Monkeypox is a viral disease that has captured global attention due to its concerning symptoms and potential for spread. Initially discovered in 1958 in monkeys, the first human case was recorded in 1970. The disease is caused by the Monkeypox virus, a member of the Orthopoxvirus genus in the family Poxviridae, which also includes the variola virus known for causing smallpox.
Recent Statistics and Geographical Spread
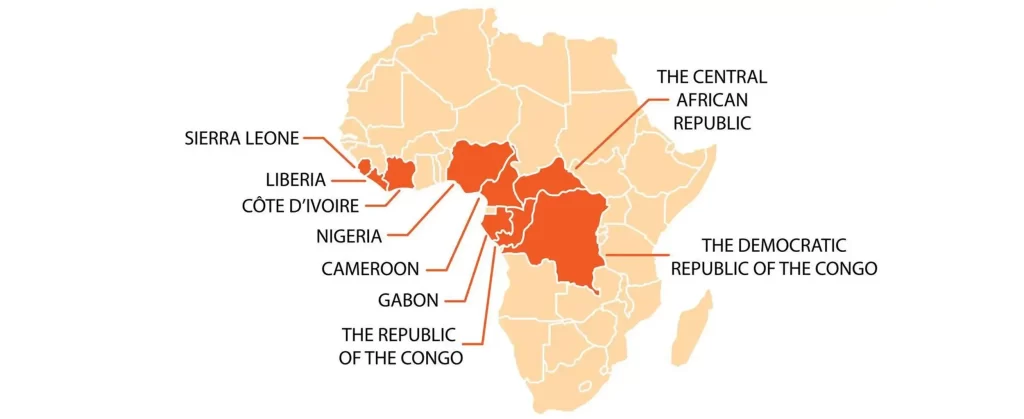
As of the latest updates, there have been significant outbreaks of Monkeypox across various continents including Africa, Europe, and the Americas. The disease has transitioned from being primarily confined to remote areas in Central and West Africa to affecting major cities around the world. In 2022, over 100,000 cases were reported globally, marking it as a year of unprecedented spread. The number of reported cases continues to fluctuate, with public health efforts aimed at controlling the outbreaks through surveillance, vaccination, and patient care.
Importance of Accurate Information
In the face of any disease outbreak, accurate information is critical. Misinformation can lead to panic, stigmatization, and the implementation of ineffective public health measures. It is essential for media outlets, health organizations, and government bodies to provide clear, factual, and timely information to the public. Educating people about the modes of transmission, symptoms, and preventive measures for Monkeypox helps in reducing unnecessary fear and promoting effective actions to manage the spread of the virus.
Understanding Monkeypox is crucial not only for those in the medical field but also for the general public to ensure a coordinated and effective response to control the disease’s impact. As we continue to gather data and research on Monkeypox, staying informed through reliable sources and adhering to recommended practices is our best defense against the spread of this disease.

What is Monkeypox?
Definition and Background
Monkeypox is a zoonotic virus, meaning it originates from animals and can be transmitted to humans. It is part of the Orthopoxvirus genus, which also includes the variola virus responsible for smallpox. The name “Monkeypox” derives from its initial discovery in laboratory monkeys in 1958, though rodents are believed to be the primary animal reservoir. The first human case was identified in the Democratic Republic of the Congo in 1970, during a period when intensified efforts were underway to eliminate smallpox.
How It Differs from Other Pox Viruses
While Monkeypox is similar to smallpox, it is generally less severe and has a lower mortality rate. Unlike smallpox, which has been eradicated, Monkeypox still causes sporadic outbreaks. The Monkeypox virus exhibits a distinct difference in its reservoir hosts; while smallpox was transmitted human-to-human, Monkeypox primarily spreads from animals to humans, with secondary human-to-human transmission through close contact. Additionally, Monkeypox causes lymphadenopathy (swelling of the lymph nodes), which is not a feature of smallpox, helping clinicians distinguish between the two diseases.
