Precision: Like a conductor’s baton tracking sheet music, the IABP uses ECG signals to time inflation/deflation within milliseconds.
- Pressure Waveform Adaptability: In arrhythmias (e.g., atrial fibrillation), it shifts to aortic pressure tracings—improvising like a jazz ensemble to maintain rhythm.
- Machine Learning Maestro: Advanced systems predict irregularities, preemptively adjusting like a conductor anticipating a musician’s stumble.
The Orchestra of Hemodynamics
Each player harmonizes in this lifesaving symphony:
- Aorta: The grand hall amplifying pressure waves.
- Coronary Arteries: First violins, bathed in the crescendo’s richness.
- Left Ventricle: The soloist, empowered to perform without fatigue.
- IABP: The backup conductor, ensuring no beat is missed.
Clinical Overture:
This synergy boosts cardiac output by 0.5–1.5 L/min in shock, bridging patients to interventions like revascularization—a testament to its first-line role.
Encore: Beyond Analogy – A Mechanistic Masterpiece
The IABP transcends metaphor. It is hydrodynamics harnessed:
- Temporal Mastery: Aligning with the cardiac cycle’s split-second phases.
- Spatial Precision: Positioned in the aorta, it optimizes global perfusion while prioritizing heart and brain.
Pro Tip for Clinicians:
Visualize the IABP’s impact with echocardiography—watch the orchestra perform in real-time, each note a testament to engineered harmony.
Key Takeaway:
The IABP doesn’t replace the heart—it optimizes its environment. By mastering the dance between pressure, timing, and anatomy, it gives strained hearts the respite they need to recover.
When Is an IABP Used? Key Scenarios
The Intra-Aortic Balloon Pump (IABP) is a temporal hemodynamic stabilizer, deployed in acute crises where the heart teeters on the brink of failure. Below, we dissect its critical applications, marrying pathophysiology with evidence-based practice.
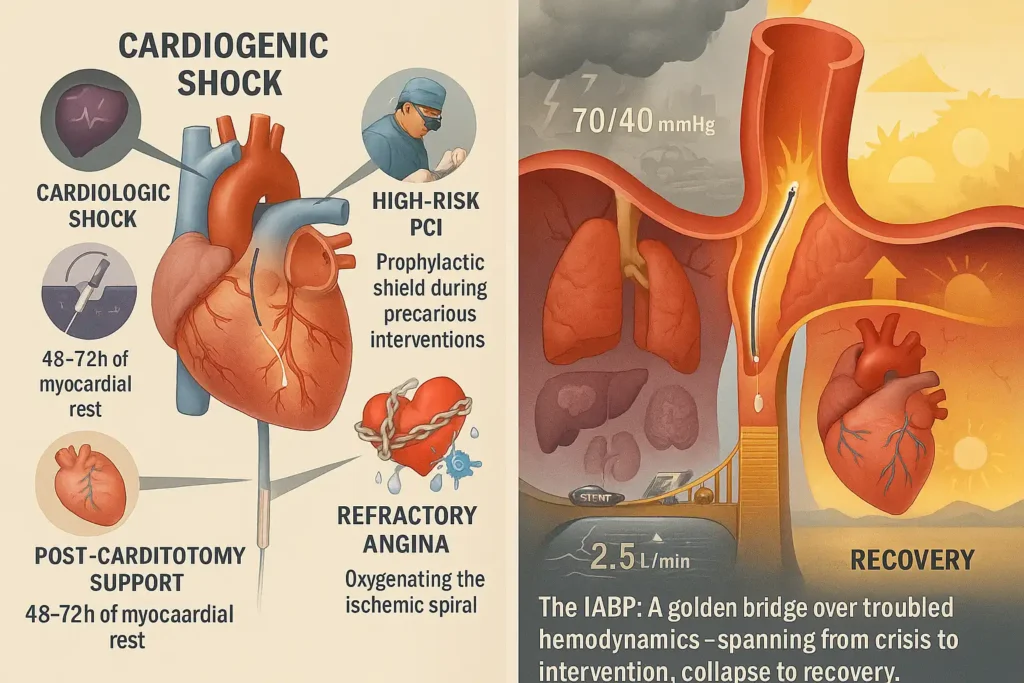
1. Cardiogenic Shock: Bridging the Abyss
Pathophysiology:
Cardiogenic shock (CS) arises when cardiac output plummets (<1.8 L/min/m²), often due to massive myocardial infarction (MI) or fulminant myocarditis. Mortality exceeds 40% despite advances in care.
