That quiet, chilling question—”Is cancer simply bad luck?”—often arises from a place of deep unease. It speaks to a feeling of powerlessness, as if our health hinges on a cosmic coin toss. This belief, while understandable, can leave us paralyzed, overlooking the significant agency we actually hold.
Modern science offers a more nuanced and ultimately more empowering perspective. Research confirms that while random cellular errors occur, they are just one piece of a complex puzzle. The most compelling evidence points to the profound influence of our daily choices on our body’s internal environment, or “inner terrain,” which can either resist or support disease development.
This article will explore this evidence, separating myth from fact. You will leave with a clearer understanding of where true risk lies and a practical, science-informed framework for building resilience. Our goal is not to promise control over chance, but to empower you with knowledge, moving you from anxiety to actionable understanding.
The “Bad Luck” Study: A Headline That Missed the Full Picture
The provocative idea that cancer is predominantly “bad luck” entered the public consciousness following a influential 2015 study published in the journal Science by researchers Tomasetti and Vogelstein. Their analysis sought to answer why some tissues in the body (like the colon or pancreas) are more prone to cancer than others (like bone or brain).
The core finding was a statistical correlation: they observed that the lifetime risk of cancer in a given tissue often aligned with the total number of times that tissue’s stem cells had divided throughout a person’s life. Simply put, tissues with cells that naturally regenerate more frequently—a biological necessity for organs like the gut or skin—had a higher observed baseline rate of cancer. This led to the conclusion that a portion of cancer risk is attributable to the random errors that inevitably occur during DNA replication in these countless cell divisions. These are the unavoidable “rolls of the genetic dice.”
What “Random Mutations” Really Mean)
This finding highlights a fundamental biological truth: our bodies are not perfect machines. Every time a single cell divides to make two, it must copy its entire genome—over 3 billion DNA letters. Errors, or mutations, are a natural byproduct of this immensely complex process. Some of these random mutations can occur in genes that regulate cell growth, potentially providing the first “spark” toward cancer.
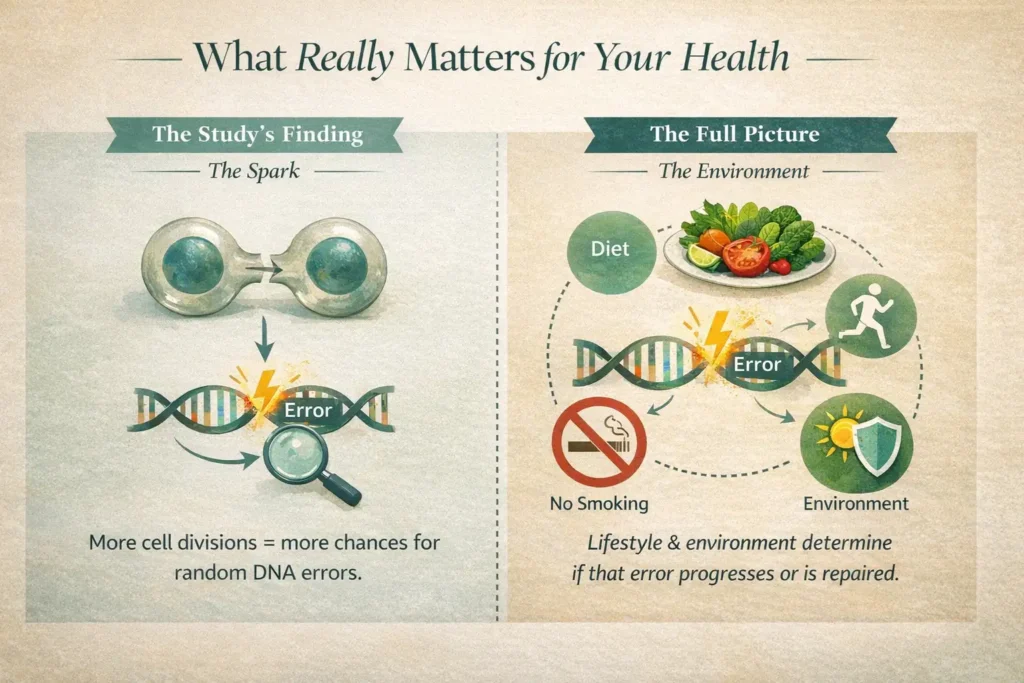
However, and this is the critical nuance that headlines often missed, the study did not claim that two-thirds of cancers are solely due to fate. The researchers were specifically analyzing variation in risk between different tissue types, not the causes of cancer overall. They explicitly stated that their model did not account for the powerful effects of known external risk factors.