Symptoms and Diagnosis
The symptoms of Monkeypox typically begin with fever, headache, muscle aches, and exhaustion. Within 1 to 3 days after the appearance of fever, the patient develops a rash, often beginning on the face then spreading to other parts of the body. The rash progresses through several stages, including scabs, before healing. The illness usually lasts for 2-4 weeks. Diagnosis is based on the recognition of the rash and confirmed through laboratory tests that identify the virus in skin lesions, body fluids, or scabs. Differential diagnosis is crucial as it helps differentiate Monkeypox from other rash illnesses such as chickenpox, measles, or bacterial skin infections.
Global Health Emergency Declaration
Explanation of What a Global Health Emergency Means
A global health emergency, officially termed a “Public Health Emergency of International Concern” (PHEIC), is declared by the World Health Organization (WHO) when a health issue poses serious health risks to multiple countries and requires a coordinated international response. This declaration is intended to draw global attention, mobilize resources, and foster international cooperation to prevent and reduce the spread of diseases like Monkeypox.
WHO’s Stance and Recommendations on Monkeypox
In response to the increasing cases of Monkeypox across different continents, the WHO has recognized the outbreak as a global health emergency. The organization emphasizes the need for countries to enhance surveillance, share data, and work together on containment strategies. WHO recommends targeted vaccinations for high-risk populations, including healthcare workers and close contacts of Monkeypox patients, along with public education campaigns to raise awareness about the modes of transmission and preventive practices.
Impact of Such Declarations on Public Perception and Policy
The declaration of a global health emergency significantly impacts public perception and policy. It often leads to increased media coverage and public attention, which, if not managed carefully, can result in panic or stigmatization. However, this heightened awareness also drives governmental and non-governmental bodies to allocate necessary resources for research, healthcare, and preventive measures. Policies may include travel advisories, health screenings at ports of entry, and the implementation of quarantine measures to prevent the spread of the virus. These efforts are crucial in shaping the global response and in mitigating the impact of the outbreak.
Transmission of Monkeypox
Detailed Look at How Monkeypox Spreads Among People
Monkeypox primarily spreads through close, personal, often skin-to-skin contact with an infected individual. This includes direct contact with the rash, scabs, or body fluids, as well as respiratory droplets during prolonged face-to-face interaction. The virus can also be transmitted by touching items (like clothing or bedding) that previously touched the infectious rash or body fluids. Additionally, it’s possible, though less common, for Monkeypox to spread via droplet respiratory particles during prolonged exposure to infected individuals.
Comparison with Other Viruses (e.g., COVID-19)
Unlike COVID-19, which is highly contagious and primarily transmitted through airborne particles and droplets from coughing or sneezing, Monkeypox requires much closer physical contact for transmission. COVID-19 can be spread by asymptomatic individuals, making it more difficult to control. In contrast, Monkeypox is most contagious when symptoms are present, particularly from the rash, which is not a symptom of COVID-19. This makes targeted interventions more effective for Monkeypox, as symptomatic individuals can be isolated more straightforwardly.
Preventive Measures to Curb Spread
To prevent the spread of Monkeypox, it’s essential to:
- Isolate infected individuals: Those with symptoms should stay away from others until fully recovered.
- Practice good hygiene: Regular hand washing with soap and water or using alcohol-based hand sanitizers can reduce the risk of transmission.
- Use personal protective equipment (PPE): Healthcare workers and caregivers should use appropriate PPE, including gloves and masks, when dealing with infected individuals.
- Educate the public: Awareness campaigns can help people recognize the symptoms of Monkeypox and understand how to respond if they suspect an infection.
- Vaccination: Vaccines used for smallpox have been shown to be about 85% effective in preventing Monkeypox, recommended for high-risk groups such as health workers and those in close contact with the infected.
Historical Context and Recent Outbreaks of Monkeypox
A Brief History of Monkeypox Outbreaks
Monkeypox was first identified in humans in 1970 in the Democratic Republic of Congo (DRC) during efforts to eliminate smallpox. Since then, the virus has primarily been confined to rainforest regions of Central and West Africa, where it sporadically causes outbreaks. The natural reservoirs, believed to be rodents, facilitate the virus’s spread in rural communities. Prior to the 2000s, Monkeypox was relatively unknown outside of Africa, with few cases reported and generally contained locally.