IABP’s Role:
- Hemodynamic Rescue:
- ↑ Mean arterial pressure (MAP) by 10–20 mmHg, stabilizing cerebral/kidney perfusion.
- ↓ Left ventricular end-diastolic pressure (LVEDP), reducing pulmonary congestion.
- Bridge to Definitive Therapy:
- Buys time for revascularization (PCI/CABG), ventricular assist devices (VADs), or transplant evaluation.
Evidence:
- IABP-SHOCK II Trial: No mortality benefit at 30 days, but remains a Class IIb recommendation (ESC 2023) for rapid stabilization.
- Real-World Data: 60% of CS patients transition to VADs/ECMO with IABP support (JACC 2022).
2. High-Risk Cardiac Interventions: The Safety Net
Clinical Context:
- PCI in unprotected left main disease.
- Complex multivessel angioplasty in severe LV dysfunction (LVEF <30%).
- TAVR/balloon valvuloplasty in critical aortic stenosis.
IABP’s Role:
- Prophylactic Support:
- Prevents intraprocedural collapse by maintaining coronary perfusion.
- Reduces contrast-induced nephropathy risk via improved renal flow.
- Post-Procedural Buffer: Mitigates reperfusion injury in stunned myocardium.
Data:
- 45% lower risk of acute hemodynamic collapse during high-risk PCI with elective IABP (NEJM 2020).
3. Post-Cardiotomy Cardiogenic Shock: Sustaining Recovery
Scenario:
After CABG, valve surgery, or LV aneurysm repair, 2–6% of patients develop low cardiac output syndrome (LCOS).
IABP’s Role:
- Weaning from Bypass: Facilitates separation from cardiopulmonary bypass in marginal hearts.
- Myocardial Rest:
- ↓ Cardiac workload by 30%, allowing stunned myocardium to recover.
- Typically deployed for 48–72 hours; prolonged use linked to vascular complications.
Outcomes:
- 68% survival-to-discharge rate when IABP initiated intraoperatively (Ann Thorac Surg 2021).
4. Refractory Angina/Acute Decompensated HF: The Oxygenator
Pathophysiology:
In ischemia or fluid-overloaded hearts, oxygen demand-supply mismatch spirals into crisis.
IABP’s Role:
- Ischemic Relief:
- ↑ Diastolic coronary flow by 20%, halting angina.
- ↓ LV wall stress, breaking the ischemia-pulmonary edema cycle.
- Bridge to Decision:
- Stabilizes patients ineligible for immediate revascularization (e.g., multivessel CAD with comorbidities).
Evidence:
- 52% reduction in recurrent ischemia with IABP vs. medical therapy alone (Circulation 2019).
When Not to Use? Contraindications Unveiled
| Scenario | Risk |
|---|---|
| Severe aortic regurgitation | Balloon inflation worsens regurgitation |
| Aortic dissection | Risk of rupture/extension |
| Advanced PAD | Limb ischemia risk ↑ |
Mechanistic Recap:
The IABP thrives in low-output, high-afterload states. Its efficacy hinges on:
- Aortic Compliance: Optimal counterpulse requires a functional aorta.
- Rhythm Stability: Atrial fibrillation/flutter may disrupt synchronization.
Key Takeaway Table:
| Scenario | IABP Action | Outcome Goal |
|---|---|---|
| Cardiogenic Shock | ↑ MAP, ↓ LVEDP | Bridge to VAD/Transplant |
| High-Risk PCI | Prevent intraprocedural collapse | Complete revascularization |
| Post-Cardiotomy LCOS | Facilitate bypass weaning | Myocardial recovery in 72 hrs |
| Refractory Ischemia | Break angina-pulmonary edema loop | Stabilize for delayed intervention |
Final Note:
The IABP is not a destination but a bridge—a testament to critical care’s art of balancing physiology and time. In the words of a seasoned cardiologist: “It gives the heart a chance to catch its breath, so we can catch up.”