The misinterpretation was profound. The study illuminated the source of the initial “spark” (random errors during cell division). But whether that isolated spark dies out or ignites into a sustained “fire” of a tumor is decisively influenced by the “environment” it lands in—an environment shaped by your lifestyle, diet, immune health, and exposures. A random error in a lung cell is far more likely to progress in a smoker’s inflamed lung tissue than in the resilient tissue of a non-smoker. The study described the potential for a spark; our daily lives determine the tinder.
Why “Bad Luck” is an Incomplete (and Unhelpful) Answer
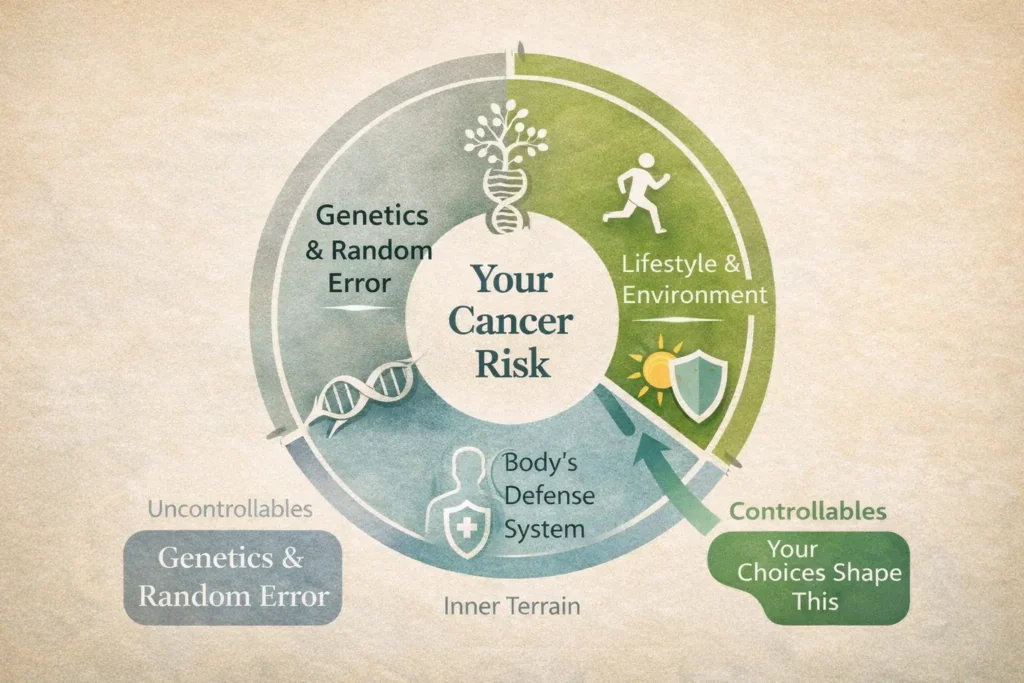
While the “bad luck” theory provides a neat, albeit unsettling, explanation, clinging to it can be psychologically and practically disempowering. It can lead to a fatalistic mindset where proactive health feels pointless, or conversely, to unnecessary guilt in those who develop cancer despite healthy habits. A more accurate and useful model recognizes that cancer risk is not a monolith but a tapestry woven from three distinct threads, each with a different level of personal influence.
1. The Uncontrollables: Genetics and Random Errors
This is the domain of pure “luck.” It encompasses the genetic blueprint you inherited—including any higher-risk variants like BRCA mutations—and the random DNA copying errors that occur in every single person as a normal part of cellular aging and renewal. We have no control over these factors. However, understanding them is not about surrendering to fate; it’s about informed vigilance. Knowing your family history empowers you to have targeted conversations with your doctor about potentially earlier or more frequent screenings, turning passive risk into an active surveillance plan.
