The Difference Between Leukemia Lymphoma and Myeloma lies in how each of these blood cancers originates, progresses, and affects the body. While they all share a common connection to the blood and immune systems, their specific characteristics make them unique and require distinct approaches to diagnosis and treatment.
Understanding these differences is vital for accurate medical care and for supporting those affected by these conditions. Whether it’s leukemia starting in the bone marrow, lymphoma impacting the lymphatic system, or myeloma affecting plasma cells, knowing the distinctions can bring clarity to these complex diseases.
In this article, you’ll discover:
- The distinct characteristics of leukemia, lymphoma, and myeloma.
- How each condition affects the body differently.
- Key symptoms, diagnostic methods, and treatment approaches.
Let’s unravel the difference between leukemia, lymphoma, and myeloma to empower better understanding and awareness.
What Are Blood Cancers?
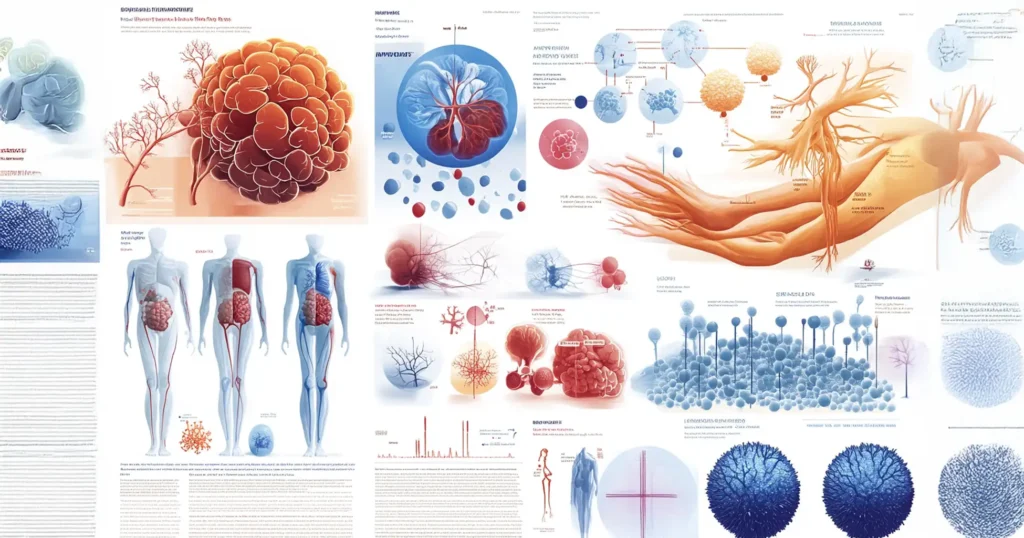
Blood cancers are a group of serious diseases that disrupt the normal functioning of the blood, bone marrow, and lymphatic system. These cancers alter the body’s ability to produce and regulate healthy blood cells, impairing essential functions such as immunity, oxygen transportation, and blood clotting. Blood cancers are among the most complex and challenging forms of cancer due to their widespread impact on the body’s vital systems.
How Blood Cancers Work
Blood cancers originate in blood-forming tissues, primarily the bone marrow. In a healthy body, bone marrow produces red blood cells (which carry oxygen), white blood cells (which fight infections), and platelets (which help in clotting). In cases of blood cancer, the process goes awry. Abnormal cells grow and multiply uncontrollably, crowding out healthy cells and disrupting normal blood functions.
Instead of maturing into functional blood cells, cancerous cells remain immature or develop abnormally. These cells can invade the bloodstream and other parts of the body, impairing organ function and increasing susceptibility to infections and complications.
Key Areas Affected
- Bone Marrow: The starting point of blood cell production and the primary site where abnormal cells originate.
- Bloodstream: Cancerous cells can travel through the bloodstream, spreading to other organs and affecting their performance.
- Lymphatic System: A crucial network of lymph nodes and vessels involved in immune response. Blood cancers often involve this system, disrupting its ability to fight infections effectively.