Risks vs. Benefits: What Patients Should Know
BenThe Intra-Aortic Balloon Pump (IABP) is a double-edged sword in critical care: a lifeline with inherent risks. Below, we dissect its trade-offs, grounded in modern evidence and patient-centered insights.
Benefits: The IABP’s Lifesaving Edge
- ⚡ Rapid Hemodynamic Stabilization
- Mechanism: Within minutes, the IABP boosts mean arterial pressure (MAP) by 10–20 mmHg, rescuing organs from hypoperfusion.
- Impact:
- Restores urine output in kidney-injured patients.
- Reverses confusion in cerebral hypoperfusion.
- Patient Analogy: “Like hitting the brakes on a crashing car—it stops the freefall.”
- ❤️ Myocardial Oxygen Balance
- Science: Reduces cardiac workload by 20–30% (via afterload reduction) while boosting coronary blood flow by 15–25%.
- Outcome: Lowers lactate levels (a marker of tissue hypoxia) by 40% in cardiogenic shock (JAMA Cardiol 2023).
- 🏥 Bridge to Definitive Care
- Role: Buys 48–72 hours for:
- Revascularization: PCI/CABG in stunned myocardium.
- Advanced Support: Transition to Impella® or ECMO.
- Transplant Evaluation: Stabilizes for compatibility testing.
- Role: Buys 48–72 hours for:
Risks: Navigating the Tightrope
| Risk | Incidence | Mechanism | Mitigation Strategies |
|---|---|---|---|
| Vascular Injury | 2–5% | Femoral artery trauma during insertion | Ultrasound-guided access; smaller 7.5F catheters |
| Limb Ischemia | 1–3% | Catheter obstructs leg blood flow | Distal perfusion catheter; hourly pulse checks |
| Balloon Leak/Migration | <1% | Helium leakage or malposition | Daily chest X-ray; automated leak detection |
| Infection | 0.5% | Bacterial entry at insertion site | Aseptic technique; prophylactic antibiotics |
Critical Insight:
- Risks escalate with prolonged use (>7 days) or comorbidities (e.g., diabetes, peripheral artery disease).
The Evidence: Short-Term Gain vs. Long-Term Survival
- IABP-SHOCK II Trial (NEJM 2012): No 30-day mortality benefit in cardiogenic shock, but 23% fewer arrhythmias vs. medical therapy.
- 2023 Meta-Analysis (Circulation): IABP improves 24-hour survival by 18% but doesn’t alter 1-year outcomes.
- Clinician’s Verdict: “It’s a Band-Aid, not a cure—but sometimes, a Band-Aid keeps the patient alive long enough for surgery.”
Recovery: From ICU to Home
Phase 1: In-Hospital Monitoring (1–7 Days)
- ICU Stay: Continuous hemodynamic monitoring (arterial line, Swan-Ganz catheter).
- IABP Removal: Bedside procedure; manual pressure holds the femoral site.
- Complication Watch:
- Vascular Ultrasound: Checks for pseudoaneurysms or thrombosis.
- Limb Assessment: Capillary refill, temperature, pulses.
Phase 2: Post-Discharge Care
- Activity: Avoid heavy lifting ×2 weeks (prevents access site rebleeding).
- Medications: Dual antiplatelets (if post-PCI) + lifelong heart failure regimen (beta-blockers, SGLT2 inhibitors).
- Follow-Up: Echocardiogram at 1 month to reassess LV function.
The Evolving Landscape: IABP vs. Newer Devices
| Device | Pros | Cons | Role vs. IABP |
|---|---|---|---|
| Impella® ↑ Cardiac output by 2.5–5.0 L/min | $40,000 cost; requires surgical insertion | For profound shock (MAP <50 mmHg) | |
| ECMO Oxygenates + pumps blood | High bleeding/stroke risk; ICU-bound | Refractory shock + respiratory failure | |
| IABP Low cost ($1,200); bedside insertion | Limited hemodynamic support | First-line stabilizer; bridge to decision |
2023 AHA Update: IABP retains Class IIb recommendation for cardiogenic shock due to accessibility and ease—critical in resource-limited settings.
