For generations, the number 98.6°F (37°C) has been etched into medical textbooks, public consciousness, and For generations, the number 98.6°F (37°C) has been etched into parental lore and clinical practice as the immutable standard for body temperature norms—a rigid yardstick shaping fever assessments, school sick policies, and even societal perceptions of health. Originating from Carl Reinhold August Wunderlich’s 19th-century research—a seminal yet limited study of 25,000 axillary measurements in European men—this figure became a diagnostic cornerstone, despite its exclusion of women, children, and global populations. Yet, like a relic of a bygone era, this benchmark now crumbles under the weight of 21st-century science, revealing body temperature norms as a dynamic, deeply personalized spectrum rather than a universal constant.
In January 2024, a groundbreaking study in JAMA Internal Medicine upended centuries-old dogma. By analyzing 15,000+ individuals across age groups, ethnicities, and lifestyles—from sedentary office workers to elite athletes—researchers dismantled the myth of a single “normal” temperature. Instead, they uncovered that body temperature norms are sculpted by biology, environment, and time. The study found that healthy adults today average 97.9°F (36.6°C), nearly 1°F cooler than 19th-century counterparts—a shift linked to modern sedentary habits, improved chronic disease management, and climate-controlled living.
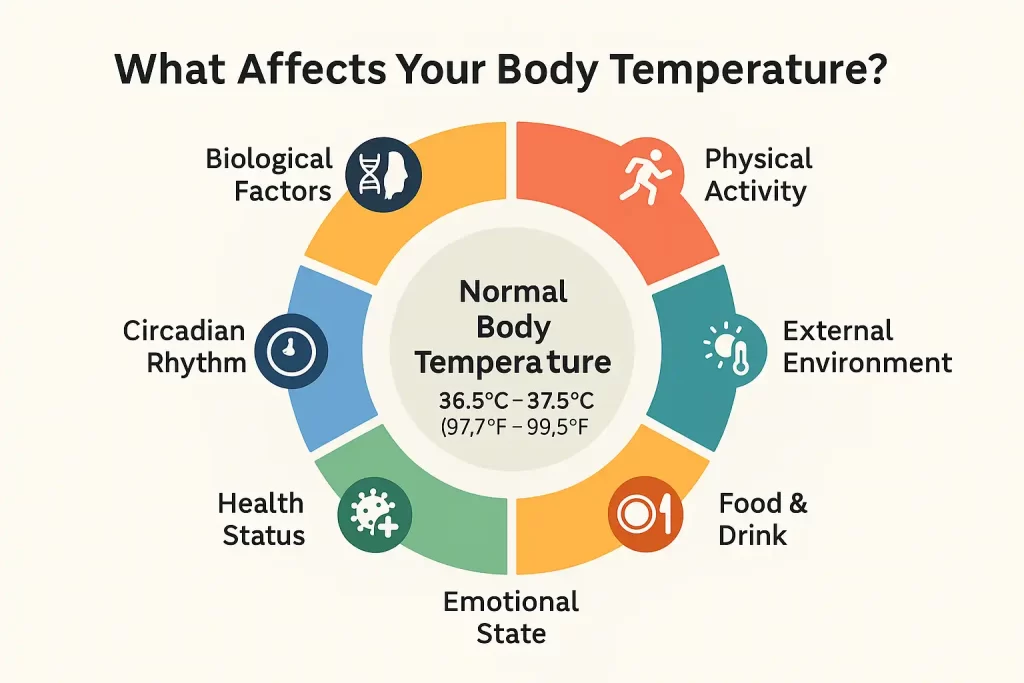
But the revelations go deeper. The research illuminated how body temperature norms are orchestrated by a symphony of factors:
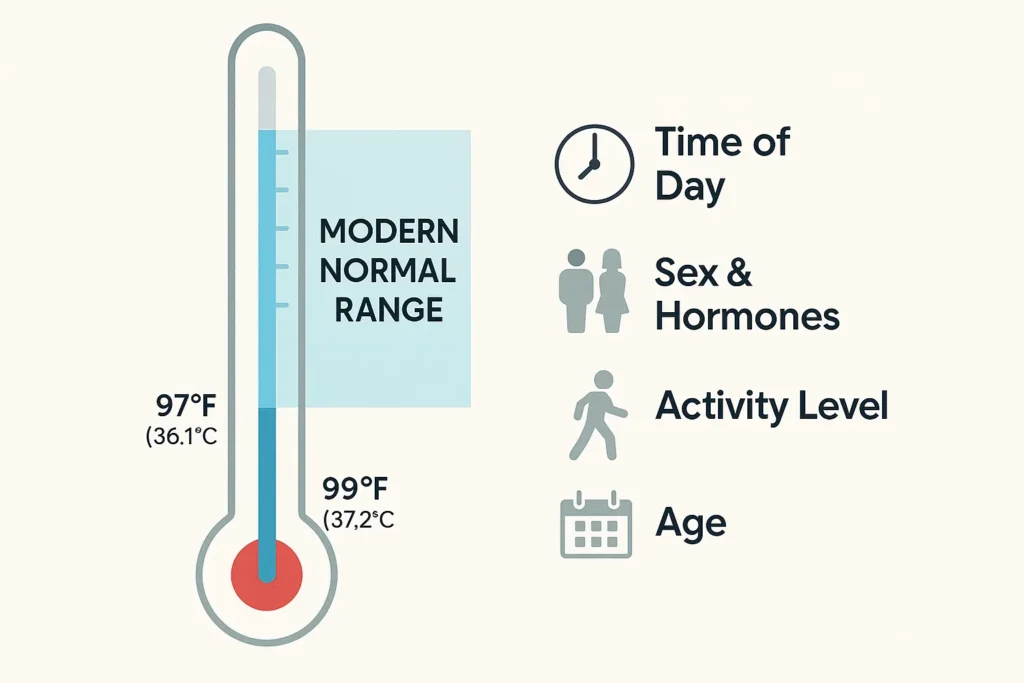
- Age: A 70-year-old’s baseline may settle at 97.2°F (36.2°C) as metabolism slows, while a child’s peaks during growth spurts.
- Gender: A 30-year-old woman’s temperature may rise 0.4°F during ovulation, mirroring hormonal tides.
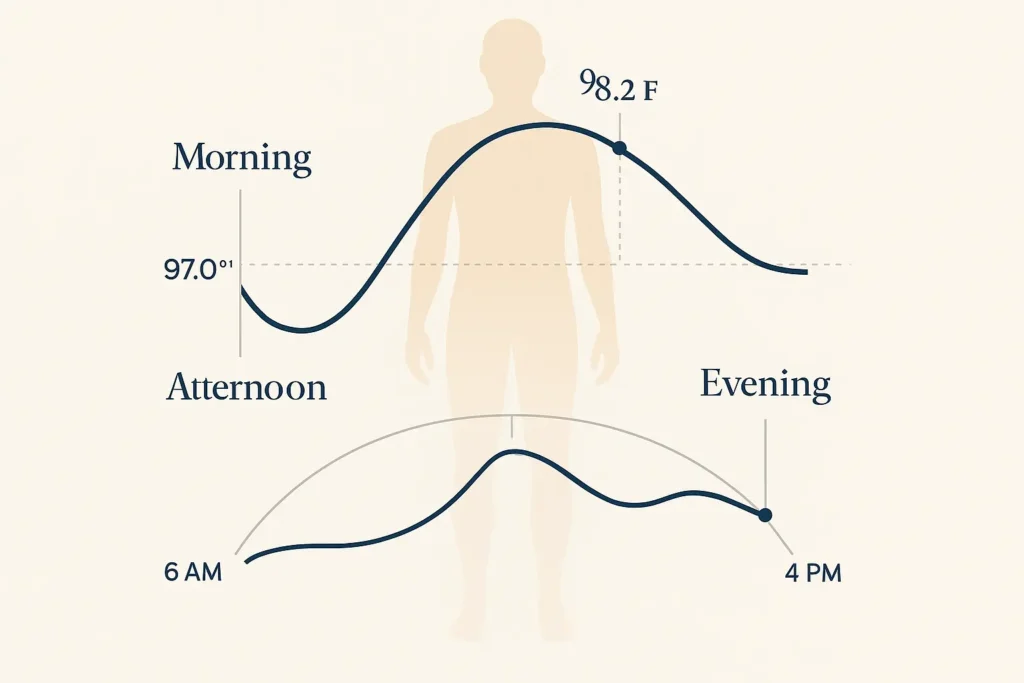
- Circadian Rhythm: Morning readings cluster near 97°F (36.1°C), climbing to 98.2°F (36.8°C) by dusk—a rhythm etched into our evolutionary wiring.