Categories of Blood Cancers
Blood cancers are broadly classified into three main types:
- Leukemia: Originates in the bone marrow and primarily affects white blood cells, leading to an overproduction of immature or dysfunctional cells.
- Lymphoma: Targets the lymphatic system, specifically lymphocytes, a type of white blood cell crucial for immunity.
- Myeloma: Affects plasma cells, another type of white blood cell, compromising the body’s ability to produce antibodies.
Why Understanding Blood Cancers Is Important
Awareness of blood cancers and their mechanisms is critical for early detection and treatment. By recognizing symptoms like unexplained fatigue, frequent infections, or abnormal bleeding, individuals can seek medical advice promptly. With advancements in diagnostic tools and therapies, many blood cancers are now manageable, and early intervention can significantly improve outcomes.
What Is Leukemia?
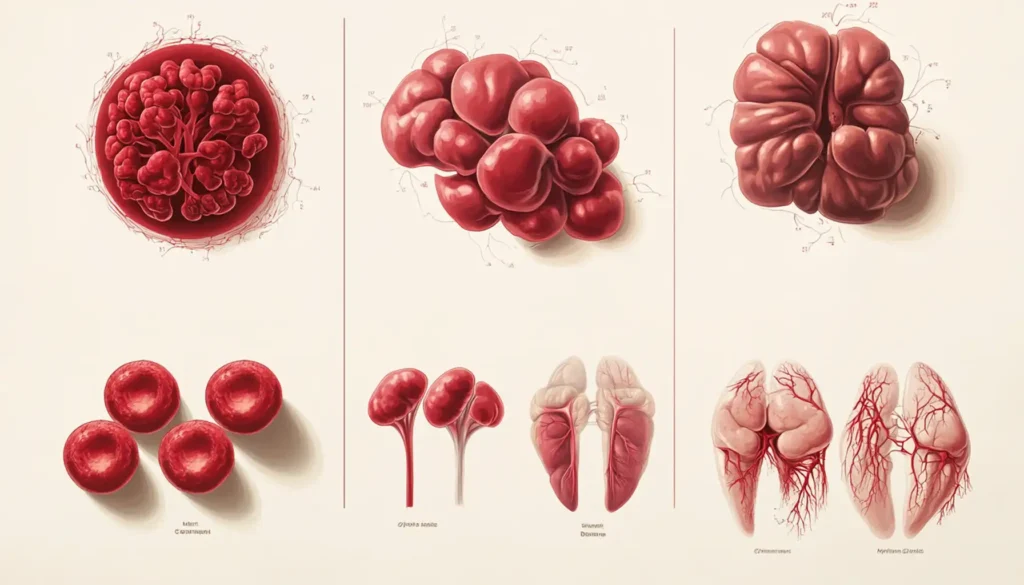
Leukemia is a type of blood cancer that originates in the bone marrow, the soft, spongy tissue inside bones responsible for producing blood cells. This cancer specifically affects the production and function of white blood cells, which play a crucial role in the body’s immune response. In leukemia, the bone marrow produces abnormal white blood cells that multiply uncontrollably, crowding out healthy cells and impairing the body’s ability to fight infections, carry oxygen, and form clots.
Types of Leukemia
Leukemia is classified based on how quickly it progresses (acute or chronic) and the type of white blood cells affected (lymphocytic or myeloid):
- Acute Leukemia:
- Progresses rapidly, requiring immediate treatment.
- Affects immature white blood cells (blasts) that cannot function properly.
- Chronic Leukemia:
- Progresses more slowly and may not require treatment immediately.
- Allows the production of some functional white blood cells but gradually worsens over time.
- Lymphocytic Leukemia:
- Originates in lymphocytes, a type of white blood cell crucial for the immune system.
- Myeloid Leukemia:
- Affects myeloid cells, which are precursors to various blood cell types, including red blood cells, platelets, and certain white blood cells.