Statistics from the 2022 and 2023 Outbreaks
The global landscape of Monkeypox changed dramatically in 2022 when outbreaks occurred in several non-endemic countries, prompting global health concerns. Over 100,000 cases were reported globally, marking a significant departure from its usual geographical containment. The 2023 outbreaks followed, with thousands of cases continuing to emerge across various continents, facilitated by international travel and greater awareness of the disease’s symptoms, which likely contributed to higher reporting rates.
Lessons Learned from Past Responses
Each outbreak of Monkeypox has offered valuable lessons for global health governance. Key takeaways include:
- Surveillance and Early Detection: Enhanced surveillance systems in endemic and non-endemic regions have proven essential. Early detection allows for quicker containment and management efforts.
- Public Health Education: Educating communities about transmission vectors and protective measures can significantly reduce the spread. Information dissemination must be clear and accessible to prevent misinformation.
- International Collaboration: Global health emergencies like Monkeypox require international cooperation. Sharing data, resources, and strategies across borders enhances the overall response efficiency.
- Vaccination Strategy: Leveraging existing smallpox vaccines has been beneficial. A targeted vaccination approach for high-risk groups and healthcare workers helps curb outbreaks effectively.
These lessons underline the importance of preparedness, community engagement, and adaptive response strategies in managing health crises.
Monkeypox Strains and Their Implications
Discussion of Different Monkeypox Strains
Monkeypox virus has two primary strains: the Central African (Congo Basin) strain and the West African strain. The Central African strain is more severe and has a higher mortality rate, with fatality rates historically up to 10%. In contrast, the West African strain, which has been more commonly identified in the recent global outbreaks, has a lower fatality rate of around 1%. These strains not only differ in severity but also in their geographical spread and potential for causing large outbreaks.

Severity and Fatality Rates of These Strains
The difference in severity between the two strains of Monkeypox can largely influence the public health response and perception of risk. The Central African strain requires more stringent control measures due to its higher severity and fatality rate. Public health officials often prioritize vaccine and medical resource allocation to areas predominantly affected by this strain. On the other hand, the West African strain, while less severe, requires vigilant surveillance due to its potential for wider spread, as seen in the recent outbreaks in non-endemic countries.
Research and Developments on Strain Mutations
Ongoing research into Monkeypox focuses on understanding how these strains mutate and spread among populations. Studies are examining the genetic evolution of the virus to predict future outbreak patterns and assess the risk of more virulent strains emerging. This research is crucial for developing effective vaccines and treatments that can address not just current strains but also potential future mutations. Additionally, understanding strain mutations helps in developing diagnostic tools that can quickly and accurately detect different strains during outbreaks, enhancing response efforts.
Case Studies: Handling Monkeypox Globally
How Different Countries Have Managed Outbreaks
The global response to Monkeypox has varied, with different strategies implemented based on the local context and the specific strain involved. For instance, in the Democratic Republic of Congo, where Monkeypox has been endemic for decades, ongoing surveillance and community education have been key components of the public health approach. In contrast, in 2022, when multiple non-endemic countries, including the United States and several European nations, experienced outbreaks, strategies focused more on isolation of cases, contact tracing, and targeted vaccination campaigns, especially among high-risk groups.
Success Stories and Challenges Faced
A notable success story in managing Monkeypox outbreaks is Nigeria, which experienced a significant outbreak in 2017. The country’s swift response, involving rapid isolation of patients, extensive contact tracing, and community engagement campaigns, helped contain the spread significantly. On the other hand, challenges remain, such as in rural areas of Central Africa where limited healthcare infrastructure complicates efforts to manage and contain outbreaks. Additionally, global disparities in vaccine access and distribution have posed challenges for equitable health interventions.
Role of International Cooperation
International cooperation has been pivotal in handling Monkeypox outbreaks. Organizations like the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) have played critical roles in coordinating responses, sharing information, and providing resources. For instance, during the 2022 outbreak, the WHO facilitated meetings and shared up-to-date research and guidelines with health ministries globally. Such cooperation ensures that knowledge and resources are shared, which is crucial for developing strategies that limit the spread of infections and mitigate their impact.