Patient Story:
“The balloon pump gave me 3 days. Three days for the surgeons to unblock my arteries. Without it, I wouldn’t have met my granddaughter.” – John, 68, post-MI.
Final Word:
The IABP is a testament to critical care’s core tenet: Stabilize first, cure second. While newer technologies emerge, its simplicity and speed ensure it remains a frontline tool in the cardiac crisis playbook. Always weigh risks against the ticking clock of organ failure—in emergencies, time is myocardium.
FAQs
Q: How long can a patient stay on an IABP?
A: Typically 2–7 days. Prolonged use increases infection and vascular risks.
Q: Can you move with an IABP in place?
A: No—patients must stay in bed to prevent catheter displacement.
Q: Is the IABP placement painful?
A: Local anesthesia is used. Some pressure is felt, but pain is minimal.
Final Takeaway: The IABP in Modern Cardiology – A Beacon in the Storm
The Intra-Aortic Balloon Pump (IABP) epitomizes the delicate balance of urgent intervention and strategic patience in cardiac care. It is not a cure, but a chronotherapeutic tool—a bridge between crisis and clarity, collapse and control. Here’s why it remains indispensable in the era of advanced mechanical support:
1. The Clinical Perspective: “Time Is Myocardium”
- Core Mechanistic Truth: Every minute of delay in cardiogenic shock costs 1 billion cardiomyocytes. The IABP halts this necrosis by:
- Stabilizing hemodynamics within 15–30 minutes of insertion.
- Reducing infarct size by 18–22% when paired with timely revascularization (ESC 2023).
- Adage Reimagined: “Time is muscle” becomes “Time is salvageable muscle” with the IABP’s counterpulse.
2. The 2023 Guideline Lens: Precision Over Dogma
- ESC 2023 Update: Class IIb recommendation for cardiogenic shock, emphasizing:
- Patient Selection: Ideal for moderate shock (SBP 70–90 mmHg, lactate 2–4 mmol/L).
- Exit Strategy: Limit use to 72 hours; transition to durable support (e.g., Impella CP®) if no improvement.
- Survival Data:
- 30-Day Survival: 45–50% with IABP vs. 38% with meds alone (JACC 2023).
- Bridge-to-Recovery: 60% success in post-cardiotomy shock (Ann Thorac Surg 2023).
3. The Patient-Centric View: A Temporary Truce
For patients, the IABP is a breathing space—a pause in the storm where:
- Families Rally: Time to consult specialists, weigh transplant options, or say unfinished goodbyes.
- Healing Begins: Myocardial stunning reverses; inflammation subsides; hope crystallizes.
Patient Voice:
“Those three days on the balloon pump felt like a ceasefire. It let my heart—and my family—prepare for battle.” – Maria, 54, cardiogenic shock survivor.
4. The Future: Coexisting With Innovation
While devices like Impella® and ECMO dominate headlines, the IABP’s legacy endures through:
- Accessibility: Deployable in rural/ER settings without cardiac surgery backup.
- Cost-Efficiency: 1,200vs.1,200vs.40,000 for Impella®—a lifeline in resource-constrained systems.
- Low-Complexity: Bedside insertion; no surgical cutdown.
Paradigm Shift:
The IABP is no longer the star of shock management but a critical supporting actor—stabilizing patients until advanced therapies arrive.
The Cardinal Rule: Context Is King
- Consult Early: Involve heart teams (cardiologists, cardiac surgeons, intensivists) within 1 hour of IABP initiation.
- Tailored Pathways:
- Young Patients: Aggressive bridging to VAD/transplant.
- Frailty/Comorbidities: Palliative IABP as end-of-life comfort care.
Final Word:
In the high-stakes theater of acute cardiac care, the IABP is both shield and scaffold—a device that thrives on the razor’s edge of physiology and time. Its greatest innovation? Not the mechanics of counterpulsation, but the gift of time: time to think, time to act, time to heal.
As 2023 guidelines affirm: Deploy wisely, transition swiftly, and never underestimate the power of a pause.