How Leukemia Impacts the Body
Leukemia disrupts the delicate balance of blood cell production in the bone marrow. As abnormal white blood cells proliferate, they crowd out normal blood cells, leading to:
- Anemia: Low red blood cell count, causing fatigue and weakness.
- Infections: Reduced functional white blood cells compromise the immune system.
- Bleeding and Bruising: Fewer platelets result in clotting issues.
Leukemia’s wide-ranging effects make early detection and treatment critical for managing symptoms and improving outcomes.
What Is Lymphoma?
Lymphoma is a type of blood cancer that develops in the lymphatic system, a crucial part of the immune system responsible for transporting lymph fluid, nutrients, and white blood cells throughout the body. This cancer originates in lymphocytes, a type of white blood cell that helps the body fight infections. Abnormal lymphocytes multiply uncontrollably and can accumulate in lymph nodes, spleen, bone marrow, and other organs, impairing the immune system’s functionality.
Two Main Types of Lymphoma
- Hodgkin Lymphoma (HL):
- Distinguished by the presence of Reed-Sternberg cells, large abnormal lymphocytes that can be identified under a microscope.
- Typically spreads in an orderly manner from one group of lymph nodes to another.
- Often considered more treatable, with high survival rates when diagnosed early.
- Non-Hodgkin Lymphoma (NHL):
- Represents a diverse group of lymphomas that do not involve Reed-Sternberg cells.
- Can arise in different lymphocyte types (B cells or T cells).
- More variable in terms of progression, symptoms, and treatment options.
How Lymphoma Affects the Lymphatic System
The lymphatic system is a network of vessels and tissues that play a key role in maintaining fluid balance and immunity. Lymphoma disrupts this system by:
- Swelling Lymph Nodes: Abnormal lymphocytes collect in lymph nodes, causing painless swelling.
- Compromising Immunity: The accumulation of cancerous lymphocytes reduces the body’s ability to fight infections.
- Spreading to Other Organs: Lymphoma can spread to other parts of the body, including the liver, spleen, and bone marrow, further weakening overall health.
Understanding lymphoma’s types and effects is critical for recognizing symptoms early and pursuing appropriate treatment, which often includes chemotherapy, radiation, and immunotherapy.
What Is Myeloma?
Definition of Myeloma
Myeloma, also known as multiple myeloma, is a type of blood cancer that begins in plasma cells. Plasma cells are a crucial part of the immune system, responsible for producing antibodies to fight infections. In myeloma, abnormal plasma cells multiply uncontrollably in the bone marrow, disrupting the production of healthy blood cells.
Impact on Bone Health
One of the most notable effects of myeloma is its impact on bone health. The cancerous plasma cells release substances that activate bone-destroying cells called osteoclasts, leading to weakened bones, fractures, and pain. This process can result in bone lesions, often visible in imaging tests.
How It Affects the Immune System
The overproduction of abnormal plasma cells interferes with the immune system’s ability to function properly. Instead of creating effective antibodies, myeloma cells produce ineffective or harmful proteins known as M-proteins. This weakens the body’s ability to fight infections and increases the risk of illnesses.
Understanding myeloma and its effects on the body is essential for recognizing its symptoms early and seeking timely medical intervention.
Key Differences Between Leukemia, Lymphoma, and Myeloma
Where Each Cancer Originates
- Leukemia: Starts in the bone marrow and primarily affects the production of white blood cells. It disrupts the balance of blood cells, leading to issues like anemia, infections, and clotting problems.
- Lymphoma: Originates in the lymphatic system, particularly in lymph nodes or lymphatic tissues. It primarily impacts the lymphocytes, a type of white blood cell involved in immune response.
- Myeloma: Develops in plasma cells found in bone marrow. These abnormal cells interfere with bone health and weaken the immune system by producing ineffective antibodies.
Differences in Symptoms and Progression
- Leukemia: Common symptoms include fatigue, frequent infections, unexplained bruising, and bleeding. It progresses as abnormal white blood cells crowd out healthy ones.