2. The Controllables: Your Lifestyle and Environment
This is where your direct, daily agency resides. Decades of epidemiological research have consistently identified powerful external levers we can pull:
- Diet: Patterns matter most. A diet consistently high in processed meats, sugary drinks, and refined carbohydrates, while low in fibre, antioxidants, and phytonutrients from diverse fruits and vegetables, creates a metabolic environment that can promote cancer development.
- Substances: Tobacco smoke is the single greatest avoidable carcinogen, implicated in numerous cancers beyond the lung. Alcohol consumption, even in moderation, is a known risk factor for several cancer types.
- Environment: Exposure to certain environmental pollutants, industrial chemicals, and excessive radiation (like UV from the sun) contributes to the mutational load your body must manage.
- Infections: Viruses like HPV (cervical, head/neck cancers) and Hepatitis B/C (liver cancer), and bacteria like H. pylori (stomach cancer) are responsible for a significant percentage of global cancers. Vaccination and treatment represent powerful, straightforward prevention tools.
3. The “Inner Terrain”: Your Body’s Defense System
This is the crucial, dynamic interface where the “Uncontrollables” and “Controllables” meet. Your “inner terrain” is the physiological milieu within your body—its internal ecology. This terrain is decisively shaped by your lifestyle choices and determines whether a random mutation is swiftly dealt with or allowed to progress. Its key components include:
Cellular Repair Mechanisms: Your body’s innate ability to detect and repair DNA damage before it becomes a fixed mutation.
Immune Surveillance: The efficacy of your immune system in recognizing and eliminating precancerous and cancerous cells.
Chronic Inflammation: A persistent, low-grade inflammatory state (often driven by poor diet, obesity, or stress) acts as fertilizer for cancer growth, damaging cells and promoting proliferation.
Hormonal Balance: Hormones like estrogen and insulin can influence the growth of certain cancers. Diet, body fat percentage, and physical activity are primary modulators of these hormones.
Think of it this way: The “Uncontrollables” provide the initial seed (a random genetic error). Your “Controllables” (lifestyle) determine the quality of the soil (your inner terrain). You cannot control which seeds blow into your garden, but you can absolutely decide whether to nurture that garden with rich soil, sunlight, and water, or to neglect it. A healthy lifestyle cultivates a resilient, inhospitable terrain where errant seeds struggle to take root.
Your Path from Fear to Empowerment: Practical Steps
Moving from anxiety about cancer to a sense of grounded agency requires shifting your focus from the vast unknown to the tangible, evidence-based actions within your control. This is not about achieving perfection or guaranteeing a specific outcome; it’s about consistently stacking the odds in your favor by building a resilient biology. Here is a practical, actionable framework to begin.
1. Nourish for Resilience: Build Your Dietary Foundation
Think of food as information and fuel for your cells. Aim to build a “protective plate” at most meals.
- The “Half-Plate” Rule: Visually, aim for half your plate to be filled with a variety of colorful non-starchy vegetables and fruits. Different colors provide different protective phytochemicals (e.g., lycopene in tomatoes, anthocyanins in berries, sulforaphane in broccoli).
- Prioritize Plant-Based Protein: Integrate legumes (beans, lentils, chickpeas), nuts, and seeds as protein sources. They provide fiber, which feeds a healthy gut microbiome linked to improved immune function and reduced inflammation.
- Choose Smart Carbs: Opt for whole grains (like oats, quinoa, brown rice) over refined grains (white bread, pasta). They have a gentler impact on blood sugar and insulin levels.
- Reframe Your Mindset: Instead of fixating on cutting out “bad” foods, focus on crowding them out by adding more of the good. When you fill up on nutrient-dense, satisfying whole foods, there’s naturally less room and desire for ultra-processed options.
2. Move Your Body Regularly: Make Activity a Non-Negotiable
Physical activity is one of the most potent modulators of your “inner terrain.” You don’t need to train for a marathon.
- The Consistent Baseline: Aim for at least 150 minutes of moderate-intensity activity per week (e.g., brisk walking, cycling, swimming). This can be broken into manageable 30-minute sessions, five days a week.
