Root canals are one of the most frequently performed dental procedures, with more than 15 million carried out each year in the United States. Despite being a routine treatment, the mere mention of a root canal often sparks anxiety or uncertainty for many people. Whether you’ve been advised to get a root canal or are simply seeking to understand the process, this comprehensive guide is here to demystify the procedure. From the duration of the treatment to what you can expect during recovery, we’ll cover everything you need to know to feel informed and prepared. Let’s dive in and explore how a root canal can save your tooth, relieve pain, and restore your oral health.
What Is a Root Canal and Why Is It Needed?
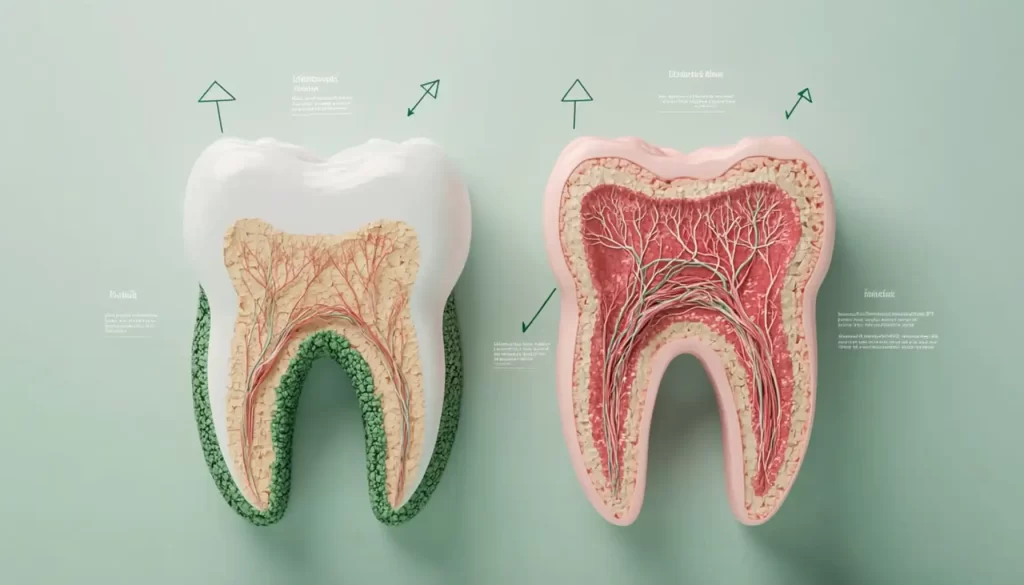
A root canal is a specialized dental procedure aimed at saving a tooth that has been severely damaged or infected. It’s a highly effective treatment that can relieve pain, prevent further complications, and preserve your natural tooth. The procedure involves removing the infected or inflamed pulp—the soft tissue inside the tooth that contains nerves, blood vessels, and connective tissue—cleaning and disinfecting the root canals, and then sealing the tooth to prevent reinfection.
While the idea of a root canal might sound daunting, it’s a routine procedure that has helped millions of people maintain their oral health and avoid tooth loss. Let’s take a closer look at why a root canal might be necessary and how it can benefit you.
Why Might You Need a Root Canal?
A root canal becomes necessary when the pulp inside your tooth becomes infected, inflamed, or damaged. This can happen for several reasons, including:
1. Deep Decay
Untreated cavities are one of the most common causes of pulp damage. When decay penetrates deep into the tooth, it can reach the pulp, causing infection and inflammation. If left untreated, the infection can spread, leading to more serious complications.
2. Cracked or Chipped Teeth
Physical injuries, such as a cracked or chipped tooth, can expose the pulp to bacteria. Even small cracks that aren’t visible to the naked eye can allow bacteria to enter and infect the pulp.
3. Repeated Dental Procedures
Teeth that have undergone multiple dental treatments (such as fillings or crowns) may become weakened over time. This can make the pulp more vulnerable to damage or infection.
4. Trauma to the Tooth
A blow to the mouth—whether from a sports injury, accident, or other impact—can damage the pulp, even if the tooth appears intact. Trauma can disrupt blood flow to the pulp, causing it to die and become infected.
What Happens If You Don’t Get a Root Canal?