- Lymphoma: Symptoms often include swollen lymph nodes, night sweats, fever, and weight loss. It progresses through the lymphatic system and can spread to other organs.
- Myeloma: Symptoms are more localized to bones and include bone pain, fractures, anemia, and increased risk of infections. It progresses by weakening bone structures and affecting kidney function.
Variations in Diagnosis and Treatment
- Leukemia: Diagnosed through blood tests and bone marrow biopsies. Treatment often includes chemotherapy, targeted therapy, and bone marrow transplants.
- Lymphoma: Diagnosed via lymph node biopsy and imaging tests. Treatments may include chemotherapy, radiation, immunotherapy, and stem cell transplants.
- Myeloma: Diagnosed with blood tests (checking for M-proteins), bone marrow biopsy, and imaging tests. Treatment options include targeted therapy, steroids, and bone-strengthening medications.
By understanding these key differences, healthcare providers can tailor treatment plans to address the unique challenges posed by each type of blood cancer.
Symptoms to Watch For
OvBlood cancers often present with overlapping and distinct symptoms, reflecting the broad impact they have on the body. Early recognition of these signs is essential for timely diagnosis and intervention, which can significantly improve outcomes.
Overlapping Symptoms of Blood Cancers
Many blood cancers share common symptoms due to their effects on blood cell production, immune function, and overall body health. These include:
- Fatigue: Persistent and unexplained tiredness, often severe enough to interfere with daily activities and not relieved by rest.
- Fever: Recurring or unexplained fevers caused by a weakened immune system struggling to fight infections.
- Weight Loss: Unintended and noticeable weight loss without changes in diet or physical activity.
- Night Sweats: Profuse sweating during the night, often soaking clothes or bedding, and unrelated to room temperature or physical activity.
Specific Symptoms for Each Type of Blood Cancer
Each type of blood cancer affects the body in unique ways, leading to specific symptoms:
Leukemia
- Frequent Infections and Slow Healing Wounds: Due to a lack of healthy white blood cells, the body becomes more vulnerable to infections and struggles to heal wounds.
- Easy Bruising or Excessive Bleeding: Low platelet counts impair the blood’s ability to clot, leading to prolonged bleeding from minor injuries or spontaneous bruising.
- Bone Pain or Tenderness: Often felt in larger bones like the legs or hips, caused by the overproduction of abnormal cells in the bone marrow.
Lymphoma
- Painless Swelling of Lymph Nodes: Particularly noticeable in the neck, armpits, or groin, these swellings are a hallmark sign of lymphoma.
- Persistent Cough or Difficulty Breathing: If lymph nodes in the chest are enlarged, they can press on the lungs or airways.
- Generalized Itching: Often without a visible rash or other apparent cause, this can be a symptom of Hodgkin lymphoma.
Myeloma
- Bone Pain: Especially in the back or ribs, this pain can be severe and often leads to fractures due to bone weakening.
- Frequent Infections: Myeloma impairs antibody production, making the body more susceptible to recurring infections.
- Symptoms of Kidney Damage: Signs include excessive thirst, frequent urination, and swelling in the legs or feet, caused by protein buildup affecting kidney function.
Why Early Recognition Matters
Blood cancer symptoms can often be mistaken for less serious conditions, leading to delayed diagnosis. Recognizing these signs, especially if they persist or worsen over time, is crucial. Individuals experiencing these symptoms should consult a healthcare provider promptly for evaluation and potential testing. Early detection not only improves treatment outcomes but can also save lives.
Diagnosis and Treatment
Understanding the diagnostic processes and treatment options for leukemia, lymphoma, and myeloma is essential for timely and effective care.
Diagnostic Methods
- Blood Tests:
Routine blood tests can identify abnormalities in blood cell counts, which may signal leukemia or myeloma. Specialized tests like flow cytometry can further pinpoint specific cancer markers. - Biopsies:
A bone marrow biopsy is commonly used for leukemia and myeloma, while a lymph node biopsy is often performed for suspected lymphoma cases. These procedures confirm the presence and type of cancer. - Imaging Techniques:
Scans such as CT, MRI, or PET are used to detect the spread of lymphoma or complications from myeloma, such as bone damage.