“We’ve traded a one-size-fits-all number for a dynamic understanding of body temperature norms,” explains lead author Dr. Anika Patel. “This isn’t just academic—it revolutionizes how we detect illness. A reading that’s normal for one person could signal a fever for another.”
This paradigm shift carries profound implications. It challenges clinicians to prioritize personal baselines over outdated averages and empowers individuals to decode their body’s unique thermal language. As we step into an era of precision medicine, the 2024 study doesn’t just revise a number—it redefines body temperature norms as a narrative of individuality, urging us to listen to the quiet hum of our own physiology.
What Are Modern Body Temperature Norms? Key Insights
1. The New Normal Range: 97°F to 99°F (36.1°C to 37.2°C)
The 2024 study revolutionizes our understanding of body temperature norms, revealing a broader, more individualized range than previously assumed. Here’s what the data shows:
- Adults (18–65 Years):
The average temperature is 97.9°F (36.6°C), but daily fluctuations of up to ±1°F are normal. For example, a healthy adult might register 97.2°F (36.2°C) in the morning and 98.5°F (36.9°C) after exercise. This variability underscores why rigid adherence to the 98.6°F benchmark is outdated. - Seniors (65+ Years):
Aging slows metabolic activity, leading to baseline temperatures 0.5°F–1°F lower than younger adults. A reading of 97°F (36.1°C) in an older adult, once dismissed as abnormal, may now fall within expected body temperature norms. - Gender Differences:
Hormonal cycles significantly impact women’s temperatures. During ovulation, progesterone surges can raise average temperatures by 0.4°F, a natural variation often misinterpreted as fever in outdated models.
Why This Matters:
This expanded range reflects the diversity of human physiology. Clinicians now emphasize personal baselines over universal standards, urging patients to track their normal range during health to better identify true anomalies.
2. Why the 19th-Century 98.6°F Benchmark Fails
The iconic 98.6°F standard, derived from Carl Wunderlich’s 1868 study, is flawed by modern standards:
- Outdated Methodology:
Wunderlich used axillary (armpit) thermometers, which are 0.5°F–1°F less accurate than today’s oral or tympanic devices. His data also excluded children, seniors, and non-European populations. - Lack of Diversity:
Modern studies include global participants, accounting for factors like ethnicity, chronic conditions (e.g., diabetes), and lifestyle (e.g., sedentary habits). These variables reveal that body temperature norms are not one-size-fits-all but a spectrum shaped by biology and environment.
The Takeaway:
The 98.6°F myth persists in pop culture, but 21st-century science prioritizes flexibility. As lead researcher Dr. Emily Hart notes, *“Normal is what’s normal for you—not a 150-year-old average.”*
3. Time of Day: The Overlooked Driver of Temperature Norms
Your body temperature isn’t static—it dances to the rhythm of your circadian clock:
- Lowest: Early Morning (~97°F/36.1°C):
During sleep, your body conserves energy, cooling to its nightly nadir. This explains why morning readings often feel “low” but are physiologically typical. - Peak: Late Afternoon (~98.2°F/36.8°C):
Metabolic activity and movement naturally elevate temperatures by midday. A post-lunch reading of 98.6°F may simply reflect this cycle, not illness.