Ignoring the signs of an infected or damaged tooth can lead to serious consequences, including:
- Spread of infection: The infection can spread to surrounding teeth, gums, and even the jawbone, causing abscesses or bone loss.
- Severe pain: As the infection worsens, the pain can become unbearable and may require emergency treatment.
- Tooth loss: In some cases, the only alternative to a root canal is tooth extraction, which can be more invasive and costly.
A root canal not only saves your natural tooth but also prevents the need for more complex and expensive procedures like dental implants or bridges.
How Does a Root Canal Help?
A root canal addresses the root cause of the problem—literally. By removing the infected or damaged pulp, cleaning and disinfecting the root canals, and sealing the tooth, the procedure:
- Eliminates pain: The source of the pain—the infected pulp—is removed, providing immediate relief.
- Prevents further damage: Sealing the tooth prevents bacteria from re-entering and causing reinfection.
- Preserves your natural tooth: Saving your natural tooth helps maintain your bite, chewing function, and overall oral health.
Final Thoughts
A root canal is a safe, effective, and often essential procedure for treating damaged or infected teeth. While the idea of a root canal might seem intimidating, it’s a routine treatment that can save your tooth, relieve pain, and prevent more serious health issues. If you’re experiencing tooth pain, sensitivity, or other symptoms, don’t wait—schedule an appointment with your dentist to determine if a root canal is the right solution for you.
By addressing the problem early, you can protect your smile and avoid more extensive dental work down the road. Remember, a root canal isn’t just about saving a tooth—it’s about preserving your oral health and quality of life.
How Long Does a Root Canal Take?
One of the most common questions about root canals is, “How long will I be in the dentist’s chair?” The answer depends on several factors, including the severity of the infection, the tooth being treated, and whether you need additional procedures like a crown.
Average Duration
- Simple root canals: 30 to 60 minutes for teeth with a single root canal (e.g., front teeth).
- Moderate cases: 90 minutes for teeth with multiple canals (e.g., premolars).
- Complex cases: Up to 3 hours for molars, which can have up to four canals.
Factors That Affect the Duration
- Tooth Location: Front teeth (incisors and canines) have fewer canals and are quicker to treat, while molars are more complex.
- Severity of Infection: Severe infections may require more time to clean and disinfect.
- Number of Appointments: Some root canals are completed in one visit, while others may require two or more appointments, especially if a crown is needed.
What Happens During a Root Canal?
If your dentist has recommended a root canal, you might be wondering what exactly the procedure entails. While the idea of a root canal can seem intimidating, understanding the process can help ease any anxiety you may have. A root canal is a carefully planned and executed procedure designed to save your natural tooth and relieve pain caused by infection or damage. Here’s a detailed, step-by-step breakdown of what to expect during a root canal:
Step 1: Examination and X-Rays
Before the procedure begins, your dentist will conduct a thorough examination of the affected tooth. This typically involves:
- Visual inspection: Checking for signs of infection, decay, or damage.
- X-rays: Taking detailed images to assess the extent of the damage, the shape of the root canals, and the location of the infection.
These steps help your dentist create a precise treatment plan and ensure the procedure is as efficient and effective as possible.
Step 2: Administering Anesthesia
Contrary to popular belief, a root canal is not a painful procedure. In fact, it’s designed to relieve pain, not cause it. To ensure your comfort, your dentist will:
- Numb the area: Local anesthesia is administered to the gums and surrounding tissues to completely numb the affected tooth and area.
- Ensure comfort: You may feel a slight pinch when the anesthesia is injected, but once it takes effect, you shouldn’t feel any pain during the procedure.
Modern anesthesia techniques make root canals no more uncomfortable than getting a routine filling.
Step 3: Isolating the Tooth with a Rubber Dam
To keep the treatment area clean and dry, your dentist will place a rubber dam around the tooth. This small, protective sheet:
- Prevents contamination: It keeps saliva and bacteria from entering the tooth during the procedure.
- Improves visibility: It provides a clear view of the tooth, allowing your dentist to work more precisely.
The rubber dam is a standard part of the procedure and ensures the highest level of hygiene and accuracy.
Step 4: Accessing the Pulp Chamber
Once the tooth is isolated, your dentist will:
- Create an access point: Using a dental drill, they’ll make a small opening in the crown (top) of the tooth to reach the pulp chamber.