General Treatment Approaches
- Chemotherapy:
- A cornerstone for all three cancers, chemotherapy targets rapidly dividing cancer cells, either alone or in combination with other treatments.
- Immunotherapy:
- This approach boosts the immune system to recognize and attack cancer cells. It’s especially promising for lymphoma and some leukemia types.
- Stem Cell Transplants:
- Used to replace damaged bone marrow, particularly in severe cases of leukemia and myeloma.
- Targeted Therapy:
- Medications designed to attack specific cancer-causing molecules, such as tyrosine kinase inhibitors for certain leukemias.
- Radiation Therapy:
- Often used for localized lymphoma or as part of a combination treatment strategy.
By combining advanced diagnostics and tailored treatment plans, healthcare providers can improve outcomes and quality of life for those affected by blood cancers.
FAQs About Blood Cancers
What Causes These Blood Cancers?
Blood cancers such as leukemia, lymphoma, and myeloma develop due to genetic mutations in blood cells. While the exact causes are not always clear, contributing factors may include:
- Genetic predisposition: A family history of blood cancers increases risk.
- Exposure to toxins: Chemicals like benzene or radiation exposure can trigger mutations.
- Immune system dysfunction: Weakened immunity or autoimmune diseases may contribute to blood cancers.
- Infections: Certain viruses, such as Epstein-Barr or HIV, are linked to lymphoma.
Can These Cancers Be Cured?
The potential for a cure depends on the type and stage of the cancer:
- Leukemia: Acute leukemias may be curable with aggressive treatments like chemotherapy or stem cell transplants, while chronic leukemias are typically managed rather than cured.
- Lymphoma: Hodgkin lymphoma has high cure rates with modern therapies, whereas non-Hodgkin lymphoma outcomes vary by subtype.
- Myeloma: While a cure for myeloma is not currently available, advancements in treatment have significantly extended survival rates and improved quality of life.
How Do Lifestyle Factors Impact Treatment Outcomes?
Lifestyle choices play a crucial role in supporting recovery and managing side effects:
- Healthy Diet: A nutrient-rich diet boosts immunity and helps the body tolerate treatments better.
- Regular Exercise: Moderate physical activity can reduce fatigue and improve overall well-being.
- Avoiding Toxins: Quitting smoking and limiting alcohol can help improve treatment efficacy.
- Stress Management: Practices like meditation or counseling can enhance mental health, which is essential for a positive treatment journey.
Taking proactive steps alongside medical care can greatly influence outcomes and quality of life for individuals battling blood cancers.
Conclusion
Understanding the differences between leukemia, lymphoma, and myeloma is essential for recognizing symptoms, seeking timely medical care, and navigating potential diagnoses. While these three blood cancers share similarities—such as their impact on the blood, bone marrow, or lymphatic system—they differ significantly in origin, symptoms, and treatment approaches. Knowing these distinctions can empower individuals and their loved ones to make informed decisions about their health.
If you or someone you know is experiencing unexplained symptoms like fatigue, persistent fever, weight loss, or unusual pain, it’s crucial to consult a healthcare specialist. Early diagnosis can dramatically improve treatment outcomes, offering a greater chance of remission and better quality of life. Specialists can also guide you through the best diagnostic methods, such as blood tests, imaging, and biopsies, tailored to your situation.
Finally, early diagnosis and a robust support system are vital for managing these challenging conditions. Whether it’s understanding treatment options, connecting with support groups, or maintaining a healthy lifestyle, taking proactive steps can make a significant difference. Remember, knowledge is power—stay informed, prioritize your health, and lean on your medical team for guidance and support.


1 thought on “How to Tell the Difference Between Leukemia Lymphoma and Myeloma”