- Incorporate Strength: Include muscle-strengthening activities (weight training, resistance bands, bodyweight exercises) at least twice a week. Muscle mass is metabolically active and helps regulate hormones and blood sugar.
- The “Why”: Regular movement lowers chronic inflammation, improves insulin sensitivity, aids in healthy weight maintenance, and enhances immune cell circulation. It’s like regularly tuning up your body’s surveillance and defense systems.
3. Be Mindful of Exposures: Your Daily Dose of Prevention
This is about conscious risk reduction in your immediate environment.
- Tobacco: The Single Best Change: If you smoke, quitting is the most powerful health decision you can make. Seek support—counseling, apps, medication—it’s a process, not a test of willpower.
- Alcohol: Less is More: Follow guidelines for low-risk drinking. Consider practicing mindful drinking: opting for smaller servings, having alcohol-free days each week, and never using alcohol to cope with stress.
- Environmental Awareness: Be practical. Use sunscreen consistently to prevent UV radiation damage. Ventilate your home when using cleaning products. Check local advisories for air quality and limit intense outdoor activity on poor days. When possible, choose products with simpler ingredient lists.
4. Partner with Your Healthcare Team: Empowerment is a Collaboration
True empowerment recognizes that you are the CEO of your health, but you need a trusted board of advisors.
Communicate Openly: Come to appointments with questions. If a recommendation doesn’t feel right, ask for the reasoning behind it. A good healthcare partnership is built on dialogue and mutual respect, ensuring you are an active participant in every decision.
Screenings: Your Early-Detection Advantage: View recommended screenings (mammograms, colonoscopies, Pap smears, skin checks) not as scary obligations, but as your most powerful tools for catching potential issues at their earliest, most treatable stages. Schedule them and keep the appointments.
Know and Share Your History: Create a simple family health history. Knowing if a parent, sibling, or child had cancer (and at what age) provides crucial context for your doctor to personalize your care plan.
Building a Deeper Understanding: Your Next Step
While the “bad luck” theory provides a neat, albeit unsettling, explanation, clinging to it can be psychologically and practically disempowering. It can lead to a fatalistic mindset where proactive health feels pointless, or conversely, to unnecessary guilt in those who develop cancer despite healthy habits. A more accurate and useful model recognizes that cancer risk is not a monolith but a tapestry woven from three distinct threads, each with a different level of personal influence.
1. The Uncontrollables: Genetics and Random Errors
This is the domain of pure “luck.” It encompasses the genetic blueprint you inherited—including any higher-risk variants like BRCA mutations—and the random DNA copying errors that occur in every single person as a normal part of cellular aging and renewal. We have no control over these factors. However, understanding them is not about surrendering to fate; it’s about informed vigilance. Knowing your family history empowers you to have targeted conversations with your doctor about potentially earlier or more frequent screenings, turning passive risk into an active surveillance plan.
2. The Controllables: Your Lifestyle and Environment
This is where your direct, daily agency resides. Decades of epidemiological research have consistently identified powerful external levers we can pull:
- Diet: Patterns matter most. A diet consistently high in processed meats, sugary drinks, and refined carbohydrates, while low in fibre, antioxidants, and phytonutrients from diverse fruits and vegetables, creates a metabolic environment that can promote cancer development.
- Substances: Tobacco smoke is the single greatest avoidable carcinogen, implicated in numerous cancers beyond the lung. Alcohol consumption, even in moderation, is a known risk factor for several cancer types.
- Environment: Exposure to certain environmental pollutants, industrial chemicals, and excessive radiation (like UV from the sun) contributes to the mutational load your body must manage.
- Infections: Viruses like HPV (cervical, head/neck cancers) and Hepatitis B/C (liver cancer), and bacteria like H. pylori (stomach cancer) are responsible for a significant percentage of global cancers. Vaccination and treatment represent powerful, straightforward prevention tools.
3. The “Inner Terrain”: Your Body’s Defense System
This is the crucial, dynamic interface where the “Uncontrollables” and “Controllables” meet. Your “inner terrain” is the physiological milieu within your body—its internal ecology. This terrain is decisively shaped by your lifestyle choices and determines whether a random mutation is swiftly dealt with or allowed to progress. Its key components include:
- Immune Surveillance: The efficacy of your immune system in recognizing and eliminating precancerous and cancerous cells.