- Remove damaged tissue: The pulp chamber houses the nerves, blood vessels, and connective tissue. If this pulp is infected or damaged, it must be removed to eliminate pain and prevent further infection.
This step is crucial for cleaning out the infected or inflamed pulp and preparing the tooth for treatment.
Step 5: Cleaning and Shaping the Root Canals
After accessing the pulp chamber, your dentist will:
- Remove the infected pulp: Using specialized tools, they’ll carefully clean out the pulp and any debris from the root canals.
- Disinfect the canals: The canals are flushed with antibacterial solutions to eliminate bacteria and prevent reinfection.
- Shape the canals: The canals are gently shaped to prepare them for filling. This step ensures that the filling material can be placed effectively.
This thorough cleaning process is essential for removing all traces of infection and ensuring the long-term success of the treatment.
Step 6: Filling the Canals
Once the canals are cleaned and shaped, they are filled with a biocompatible material called gutta-percha. This rubber-like material:
- Seals the canals: It prevents bacteria from re-entering the tooth.
- Provides stability: It helps maintain the structure of the tooth.
After filling the canals, your dentist will seal the access hole with a temporary or permanent filling.
Step 7: Temporary or Permanent Restoration
The final step depends on the condition of your tooth and your treatment plan:
- Temporary filling: If additional appointments are needed (e.g., for a crown), a temporary filling is placed to protect the tooth until the next visit.
- Permanent restoration: In some cases, your dentist may place a permanent filling or crown during the same appointment. A crown is often recommended for back teeth (molars and premolars) to restore strength and functionality.
What to Expect After the Procedure
After your root canal, you may experience some mild discomfort or sensitivity, but this can usually be managed with over-the-counter pain relievers. Your dentist will provide specific aftercare instructions, including:
- Avoiding chewing on the treated tooth until it’s fully restored.
- Maintaining good oral hygiene to promote healing.
- Scheduling follow-up appointments to monitor the tooth’s recovery.
Why a Root Canal Is Worth It
A root canal is a highly effective way to save a damaged or infected tooth, relieve pain, and prevent further complications. By understanding the steps involved, you can approach the procedure with confidence, knowing that it’s a routine and relatively painless process.
If you’re experiencing tooth pain or other symptoms, don’t wait—schedule an appointment with your dentist to determine if a root canal is the right solution for you.
Is a Root Canal Painful?
The idea of a root canal often conjures up images of excruciating pain, but modern dentistry has made the procedure relatively comfortable. Here’s what you need to know about pain during and after a root canal:
During the Procedure
- Local anesthesia: Ensures you feel little to no pain during the procedure.
- Pressure, not pain: You may feel some pressure as the dentist works, but it shouldn’t be painful.
After the Procedure
- Mild discomfort: It’s normal to experience some soreness or sensitivity for a few days after the procedure.
- Pain management: Over-the-counter pain relievers like ibuprofen or acetaminophen are usually sufficient to manage any discomfort.
- When to call your dentist: If the pain is severe or lasts more than a week, contact your dentist, as this could indicate a complication.
Root Canal Aftercare: Tips for a Smooth Recovery
Proper aftercare is essential to ensure a smooth recovery and prevent complications. Here are some tips to follow after your root canal:
Immediate Aftercare
- Avoid chewing on the treated tooth: Until the permanent restoration is placed, avoid putting pressure on the tooth to prevent damage.
- Stick to soft foods: Opt for foods like yogurt, mashed potatoes, and soup for the first few days.
- Practice good oral hygiene: Brush and floss gently, avoiding the treated area if it’s sensitive.
Long-Term Care
- Get a crown: If recommended by your dentist, a crown will protect the tooth and restore its function.
- Attend follow-up appointments: Regular check-ups will ensure the tooth is healing properly.
- Maintain oral hygiene: Brush twice a day, floss daily, and schedule regular cleanings to keep your teeth healthy.

Signs You Might Need a Root Canal
A root canal is often the best solution to save a tooth that’s severely damaged or infected. But how do you know if you need one? While only a dentist can provide a definitive diagnosis, there are several telltale signs that may indicate a root canal is necessary. If you’re experiencing any of the following symptoms, it’s crucial to schedule an appointment with your dentist as soon as possible. Ignoring these signs could lead to worsening pain, infection, or even tooth loss.