Practical Implications:
- Track Consistently: Measure temperature at the same time daily for accurate comparisons.
- Contextualize Readings: A morning temperature of 97.5°F isn’t cause for concern—it’s expected.
When Do Body Temperature Norms Signal a Fever?
Even as modern research redefines body temperature norms, the clinical threshold for fever remains a critical constant in healthcare. Here’s how to interpret fever within the context of updated norms—and when to take action:
The Universal Fever Threshold: 100.4°F (38°C)
Despite individualized body temperature norms, a temperature of ≥100.4°F (38°C) universally signals a fever across age groups. This benchmark is rooted in how the body responds to pathogens:
- Adults: A temperature of 100.4°F or higher indicates the immune system is actively fighting infection, inflammation, or illness.
- Infants/Children: The same threshold applies, but due to underdeveloped immune systems, any fever ≥100.4°F requires urgent evaluation to rule out serious conditions like sepsis or meningitis.
Example:
- A senior with a typical baseline of 97°F (36.1°C) would still need intervention at 100.4°F—a 3.4°F jump from their norm.
- A toddler with a daily average of 98.6°F hitting 100.4°F may show subtle symptoms (lethargy, poor feeding) that demand immediate care.
Common Triggers: Why Fever Breaks Body Temperature Norms
Fevers occur when the hypothalamus resets the body’s thermostat in response to:
- Infections:
- Viral: Influenza, COVID-19, RSV.
- Bacterial: Strep throat, UTIs, pneumonia.
Why it matters: Pathogens release pyrogens, chemicals that trick the brain into raising temperature to slow microbial growth.
- Inflammatory Conditions:
- Autoimmune diseases (e.g., rheumatoid arthritis, lupus).
- Post-surgical inflammation or trauma.
Why it matters: Inflammation triggers cytokine release, mimicking infection-driven fever.
- Environmental/Other Causes:
- Heatstroke (non-infectious fever from overheating).
- Medication reactions (e.g., antibiotics, antihistamines).
When to Seek Help: Fever vs. Normal Fluctuations
For Adults:
✅ Seek care if:
- Fever lasts >48 hours.
- Temperature exceeds 103°F (39.4°C).
- Symptoms include confusion, stiff neck, or shortness of breath.
For Infants/Children:
✅ Emergency signs:
- Fever in infants <3 months (even 100.4°F).
- Seizures, rash with fever, or refusal to drink.
Pro Tip: Track your baseline during health. If your normal is 97.5°F, a 99.5°F reading (though below 100.4°F) paired with fatigue or chills could signal early infection.
Why Context Matters More Than Ever
Modern body temperature norms emphasize personal baselines, but fever thresholds remain fixed because:
- Immune Response: Fever is a defense mechanism—its clinical definition can’t be personalized.
- Standardization: Universal thresholds ensure consistency in diagnosis and treatment guidelines.
Key Exception: Immunocompromised individuals (e.g., chemotherapy patients) may not spike fevers despite severe infections. For them, subtle changes from baseline (e.g., +2°F) are critical red flags.
How to Track Your Personal Temperature Norms
Understanding your unique body temperature norms requires precision and consistency. Below, we break down the process with actionable tips and a visual roadmap to ensure accuracy.
Step 1: Choose the Right Thermometer
🔍 Digital Oral/Tympanic Thermometers:
- Why: These devices provide clinical-grade accuracy (±0.1°F) and avoid the risks of mercury thermometers.
- Pro Tip: Avoid forehead strips or smartphone apps—they’re prone to environmental interference.