- Chronic Inflammation: A persistent, low-grade inflammatory state (often driven by poor diet, obesity, or stress) acts as fertilizer for cancer growth, damaging cells and promoting proliferation.
- Hormonal Balance: Hormones like estrogen and insulin can influence the growth of certain cancers. Diet, body fat percentage, and physical activity are primary modulators of these hormones.
- Cellular Repair Mechanisms: Your body’s innate ability to detect and repair DNA damage before it becomes a fixed mutation.
Think of it this way: The “Uncontrollables” provide the initial seed (a random genetic error). Your “Controllables” (lifestyle) determine the quality of the soil (your inner terrain). You cannot control which seeds blow into your garden, but you can absolutely decide whether to nurture that garden with rich soil, sunlight, and water, or to neglect it. A healthy lifestyle cultivates a resilient, inhospitable terrain where errant seeds struggle to take root.
Conclusion: Is Cancer Simply Bad Luck? From Powerless to Proactive
Cancer is not simply bad luck. It is a complex interplay of the random, the inherited, and the lived. While we cannot control every roll of the genetic dice, we have immense power over the environment in which those dice are cast—our own bodies.
Let go of the disempowering myth of pure chance. Instead, choose to focus on the significant domain you can influence. By making informed, consistent choices that build a resilient inner terrain, you are no longer a passive recipient of luck. You become an active participant in your own long-term health. Start that journey today.
Ready to take your first step toward empowered understanding? Download your free copy of “Cancer Is No Coincidence – The Missing Link” now.
FAQ
Q: If I have a family history of cancer, does that mean it’s just “bad luck” and inevitable for me?
A: Not at all. A family history means your baseline risk may be higher, but it is not a destiny. It means the proactive steps of lifestyle and screening are even more important for you. It’s a signal to be more vigilant and work closely with your doctor, not a reason to give up hope or agency.
Q: Does stress really cause cancer?
A: The direct link between stress and causing cancer is not conclusively proven. However, chronic, severe stress can weaken your immune system over time and may lead to unhealthy coping behaviors (like poor diet or smoking), which are known risk factors. Managing stress is a key part of supporting your overall “inner terrain.”
Q: I’ve lived an unhealthy life in the past. Is it too late for me to make a difference?
A: It is almost never “too late.” The body has a remarkable capacity to heal and respond positively to better care. Quitting smoking, improving your diet, and becoming active provide health benefits at any age and can help reduce future risk and support overall well-being.
Q: Are “superfoods” the answer to preventing cancer?
A: No single food can prevent or cure cancer. The concept of “superfoods” is often sensationalized. The true power lies in your overall dietary pattern—a consistent, long-term habit of eating a wide variety of nutrient-dense, whole foods that support your body’s defenses.
Ressources
- World Cancer Research Fund / American Institute for Cancer Research (WCRF/AICR): The leading global authority on diet, nutrition, physical activity, and cancer prevention. Their Continuous Update Project analyzes global research to provide the most current recommendations.
- National Cancer Institute (NCI): The U.S. government’s principal agency for cancer research and training. Provides comprehensive, peer-reviewed information on all aspects of cancer.
- American Cancer Society (ACS): A nationwide health organization dedicated to eliminating cancer. Excellent resource for prevention guidelines, screening recommendations, and patient support.
- Link: Can Cancer Be Prevented?
- Centers for Disease Control and Prevention (CDC): The U.S. national public health agency. Offers clear, actionable guides on preventable cancers, screenings, and lifestyle factors.
- The “Bad Luck” Study (Tomasetti & Vogelstein, 2015): The original research article in Science that sparked the public discussion on random mutations and cancer risk.
Disclaimer: The content provided on HealthySimo, including this article and all linked resources, is for educational and informational purposes only. It is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read here. Reliance on any information provided by HealthySimo is solely at your own risk.
About the author
Max Wild is a health writer and researcher focused on cancer awareness, prevention, and patient education. He translates complex medical topics into simple, practical guidance so readers can have more informed conversations with their doctors.