Medical Response to Monkeypox
Current Treatments and Vaccines Available
As part of the medical response to Monkeypox, several treatments and vaccines have been adapted from those developed for smallpox, given the similarities between the two viruses. Antiviral medications such as Tecovirimat (TPOXX) have been approved for the treatment of Monkeypox. This medication has shown efficacy in reducing symptoms and shortening the duration of the illness. For prevention, vaccines like JYNNEOS (also known as Imvamune or Imvanex) have been authorized for use against Monkeypox. These vaccines are primarily recommended for healthcare workers, lab personnel, and individuals at high risk of exposure.

Ongoing Research and Clinical Trials
Research into Monkeypox is actively ongoing, with numerous clinical trials underway to find more effective treatments and to understand the long-term efficacy of vaccines. Scientists are exploring the genetic evolution of the virus to anticipate possible future changes that could affect its spread and virulence. Research is also focused on developing better diagnostic tools that can quickly and accurately detect the virus, facilitating faster response and containment measures.
Accessibility of Medical Resources
The accessibility of medical resources for managing Monkeypox varies globally. In many Western countries, strategic stockpiles of vaccines and antivirals have been established, ensuring a relatively quick deployment during outbreaks. However, in endemic regions, such as parts of Central and West Africa, access to these medical resources can be limited. International health organizations are working to improve the distribution of vaccines and treatments to these areas, emphasizing the need for equity in health resource allocation to prevent widespread transmission.
Public Health Strategies for Managing Monkeypox
Prevention Campaigns and Public Education
Effective public health strategies begin with robust prevention campaigns and public education efforts. For Monkeypox, these campaigns focus on informing the public about how the virus is transmitted and the importance of hygiene practices such as regular hand washing and avoiding close contact with infected individuals. Educational materials often include guidelines on recognizing symptoms and the necessary steps to take if one suspects they have contracted the virus. Health departments also use social media, posters, community meetings, and broadcasts to disseminate this crucial information widely.
Contact Tracing and Containment Efforts
Contact tracing is a critical component in containing Monkeypox outbreaks. Once a case is identified, health officials work to trace and monitor everyone who may have been in contact with the infected individual. This process helps to prevent further transmission by ensuring that those exposed are aware and can take precautions, such as self-isolating. Containment efforts also include setting up specialized treatment centers and isolation zones to manage and treat confirmed cases without putting the broader population at risk.
Importance of Community Engagement
Community engagement is vital for the success of public health initiatives, especially in managing outbreaks like Monkeypox. By involving local leaders, community organizations, and volunteers, health authorities can enhance their outreach and ensure that messages are culturally appropriate and well-received. Community-driven efforts are often more effective because they are based on a deep understanding of local contexts and can address specific community needs and concerns. Such engagement also helps in reducing stigma associated with the disease, encouraging more people to come forward and seek medical help early.
Monkeypox vs. COVID-19: A Comparative Analysis
Direct Comparison of Transmission, Symptoms, and Impact
While both Monkeypox and COVID-19 are infectious diseases caused by viruses, their modes of transmission differ significantly. Monkeypox spreads primarily through close contact with infected individuals or contaminated materials, requiring direct interaction with bodily fluids or lesion material. In contrast, COVID-19 is predominantly transmitted via airborne particles and droplets, making it far more contagious in various settings. Symptomatically, Monkeypox is characterized by rash, fever, and lymphadenopathy, whereas COVID-19 symptoms include fever, cough, and respiratory difficulties. The impacts of these viruses also differ; COVID-19 has had a global impact, affecting millions and causing significant mortality, while Monkeypox, though serious, has led to fewer infections and deaths globally.
Public and Health System Responses to Both Viruses
The responses to Monkeypox and COVID-19 have highlighted the flexibility and challenges of health systems worldwide. For COVID-19, governments implemented widespread lockdowns, travel bans, and mass vaccination campaigns. The rapid development and rollout of vaccines were critical in managing the pandemic. For Monkeypox, the response has been more targeted, focusing on high-risk groups and utilizing existing smallpox vaccines for prevention. Contact tracing and isolation have been the primary strategies, without the large-scale societal lockdowns seen during the COVID-19 pandemic.