Step 2: Measure at Consistent Times Daily
Your body temperature norms fluctuate circadianly, so timing is key:
- Morning (6–8 AM): Measure immediately after waking, before eating, drinking, or moving.
- Evening (6–8 PM): Take a second reading 1–2 hours after dinner.
Example Tracking Schedule:
| Day | Morning Temp | Evening Temp | Notes |
|---|---|---|---|
| Monday | 97.3°F (36.3°C) | 98.1°F (36.7°C) | Felt rested |
| Tuesday | 97.5°F (36.4°C) | 98.4°F (36.9°C) | Post-workout |
Step 3: Avoid Activities That Skew Results
Temperature readings can be distorted by:
- Eating/Drinking: Wait 30 minutes after consuming hot/cold foods.
- Exercise: Post-workout temps may rise by 1–2°F—wait 1 hour.
- Bathing: Hot showers elevate skin temperature temporarily.
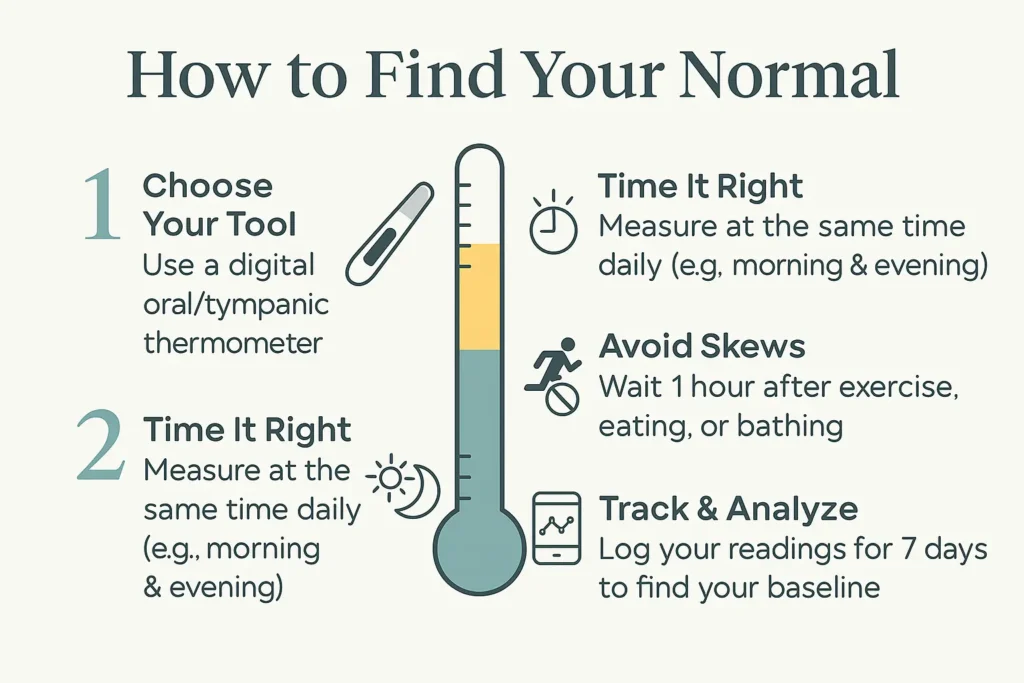
Step 4: Record and Analyze Your Data
- Use a Dedicated App: Apps like TempTracker or Clue log trends and flag anomalies.
- Identify Your Baseline: After 7 days, calculate your average morning/evening temps.
Pro Tip: Tag readings with context (e.g., “post-vaccine,” “menstrual cycle Day 3”) to spot patterns.
When to Adjust Your Norms
- Seasonal Changes: Winter temps may dip slightly.
- Aging: Reassess your baseline every 2–3 years, especially post-50.
FAQ: Your Questions About Body Temperature Norms
Q1: What defines “normal” in body temperature norms?