1. Persistent Tooth Pain
One of the most common signs that you might need a root canal is persistent tooth pain. This pain can range from a dull ache to a sharp, throbbing sensation and often worsens when you chew, bite down, or apply pressure to the tooth. The pain may come and go, but if it lingers or becomes more intense over time, it could indicate that the pulp inside your tooth is infected or inflamed.
Why it happens: The pain is caused by damage to the nerves and blood vessels in the pulp, which can occur due to deep decay, trauma, or a crack in the tooth.
2. Sensitivity to Hot and Cold
If you notice lingering sensitivity or pain after eating or drinking hot or cold foods, it could be a sign that the nerves inside your tooth are damaged. While some sensitivity is normal, especially after dental work, pain that persists long after the hot or cold stimulus is gone is a red flag.
Why it happens: Damaged or infected pulp can cause the nerves in your tooth to overreact to temperature changes, leading to prolonged discomfort.
3. Swollen or Tender Gums
Swelling or tenderness in the gums near the affected tooth is another common symptom of a tooth infection. The swelling may be localized to one area or spread to other parts of your mouth. In some cases, the gums may feel warm to the touch or appear red and inflamed.
Why it happens: Swelling occurs as your body’s immune system tries to fight off the infection. If the infection spreads, it can lead to an abscess, which is a pocket of pus that forms at the root of the tooth.
4. Tooth Discoloration
A tooth that has turned grayish or blackish may indicate that the pulp inside is dead or dying. This discoloration happens because the blood vessels and nerves in the pulp have been damaged, causing the tooth to lose its natural color.
Why it happens: Trauma to the tooth or prolonged infection can disrupt blood flow to the pulp, leading to discoloration.
5. Pimple on the Gums (Abscess)
A small, pimple-like bump on the gums near the affected tooth is a clear sign of infection. This bump, known as a gum boil or abscess, may ooze pus and can cause a bad taste in your mouth or foul-smelling breath.
Why it happens: An abscess forms when bacteria from the infected pulp spread to the surrounding tissue. It’s your body’s way of trying to contain the infection, but it requires immediate dental attention.
Other Symptoms to Watch For
In addition to the signs above, you may also experience:
- Loose teeth: An infection can weaken the bone and ligaments supporting the tooth, causing it to feel loose.
- Pain that radiates: The pain may spread to your jaw, ear, or other teeth.
- Fever or general discomfort: In severe cases, the infection can cause systemic symptoms like fever or fatigue.
What Should You Do If You Notice These Signs?
If you’re experiencing any of these symptoms, don’t wait—schedule an appointment with your dentist right away. Early intervention can prevent the infection from spreading and save your tooth. During your visit, your dentist will:
- Examine the affected tooth.
- Take X-rays to assess the extent of the damage.
- Determine whether a root canal is necessary.
Final Thoughts
While the idea of a root canal may seem intimidating, it’s a highly effective way to relieve pain, save your natural tooth, and prevent further complications. Ignoring the signs of a damaged or infected tooth can lead to more serious issues, including tooth loss or the spread of infection to other parts of your body.
If you’re experiencing persistent tooth pain, sensitivity, swelling, or any of the other symptoms mentioned above, don’t delay—seek professional dental care as soon as possible. Your dentist can help you determine the best course of action to restore your oral health and keep your smile intact.
Potential Complications and How to Avoid Them
While root canals are generally safe and effective, complications can occur in rare cases. These include:
- Reinfection: If the tooth isn’t properly sealed, bacteria can re-enter and cause infection.
- Cracked tooth: A weakened tooth may crack, requiring additional treatment.
- Missed canals: Some teeth have extra canals that may be missed during the procedure.
To minimize the risk of complications:
- Choose an experienced dentist or endodontist.
- Follow all aftercare instructions.
- Attend follow-up appointments as scheduled.
Conclusion
A root canal is a highly effective way to save a damaged or infected tooth and prevent further complications. While the idea of a root canal may seem daunting, the procedure is relatively straightforward and much less painful than most people imagine. With proper care, a treated tooth can last a lifetime.
If you’re experiencing tooth pain or other symptoms, don’t wait—schedule an appointment with your dentist to determine if a root canal is right for you. Remember, addressing dental issues early can save you time, money, and discomfort in the long run.