Societal Impact and Media Coverage
The societal impacts of COVID-19 have been profound, affecting every aspect of life, from economic downturns to changes in daily behaviors and long-term social norms. Monkeypox, while serious, has not precipitated the same level of societal or global disruption. Media coverage of COVID-19 has been extensive, often dominating headlines for months on end, whereas Monkeypox has received more sporadic attention, focused mainly during outbreaks or in regions experiencing a higher number of cases.
Addressing the Panic: Rational Approach to Monkeypox
Understanding the Statistical Risks
Monkeypox, while a concern, poses a relatively low statistical risk of widespread transmission compared to more contagious diseases like influenza or COVID-19. It is primarily spread through close contact with the lesions, body fluids, or respiratory droplets of an infected person, or through contaminated materials. Statistically, the global case fatality rate has been relatively low, varying from under 1% to around 10% in poorer healthcare settings, primarily associated with the more virulent strain of the virus.
Misconceptions and Myths Debunked
Many myths and misconceptions about Monkeypox contribute to unnecessary panic and stigma. Contrary to some beliefs, Monkeypox is not as easily transmissible as airborne viruses like COVID-19. It requires close physical contact for transmission, which means it is less likely to cause large-scale outbreaks. Another common misconception is that Monkeypox only affects certain demographic or geographic groups; in reality, anyone who comes into contact with the virus can contract it, regardless of age, gender, or location. Debunking these myths is crucial for preventing panic and encouraging the appropriate public health response.
Expert Opinions and Advice
Health experts emphasize the importance of staying informed through credible sources and adhering to public health advisories. They advise maintaining good hygiene, minimizing close contact with individuals who have symptoms of Monkeypox, and seeking medical attention early if symptoms develop. Vaccination is recommended for healthcare workers and others at high risk of exposure. Experts also stress the need for calm and rational response from the public and policymakers, based on scientific evidence and best practices in disease control.
By understanding the actual risks, dispelling myths, and following expert advice, communities can effectively manage their response to Monkeypox without undue panic.
Conclusion
As we conclude our exploration of Monkeypox, it’s important to recap the key points we’ve discussed and consider how we can respond effectively to this public health concern.
Recap of Key Points:
- Transmission and Symptoms: Monkeypox spreads primarily through close contact with infected individuals or contaminated materials, with symptoms including rash, fever, and lymph node swelling.
- Global Response and Vaccination: Effective public health strategies, including vaccination and contact tracing, have been implemented to manage outbreaks.
- Debunking Myths: It’s crucial to dispel common myths about Monkeypox, understanding that it is less contagious than airborne viruses and affects people regardless of geography or demographics.
Encouragement for Informed Actions and Calm: Staying informed through credible sources and understanding the real risks associated with Monkeypox are essential. Panic can be mitigated through knowledge and practical measures such as maintaining hygiene and seeking medical advice when necessary. Communities are encouraged to rely on guidance from health authorities and not succumb to misinformation.
Further Resources and Links for More Information: For those looking to delve deeper into the subject of Monkeypox or stay updated with the latest research and guidelines, here are some valuable resources:
- World Health Organization (WHO) – Monkeypox
- Centers for Disease Control and Prevention (CDC) – About Monkeypox
- National Health Service (NHS) – Monkeypox
By approaching Monkeypox with a rational and informed perspective, we can collectively ensure a calm and effective response to its challenges.
Ressources
World Health Organization (WHO): Provides comprehensive information on Monkeypox, including global outbreak updates, prevention strategies, and public health advice.
Centers for Disease Control and Prevention (CDC): Offers detailed guidance on the diagnosis, treatment, and prevention of Monkeypox, as well as statistics on its spread in the United States and globally.
National Health Service (NHS): Provides information about Monkeypox symptoms, how it’s spread, and advice on what to do if you think you have it, tailored for the UK audience.
European Centre for Disease Prevention and Control (ECDC): Offers updates on the current situation of Monkeypox in Europe, including risk assessments and control measures.
Public Health England (PHE) – Health Matters: Offers educational resources and updates on Monkeypox for health professionals and the general public.