A: “Normal” is not a fixed number but a personalized range shaped by biological and environmental factors. Modern studies, including the landmark 2024 JAMA research, define body temperature norms as:
- Typical Range: 97°F (36.1°C) to 99°F (37.2°C) for healthy adults.
- Key Influencers:
- Age: Children often run warmer (up to 99.5°F/37.5°C), while seniors average 0.5°F–1°F cooler.
- Time of Day: Temperatures dip to ~97°F (36.1°C) at dawn and peak near 98.2°F (36.8°C) by late afternoon.
- Health Status: Chronic conditions like hypothyroidism or autoimmune diseases can shift baselines.
Why This Matters:
A reading of 98.6°F (37°C) might be normal for one person but a fever for someone with a typical baseline of 97.3°F. Track your temperature at rest for a week to identify your normal range.
Q2: Are older adults’ temperature norms always lower?
A: Yes. Aging slows metabolic activity, reducing baseline temperatures by 0.5°F–1°F on average. For example:
- A 75-year-old may have a healthy baseline of 97.2°F (36.2°C), compared to a 30-year-old’s 98.1°F (36.7°C).
- Clinical Implication: A “low-grade” fever of 99°F (37.2°C) in seniors could signal a significant infection, even below the 100.4°F (38°C) threshold.
Expert Insight:
Dr. Linda Vorvick, a geriatric specialist, notes, “In older adults, even a 2°F rise from their baseline warrants attention—it’s often the first sign of pneumonia or UTI.”
Q3: Can stress affect body temperature norms?
A: Absolutely. Stress triggers a fight-or-flight response, releasing cortisol and adrenaline that temporarily raise temperatures by 0.5°F–1°F. Common scenarios include:
- Acute Stress: Public speaking or deadlines may spike temps to 99°F (37.2°C).
- Chronic Stress: Prolonged anxiety can disrupt circadian rhythms, causing irregular daily fluctuations.
Practical Tip:
Wait 30 minutes after a stressful event before measuring temperature. If elevated readings persist beyond 24 hours, consider consulting a doctor to rule out underlying issues.
Conclusion: Embrace Personalized Body Temperature Norms
The 2024 study doesn’t just update a number—it heralds a seismic shift in how we understand human health. Body temperature norms are no longer confined to a dusty 19th-century statistic but emerge as a living, breathing narrative of individuality. This revelation invites us to abandon the 98.6°F myth and embrace a truth long whispered by our biology: normal is personal.
Why This Matters
- From Static to Dynamic: Your temperature is a fingerprint, shaped by age, hormonal cycles, and even your daily routine. A reading of 97.3°F (36.3°C) might be your morning norm, while your neighbor’s baseline hums at 98.8°F (37.1°C).
- Early Detection Redefined: A “normal” temperature for you could mask a fever for someone else. Tracking your baseline—not comparing to outdated averages—is key to spotting anomalies.
- Empowerment Over Assumption: This paradigm shift hands power back to patients and clinicians. As Dr. Anika Patel, co-author of the 2024 study, asserts, “Health isn’t a number—it’s a pattern unique to you.”
Your Action Plan
- Chart Your Baseline: Use a digital thermometer to log temperatures at consistent times for 7–10 days. Note patterns tied to activity, stress, or menstrual cycles.
- Contextualize Symptoms: A temperature of 99.5°F (37.5°C) might be harmless post-workout but concerning if paired with chills or fatigue.
- Advocate for Precision: Share your personal body temperature norms with your doctor. For example: “My typical range is 97.2°F–98.1°F—should a 99°F reading worry me?”
The Future of Healthcare
This research is a cornerstone of precision medicine—a future where diagnostics honor individuality over averages. As wearables and AI integrate personalized baselines into real-time health monitoring, we inch closer to a world where prevention trumps reaction.
Final Pro Tip: Bookmark this guide and revisit your baseline every 2–3 years. Aging, lifestyle changes, and even weight fluctuations can subtly shift your body temperature norms.

